Key Points
-
Explains the uses of anti-platelet drugs.
-
Reports variation in the practice of managing these patients.
-
Suggests there is no high quality evidence on how to best manage patients taking dual anti-platelet medication undergoing dentoalveolar surgery.
Abstract
Objective The optimum management of dual anti-platelet therapy (DAPT) in patients undergoing dentoalveolar surgery is controversial. The lack of guidelines has meant clinicians have been left to manage these cases from specialist advice or past experience. In view of this the British Association of Oral Surgeons (BAOS) membership was surveyed to assess current practice.
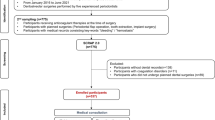
Design An electronic survey consisting of nine closed multiple-choice questions was circulated to all 435 registered BAOS members. A section for open comments was also included. The data was transcribed, organised and reduced to themes by hand and finally analysed.
Results One hundred and eighty members completed the questionnaire giving a response rate of 41%. Ninety-two percent of clinicians had direct involvement in managing patients on DAPT and of these 80% had not encountered a bleeding complication. DAPT was continued for simple dental extraction under local anaesthetic by 83% of respondents and 73% for surgical extractions. Two thirds of the respondents did not follow any guidelines but for those that did the most common was the UK Medicines Information protocols. Only 10% of respondents reported a significant post-operative bleeding complication following surgery in patients on DAPT.
Conclusion This survey confirmed the continued variable management of patients on DAPT undergoing dentoalveolar surgery. Reported bleeding rates were low with over 75% of patients not having their DAPT treatment interrupted.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Nobili A, Garattini S, Mannucci P M . Multiple diseases and polypharmacy in the elderly: challenges for the internist of the third millennium. J Comorbidity 2011; 1: 28–44.
Patel, N, Broadfield, L J, Mellor A C . Medical profile of patients accessing hospital-based emergency dental care. Oral Surg. 2013; 7: 26–32.
Ferrari E, Benhamou M, Cerboni P, Marcel B . Coronary syndromes following aspirin withdrawal: a special risk for late stent thrombosis. J Am Coll Cardiol 2005; 45: 456–459.
George J N, Shattil S J . The clinical importance of acquired abnormalities of platelet function. N Engl J Med 1991; 324: 27–39.
Nizarali N, Rafique S . Special care dentistry: Part 2. Dental management of patients with drug-related acquired bleeding disorders. Dent Update 2013; 40: 711–771.
Lecompte T, Hardy J-F . Antiplatelet agents and perioperative bleeding. Can J Anesth 2006; 53: S103–S112.
Dipyridamole. In Sweetman S C (ed). Martindale: The complete drug reference. 34th ed (electronic version). London: Pharmaceutical Press, 2005. Available online via www.medicinescomplete.com (accessed 7 July 2014).
Merritt J C, Bhatt D L . The efficacy and safety of perioperative anti-platelet therapy. J Thromb Thrombolysis 2002; 13: 97–103.
Clopidogrel (Drug Evauation) Klasco RK (Ed): DRUGDEX® System (electronic version). Thomson Micromedex, Greenwood Village, Colorado U S A. Information available online at http://www.app.dundee.ac.uk/tuith/Static/info/antiplatelet.pdf. (accessed 21 November 2014).
The Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345: 494–502.
COMMIT (Clopidogrel and Metoprolol in Myocardial Infarction Trial) collaborative group. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. The Lancet 2005; 366: 1607–1621.
Gouya G, Arrich J, Wolzt M et al. Antiplatelet treatment for prevention of cerebrovascular events in patients with vascular diseases: a systematic review and meta-analysis. Stroke 2014; 45: 492–503.
Hanna E B . Dual anti-platelet therapy in peripheral arterial disease and after peripheral percutaneous revascularization. J Invasive Cardiol 2012; 24: 679–684.
Myocardial Ischaemia National Audit Project. Information available online at http://www.ucl.ac.uk/nicor/audits/minap (accessed 5 November 2014).
MI–secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction. NICE clinical guideline 172. November 2013. Guideline available online at http://www.nice.org.uk/guidance/cg172 (accessed 5 November 2014).
Brandt J T, Close S L, Iturria S J et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost 2007; 5: 2429–2436.
Ticagrelor for the treatment of actue coronary syndromes. NICE Guidance TA 236. October 2011. Available online at http://publications.nice.org.uk/ticagrelor-for-the-treatment-of-acute-coronary-syndromes-ta236 (accessed 2 July 2014).
Prasugrel for the treatment of acute coronary syndromes with percutaneous coronary intervention. NICE Guidance 182. Available online at http://publications.nice.org.uk/prasugrel-for-the-treatment-of-acute-coronary-syndromes-with-percutaneous-coronary-intervention-ta182 (accessed 5 November 2014).
Miles, M, Huberman A . Qualitative data analysis: an expanded sourcebook. 2nd ed. London: Sage, 1994.
North West Medicines Information Centre. Surgical management of the primary care dental patient on antiplatelet medication, 2007. Available online at http://www.ukmi.nhs.uk/med_info/documents/Dental_Patient_on_Antiplatelet_ Medication.pdf (accessed 2 July 2014).
Lockhart P B, Gibson J, Pond S H, Leitch J . Dental management considerations for the patient with an acquired coagulopathy. Part 1: Coagulopathies from systemic disease. Br Dent J 2003; 195: 439–445.
Grines C L, Bonow R O, Casey D E Jr et al. Prevention of premature discontinuation of dual anti-platelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation 2007; 115: 813–818.
Lillis T, Ziakas A, Koskinas K, Tsirlis A, Giannoglou G . Safety of dental extractions during uninterrupted single or dual anti-platelet treatment. Am J Cardiol 2011; 108: 964–967.
Napeñas J J, Hong C H, Brennan M T, Furney S L, Fox P C, Lockhart P B . The frequency of bleeding complications after invasive dental treatment in patients receiving single and dual anti-platelet therapy. J Am Dent Assoc 2009; 140: 690–695.
Burger W, Chemnitius J M, Kneissl G D, Rücker G . Low-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysis. J Intern Med 2005; 257: 399–414.
Biondi-Zoccai G G, Lotrionte M, Agostoni P et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J 2006; 27: 2667–2674.
Collet J P, Montalescot G, Blanchet B et al. Impact of prior use or recent withdrawal of oral anti-platelet agents on acute coronary syndromes. Circulation 2004; 110: 2361–2367.
Gershlick A H, Richardson G . Drug eluting stents. BMJ 2006; 333: 1233–1234.
Farb A, Boam A B . Stent thrombosis redux – The FDA perspective. N Engl J Med 2007; 365: 984–987.
Acknowledgements
The authors would like to thank the British Association of Oral Surgeons membership for their contribution to the survey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Patel, N., Patel, V., Sarkar, D. et al. Dual anti-platelet therapy and dento-alveolar surgery. How do we manage patients on anti-platelet medication?. Br Dent J 217, E24 (2014). https://doi.org/10.1038/sj.bdj.2014.1055
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bdj.2014.1055