Abstract
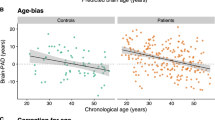
The objective of our study was to elucidate distinct paths to depression in a model that incorporates age, measures of medical comorbidity, neuroanatomical compromise, and cognitive status in a sample of patients with late-life major depressive disorder (MDD) and nondepressed controls. Our study was cross-sectional in nature and utilized magnetic resonance imaging (MRI) estimates of brain and high-intensity lesion volumes together with clinical indices of cerebrovascular and nonvascular medical comorbidity. Neuroanatomic and clinical measures were incorporated into a structural covariance model in order to test pathways to MDD. Our data indicate that there are two paths to MDD; one path is represented by vascular and nonvascular medical comorbidity that contribute to high-intensity lesions that lead to depression. Smaller brain volumes represent a distinct path to the mood disorder. Age influences depression by increasing atrophy and overall medical comorbidity but has no direct impact on MDD. These findings demonstrate that there are distinct biological substrates to the neuroanatomical changes captured on MRI. These observations further suggest that neurobiological mechanisms acting in parallel may compromise brain structure/function, thereby predisposing individuals to clinical brain disorders such as depression.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Alexopoulos GS, Meyers BS, Young RC, Mattis S, Kakuma T . (1993): The course of geriatric depression with “reversible dementia”: A controlled study. Am J Psychiatry 150: 1693–1699
Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Silbersweig D, Charlson M . (1997): Clinically defined vascular depression. Am J Psychiatry 154: 562–565
Alexopoulos GS, Meyers BS, Young RC, Kalayam B, Kakuma T, Gabrielle M, Sirey JA, Hull J . (2000): Executive dysfunction and long-term outcomes of geriatric depression. Arch Gen Psychiatry 57: 285–290
American Heart Association. (1990): Stroke Risk Factor Prediction Chart. Dallas, American Heart Association
American Psychiatric Association. (1994): Diagnostic and Statistical Manual of Mental Disorders (4th Edition). Washington, DC, American Psychiatric Press
Awad IA, Spetzler RF, Hodak JA, Awad CA, Carey R . (1986): Incidental subcortical lesions identified on magnetic resonance imaging in the elderly. I. Correlation with age and cerebrovascular risk factors. Stroke 17: 1084–1089
Blazer D, Hughes DC, George LK . (1987): The epidemiology of depression in an elderly community population. Gerontologist 27: 281–287
Bollen KA . (1989): Structural Equations with Latent Variables. New York, John Wiley & Sons
Borson S, Claypoole K, McDonald G . (1998): Depression and chronic obstructive pulmonary disease: Treatment trials. Seminars in Clinical Neuropsychiatry 3: 115–130
Braffman BH, Zimmerman RA, Trojanowski JQ, Gonatas NK, Hickey WF, Schlaepfer WW . (1988): Brain MR: Pathologic correlation with gross and histopathology. 1. Lacunar infarction and Virchow-Robin spaces. 2. Hyperintense white-matter foci in the elderly. Am J Roentgenol 151: 551–558
Caine ED, Lyness JM, King DA . (1993): Reconsidering depression in the elderly. Am J Geriatr Psychiatry 1: 4–20
Coffey CE, Wilkinson WE, Weiner RD, Parashos IA, Djang WT, Webb MC, Figiel GS, Spritzer CE . (1993): Quantitative cerebral anatomy in depression. A controlled magnetic resonance imaging study. Arch Gen Psychiatry 50: 7–16
Coulehan JL, Schulberg HC, Block MR, Janosky JE, Arena VC . (1990): Medical comorbidity of major depressive disorder in a primary medical practice. Arch Intern Med 150: 2363–2367
Cowell PE, Turetsky BI, Gur RC, Grossman RI, Shtasel DL, Gur RE . (1994): Sex differences in aging of the human frontal and temporal lobes. J Neurosci 14: 4748–4755
Drayer BP . (1988): Imaging of the aging brain. Part I. Normal findings. Part II. Pathologic conditions. Radiology 166: 785–796
Duman RS, Charney DS . (1999): Cell atrophy and loss in major depression. Biol Psychiatry 45: 1083–1084
Emery VO, Oxman TE . (1992): Update on the dementia spectrum of depression. Am J Psychiatry 149: 305–317
Folstein MF, Folstein SE, McHugh PR . (1975): “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189–198
Frasure-Smith N, Lesperance F, Talajic M . (1995): Depression and 18-month prognosis after myocardial infarction [published erratum appears in Circulation 1998 Feb 24:708]. Circulation 91: 999–1005
Gierz M, Jeste DV . (1993): Physical comorbitidy in elderly schizophrenic and depressed patients. Am J Geriatr Psychiatry 1: 165–170
Gould E, Tanapat P, McEwen BS, Flugge G, Fuchs E . (1998): Proliferation of granule cell precursors in the dentate gyrus of adult monkeys is diminished by stress. Proc Natl Acad Sci USA 95: 3168–3171
Hamilton M . (1967): Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6: 278–296
Henderson AS, Korten AE, Jacomb PA, Mackinnon AJ, Jorm AF, Christensen H, Rodgers B . (1997): The course of depression in the elderly: A longitudinal community-based study in Australia. Psychol Med 27: 119–129
Hickie I, Scott E . (1998): Late-onset depressive disorders: A preventable variant of cerebrovascular disease? Psychol Med 28: 1007–1013
Katz IR . (1996): On the inseparability of mental and physical health in aged persons: Lessons from depression and medical comorbidity. Am J Geriatr Psychiatry 4: 1–16
Katz IR, Striem J, Parmelee P . (1994): Psychiatric-medical comorbidity: Implications for health services delivery and for research on depression. Biol Psychiatry 36: 141–145
Kraemer HC, Yesavage JA, Taylor JL, Kupfer D . (2000): How can we learn about developmental processes from cross-sectional studies, or can we? Am J Psychiatry 157: 163–171
Krishnan KR . (1993): Neuroanatomic substrates of depression in the elderly. J Geriatr Psychiatry Neurol 6: 39–58
Krishnan KR, Hays JC, Blazer DG . (1997): MRI-defined vascular depression. Am J Psychiatry 154: 497–501
Kumar A, Miller D, Ewbank D, Yousem D, Newberg A, Samuels S, Cowell P, Gottlieb G . (1997a): Quantitative anatomic measures and comorbid medical illness in late-life major depression. Am J Geriatr Psychiatry 5: 15–25
Kumar A, Schweizer E, Jin Z, Miller D, Bilker W, Swan LL, Gottlieb G . (1997b): Neuroanatomical substrates of late-life minor depression. A quantitative magnetic resonance imaging study. Arch Neurol 54: 613–617
Kumar A, Jin Z, Bilker W, Udupa J, Gottlieb G . (1998): Late-onset minor and major depression: Early evidence for common neuroanatomical substrates detected by using MRI. Proc Natl Acad Sci USA 95: 7654–7658
Kumar A, Bilker W, Jin A . (2000): Atrophy and high intensity lesions: Complementary neurobiological mechanisms in late-life major depression. Neuropsychopharmacology 22: 264–274
Lacro JP, Jeste DV . (1994): Physical comorbidity and polypharmacy in older psychiatric patients. Biol Psychiatry 36: 146–152
Lai TJ, Payne ME, Byrum CE, Steffens DC, Krishnan KR . (2000): Reduction of orbital frontal cortex volume in geriatric depression. Biol Psychiatry 48: 971–975
Linn BS, Linn MW, Gurel L . (1968): Cumulative illness rating scale. J Am Geriatr Soc 16: 622–626
Lopez JF, Chalmers DT, Little KY, Watson SJ . (1998): A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: Implications for the neurobiology of depression. Biol Psychiatry 43: 547–573
Lustman PJ, Griffith LS, Gavard JA, Clouse RE . (1992): Depression in adults with diabetes. Diabetes Care 15: 1631–1639
Lyness JM, Caine ED, Cox C, King DA, Conwell Y, Olivares T . (1998): Cerebrovascular risk factors and later-life major depression. Testing a small-vessel brain disease model. Am J Geriatr Psychiatry 6: 5–13
Mintz J, Dixon W . (1997): Objection overruled: A comment on Gastwirth, Krieger, and Rosenbaum. American Statistician 51: 117–119
Morris P, Rapoport SI . (1990): Neuroimaging and affective disorder in late life: A review. Can J Psychiatry 35: 347–354
Muthen B . (1984): A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika 49: 115–132
National Institutes of Health. (1992): NIH consensus conference. Diagnosis and treatment of depression in late life. JAMA 268: 1018–1024
O'Brien J, Desmond P, Ames D, Schweitzer I, Harrigan S, Tress B . (1996): A magnetic resonance imaging study of white matter lesions in depression and Alzheimer's disease [published erratum appears in Br J Psychiatry 1996 168:792]. Br J Psychiatry 168: 477–485
Parmalee PA, Katz IR, Lawton MP . (1992): Incidence of depression in long term care settings. J Gerontol 47: M189–M196
Penninx BW, Geerlings SW, Deeg DJ, van Eijk JT, van Tilburg W, Beekman AT . (1999): Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry 56: 889–895
Rabins PV, Pearlson GD, Aylward E, Kumar AJ, Dowell K . (1991): Cortical magnetic resonance imaging changes in elderly inpatients with major depression. Am J Psychiatry 148: 617–620
Rajkowska G . (2000): Postmortem studies in mood disorders indicate altered numbers of neurons and glial cells. Biol Psychiatry 48: 766–777
Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, Overholser JC, Roth BL, Stockmeier CA . (1999): Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol Psychiatry 45: 1085–1098
Sapolsky RM, Pulsinelli WA . (1985): Glucocorticoids potentiate ischemic injury to neurons: Therapeutic implications. Science 229: 1397–1400
Sato R, Bryan RN, Fried LP . (1999): Neuroanatomic and functional correlates of depressed mood: the Cardiovascular Health Study. Am J Epidemiol 150: 919–929
Sheline YI . (2000): 3D MRI studies of neuroanatomic changes in unipolar major depression: The role of stress and medical comorbidity. Biol Psychiatry 48: 791–800
Sheline YI, Wang PW, Gado MH, Csernansky JG, Vannier MW . (1996): Hippocampal atrophy in recurrent major depression. Proc Natl Acad Sci USA 93: 3908–3913
Spangler KM, Challa VR, Moody DM, Bell MA . (1994): Arteriolar tortuosity of the white matter in aging and hypertension. A microradiographic study. J Neuropathol Exp Neurol 53: 22–26
Steffens DC, Helms MJ, Krishnan KR, Burke GL . (1999): Cerebrovascular disease and depression symptoms in the Cardiovascular Health Study. Stroke 30: 2159–2166
Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, McGlynn EA, Ware JE Jr . (1989): Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA 262: 907–913
Udupa J, Samarasekera S . (1996): Fuzzy connectedness and object definition: theory, algorithms, and applications in image segmentation. Graphical Models and Image Processing 58: 246–261
Unutzer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W . (1997): Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. A 4-year prospective study. JAMA 277: 1618–1623
Wells KB, Stewart A, Hays RD . (1989): The functioning and well-being of depressed patients: Results from the Medical Outcomes Study. JAMA 277: 1618–1623
Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB . (1991): Probability of stroke: A risk profile from the Framingham Study. Stroke 22: 312–318
Ylikoski A, Erkinjuntti T, Raininko R, Sarna S, Sulkava R, Tilvis R . (1995): White matter hyperintensities on MRI in the neurologically nondiseased elderly. Analysis of cohorts of consecutive subjects aged 55 to 85 years living at home. Stroke 26: 1171–1177
Zubenko GS, Marino LJ Jr, Sweet RA, Rifai AH, Mulsant BH, Pasternak RE . (1997): Medical comorbidity in elderly psychiatric inpatients. Biol Psychiatry 41: 724–736
Acknowledgements
Supported by NIMH grants MH 55115 and MH61567 (AK) and NIMH grant MH 52129 (Clinical Research Center for Depression in Late Life). Presented in Part at the Annual Meeting of the Society for Neuroscience, New Orleans, Oct 2000
STATISTICAL ENDNOTE
The statistical methodology of path analysis remains relatively unfamiliar in the neurosciences. It is an extension of regression analysis that attempts to separate causal influences among a set of variables into direct and indirect (or mediating) pathways. Path analysis makes it possible to model more complex systems than is possible with usual multiple regression models that include only a single dependent variable. Path models typically include intervening variables, often at multiple causal levels, and may omit paths presumed to be irrelevant. Using the methods of structural equation modeling (SEM), overall evaluation of an entire postulated system of causal relations is possible.
Multiple logistic regression analysis, as employed in a previous report of this study (Kumar et al. 2000), evaluates the significance of direct associations from a set of predictor variables to the occurrence of depression. Path analysis, as employed in this report, makes it possible to simultaneously evaluate the statistical plausibility of the entire set of posited causal relationships. As depicted in the main Figure 1, this is a multilevel model that includes both direct and indirect causal paths. The goodness-of-fit χ2 tests the deviation of the data from the model. When significant, it indicates that the data do not fit the posited causal model. Thus, a nonsignificant goodness-of-fit χ2 is desirable, in that it indicates that the posited causal model is statistically plausible in light of the observed data. Of course, the fact that a model is plausible does not guarantee that it is correct. It is not at all uncommon for several alternative models to “fit” the data (as occurred in this case).
The Mplus software makes it possible to simultaneously evaluate multistage models including both continuous and dichotomous dependent variables. In the former case, the path (regression) coefficients are conventional linear regression coefficients, indicating the expected change in the dependent variable for a unit change in the independent variable. In the case of dichotomous dependent variables (e.g., depression in the current analyses), the coefficients are probit coefficients. As such, they represent the change in the probability of “caseness” associated with a unit change in the independent variable. The model underlying the probit portion of the analysis is that the likelihood of observing the outcome (depression in this case) is based on one's position on a hypothetical, unobserved normal curve. The probit equation estimates a linear combination of predictors to predict the z-score representing one's position on that curve and thus the probability of being a case.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, A., Mintz, J., Bilker, W. et al. Autonomous Neurobiological Pathways to Late-Life Major Depressive Disorder: Clinical and Pathophysiological Implications. Neuropsychopharmacol 26, 229–236 (2002). https://doi.org/10.1016/S0893-133X(01)00331-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1016/S0893-133X(01)00331-1
Keywords
This article is cited by
-
Quantitative Tract-Specific Measures of Uncinate and Cingulum in Major Depression Using Diffusion Tensor Imaging
Neuropsychopharmacology (2012)
-
Temporal Lobe Atrophy and White Matter Lesions are Related to Major Depression over 5 years in the Elderly
Neuropsychopharmacology (2010)
-
Translational Research in Late-Life Mood Disorders: Implications for Future Intervention and Prevention Research
Neuropsychopharmacology (2007)
-
Volumetric brain imaging studies in the elderly with mood disorders
Current Psychiatry Reports (2006)
-
Vascular depression: Recent advances
Current Psychosis and Therapeutics Reports (2004)