Summary:
Although follicular lymphoma (FL) is generally responsive to conventional-dose chemotherapy, improved survival in patients with this disease has been difficult to demonstrate. High-dose chemo/radiotherapy followed by autologous stem-cell transplantation (ASCT) can improve response rates, although its effects on survival remain controversial. Between 1990 and 2003, we transplanted 49 patients with low-grade FL at our institution. Twenty-two patients (45%) had undergone histologic transformation at the time of ASCT. In all, 44 patients (90%) had relapsed disease and five patients (10%) were resistant to chemotherapy at the time of transplantation. After ASCT, 30 patients (61%) were in complete remission (CR). The median overall survival (OS) has not been reached, while the median event-free survival (EFS) is 2.4 years. At a median follow-up of 5.5 years (longest 12.4 years), a plateau has been reached with 56% of patients remaining alive, and 35% event-free. ASCT was well tolerated except for two (4%) treatment-related deaths. In multivariable analysis, CR after ASCT and age less than 60 years are the best predictors of EFS and OS. ASCT is thus a safe therapeutic approach in FL, resulting in long-term EFS and OS for some patients, even with transformed disease.
Similar content being viewed by others
Main
Follicular lymphoma (FL) represents the second most frequent subtype of non-Hodgkin's lymphoma. The WHO classification recognizes three grades of disease, according to the number of large cells and the pattern of involvement.1 Limited-stage, grade 1 or 2 FL may be cured with radiotherapy alone2 but advanced-stage disease, which is present in more than 80% of patients, has been traditionally considered incurable. The natural history of advanced-stage FL is characterized by repeated chemosensitive relapses of progressively shorter duration and ultimately death from progressive disease. Thus, even though outcomes may be improving with the introduction of monoclonal antibody therapy, conventional chemotherapy has no impact on overall survival (OS), which remains a median of 8–10 years from diagnosis.3 Additionally, 30–70% of patients undergo histologic transformation to a more aggressive lymphoma,4, 5 with limited treatment options and historically inferior outcomes with conventional-dose therapy.3
High-dose therapy with autologous stem-cell transplantation (ASCT) represents an alternative treatment option for advanced-stage FL. Prior studies have shown that this approach can increase the depth and duration of response in selected patients, although follow-up in most instances has been short vis-à-vis the natural history of FL. Furthermore, this benefit comes at the cost of potentially significant immediate and long-term toxicity, especially for a disease that can be managed for long periods of time with ‘watchful waiting’ or conventional therapies. Prior studies also present conflicting results on the impact of histologic transformation on clinical outcomes. In this paper, we review a single institution experience with ASCT in patients with low-grade FL and identify a group of long-term event-free survivors, even among patients with transformed disease.
Patients and methods
Clinical characteristics
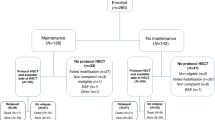
Clinical data were retrospectively collected from all patients with an initial diagnosis of low-grade FL who underwent high-dose chemo/radiotherapy with autologous stem-cell support at our institution between 1990 and 2003. Of the 52 patients identified, three were excluded because of incomplete baseline information. Low-grade FL was defined as the equivalent of FL grade 1 and 2 according to the current WHO classification. At the time of transplantation, 22 (45%) patients had undergone histologic transformation of their disease. Histologic transformation was defined by frequency of large cells or the presence of diffuse architecture, that is, FL grade 3 or diffuse-large B-cell lymphoma based on the WHO classification.
The number of failed therapies included any single-agent or combination chemotherapy, monoclonal antibody, or radiotherapy that was associated with refractory, relapsed, or progressive disease prior to ASCT.
High-dose therapy, stem-cell source, and purging
The choice of high-dose chemo/radiotherapy regimen utilized was mandated by institutional policy at the time (Table 1). Occasionally, substitutions were made at the discretion of the treating physician because of concern for excess toxicity or previous exposure to radiation. Overall, 25 patients (51%) received total body irradiation (TBI) as part of their conditioning therapy, given in the standard anterior–posterior approach.
The choice of stem-cell source was also mandated by institutional policy and reflects the evolving standard of practice. In all, 32 patients (65%) received peripheral stem cells alone, 10 patients (20%) received autologous bone marrow alone, and seven patients (14%) received both peripheral stem-cell and bone marrow grafts. Nine patients (18%) were treated on an institutional bone marrow purging protocol and received 4-hydroxyperoxycyclophosphamide (4-HC) purged bone marrow grafts as previously reported by Bird et al.6
Disease evaluation
Response assessment was performed by the treating physician, using available radiographic, clinical, and histopathologic data. A complete remission (CR) required complete normalization of radiographic and laboratory values, or a biopsy proven remission of any mass that underwent a less than 75% reduction. Chemosensitivity was defined as any response higher than stable disease to the regimen administered most recently before high-dose chemo/radiotherapy. Chemoresistance was defined as stable or progressive disease to the last regimen. Response after transplant was determined approximately 100 days following stem-cell infusion, and regularly thereafter according to physician preference. Disease-free survival (DFS) for patients in CR was measured from attainment of CR after ASCT until the time of disease relapse or disease-related death, with censoring at the time of death unrelated to lymphoma or last follow-up. Event-free survival (EFS) was measured from the day of stem-cell infusion (day 0) until the time of disease progression, development of secondary malignancy, or disease/treatment-related death, with censoring at the time of death unrelated to lymphoma/treatment or last follow-up. OS was measured from day 0 until the date of death, with censoring at the time of last follow-up.
Statistical analysis
Data were collected using retrospective chart and database review. The closing day for analysis was January 31, 2005. All survival distributions and rates were calculated according to the Kaplan–Meier method. Achievement of CR after ASCT was examined in univariable analysis using the χ2 test, and in multivariable analysis using logistic regression. Univariable hazard ratios were derived from the Cox proportional hazards regression model and P-values were calculated for the log-rank test. Multivariable survival analysis was performed to develop predictive models for EFS and OS. As eight of the 10 patients (80%) that received a BM graft had 4-HC purging, the source of stem cells and purging exhibited colinearity (Pearson correlation 0.88). As a result, only one of the two variables was included in multivariable analysis, namely the source of stem cells. We started with a model that included all the variables in Table 3 and serially subtracted the least significant variable using the P-value for the Wald test. The likelihood ratio test was performed after each successive iteration to evaluate the resulting (nested) model. We tested the proportional hazards assumption using -ln(-ln(survival)) vs ln(time) plots (‘log-log plots’) for each variable in the final model and found the assumption to be acceptable. All P-values are two-tailed. Statistical analysis was performed with the STATA software (STATA Corporation v.8, Research Park, TX, USA, 2003).
Results
In total, 49 patients with an initial diagnosis of low-grade FL underwent high-dose chemo/radiotherapy with ASCT at our institution between 1990 and 2003. Their clinical characteristics are listed in Table 2. Median age was 50 years (range: 29–65 years) with five patients 60 years or older. At initial diagnosis, 27 patients (55%) had FL grade 1 and 22 patients (45%) had FL grade 2 by WHO criteria. At the time of transplantation, 22 patients (45%) had disease with histologic transformation. Five patients (10%) received ASCT as consolidation after first-line therapy, 24 patients (49%) after second-line, 11 patients (22%) after third-line, and nine patients (18%) after fourth-line or later therapy (Table 2). At the time of transplantation, 44 patients (90%) had chemosensitive disease with 20 patients (41%) in CR. Five patients (10%) had chemoresistant disease prior to ASCT (Table 2). Among patients alive at the last evaluation, the median follow-up was 5.5 years (range: 0.7–12.4 years).
Event information was missing in two patients. For the 47 patients with event data available, the median EFS was reached at 2.4 years. However, EFS reached a plateau at 35% after 5 years (Kaplan–Meier estimate), with 10 patients remaining alive and event-free at last follow-up (Figure 1a). The median OS has not yet been reached, with a plateau of the Kaplan–Meier curve at 56% (longest follow-up 12.4 years) (Figure 1b).
Following ASCT, 30 patients (61%) were in CR. Among the response subgroups, 28 of the 44 (64%) patients with chemosensitive disease and two of the five (40%) patients with chemoresistant disease were in CR after ASCT. Of note, 18 of the 20 (90%) patients in CR prior to ASCT remained in CR after ASCT. Of the patients in CR after ASCT, the DFS has reached a plateau at 56% with a median follow-up of 6.0 years (range: 0.25–12.1 years) (Figure 1c).
There was one (2%) treatment-related death secondary to sepsis within 100 days after ASCT. Additionally, one patient (2%) who had failed first-line anthracycline-based chemotherapy (CHOP) and received a TBI-containing conditioning prior to transplantation developed myelodysplastic syndrome (MDS) 9 months after ASCT and expired 37 months later while in CR from his lymphoma.
In univariable survival analysis, age less than 60 years, 4-HC purging of the graft, and achievement of CR after ASCT are significantly associated with favorable EFS and OS (Table 3). Additionally, the presence of transformed disease prior to ASCT is significantly associated with inferior OS but not EFS in this group (Table 3). A bone marrow vs a peripheral stem-cell graft is significantly associated with improved EFS but not OS (Table 3). In multivariable analysis, age less than 60 years and achievement of CR after ASCT are the best predictors of EFS and OS (Table 4). Among patients who achieved a CR after ASCT, the DFS, EFS, and OS curves have reached a plateau at 56, 54, and 79%, respectively (Figure 2).
For the 22 patients with transformed disease at the time of ASCT, the median EFS and OS are 1.4 years (range: 0.16–8.2 years) and 4.6 years (range: 0.24–12.4 years), respectively. In all, 11 patients in this subgroup (50%) achieved a CR after transplantation. The CR rate is not significantly different from that in patients without histologic transformation (P=0.10). Age less than 60 years and achievement of CR remain the best predictors of EFS and OS in this subgroup with hazard ratios that are comparable to those of the entire cohort (Table 4). Among patients with transformed disease who achieve a CR, the rates of DFS, EFS, and OS at 5 years are 52, 44, and 80%, respectively, and compare favorably to those for complete responders in the entire cohort, which are 56, 54, and 84%, respectively.
Discussion
FL is an indolent disease, generally considered incurable in advanced stages with conventional therapy. Although high-dose chemo/radiotherapy with stem-cell support has been shown to improve the depth and duration of response, long-term follow-up information is limited. In this retrospective review of a single-institution experience with mostly relapsed low-grade FL, we have identified a group of patients (35% of our cohort) that remain long-term event-free survivors.
In this study, with a median follow-up of 5.5 years, DFS, EFS, and OS at 5 years were 56, 35 and 70%, respectively. These rates are comparable to those observed in other single-institution trials that used various sources of stem cells, purging techniques, and chemo/radiotherapy conditioning regimens. In patients with relapsed disease, previously published studies with a median follow-up of 4 years or longer have reported progression-free survival rates of 38 to 72% and DFS rates (among complete responders) of 31 to 63%. OS rates in these studies range between 55 and 81%.7, 8, 9, 10, 11, 12, 13 A randomized phase III trial sponsored by the EBMTR that was closed prematurely reported a significant prolongation of both progression-free and OS with purged or unpurged ASCT compared to chemotherapy alone in this group of patients.14 The progression-free survival at 2 years for patients receiving purged ASCT, unpurged ASCT, and chemotherapy was 55, 58, and 26%, respectively. OS at 4 years for the purged ASCT, unpurged ASCT and chemotherapy alone arms was 77, 71, and 46%, respectively.14 The data are still relatively immature and need to be observed over longer follow-up.
In our study, the only statistically significant predictors of long-term EFS and OS by multivariable analysis are age less than 60 years and achievement of CR after ASCT. Although there were only five patients over the age of 60 in our study, this variable was found to be statistically significant on both EFS and OS by univariable as well as multivariable analysis. It is important to note that CR prior to transplantation was not predictive of prolonged EFS or OS in our study. It is rather the quality of the response after ASCT that is more significant than any response prior to ASCT. This is confirmed by recent evidence that a molecular remission by PCR after ASCT is a predictor of long-term outcomes over and above a conventional CR.9, 10, 15, 16
Information on the effectiveness of high-dose chemo/radiotherapy and ASCT in patients with histologic transformation is more limited. There were no such patients included in the randomized phase III trial of ASCT in patients with relapsed disease.14 There are small single-institution studies in the literature that have included patients with histologic transformation with conflicting results. Heterogeneity among these studies in terms of eligibility criteria, the definition of transformation, and the timing of ASCT in the course of disease (lead time bias), may explain some of the variability. Early studies have suggested that these patients have a lower EFS and OS compared to patients with low-grade disease.17, 18 Several later studies with limited numbers of patients have not shown a difference in outcomes, potentially secondary to inadequate power.11, 12, 16, 19, 20 Only one study of 50 patients with transformed disease demonstrated no difference in outcomes indirectly, comparing the patients to historical controls with de novo follicular or de novo large cell lymphoma.21 In our cohort of 49 patients, among whom 22 had transformed disease, histologic transformation was not a statistically significant predictor of OS or EFS by multivariable analysis. Furthermore, complete response after ASCT and age younger than 60 years remained the best predictors of EFS and OS in this subgroup. Among complete responders, the 5-year OS, EFS, and DFS rates are comparable to those for the entire cohort.
High-dose therapy followed by autologous stem-cell transplantation was relatively well tolerated by our moderately pretreated patient population with FL. Treatment-related mortality (TRM) within 100 days of ASCT was low at 2%. In other studies with high-risk or transformed patients, early TRM rates as high as 20% have been reported.20 The incidence of secondary malignancies, specifically MDS, was 2%. A reason for the low rates of early TRM and secondary malignancies may be the low utilization of TBI compared to the other studies. In the study by Van Besien et al7 in the ABMTR/IBMTR registries, TBI was associated with a lower risk of disease recurrence, but a higher risk of TRM. In several smaller studies that uniformly incorporated TBI in the conditioning regimen, 12–16% of patients developed MDS/AML or other secondary malignancies.9, 10, 11 We did not observe a statistically significant benefit in survival measures by the incorporation of TBI in our patient cohort. The high risk of late complications and the conflicting information on disease benefit suggest that TBI may be omitted from high-dose therapy regimens in patients with low-grade FL, in accordance with the practice for aggressive lymphomas. On the other hand, incorporation of targeted radiation approaches to ASCT, as with radioimmunoconjugates, has shown promise in phase I trials22, 23 and in a retrospective comparison.24
In summary, high-dose therapy with stem-cell transplantation can result in long-term EFS and OS, even among patients with histologic transformation. In univariable and multivariable analyses, achievement of CR after ASCT is associated with prolonged EFS and OS suggesting that this approach may alter the course of the disease. ASCT was associated with low short-term and long-term toxicity in our group of largely relapsed patients with low-grade FL. These results support the incorporation of high-dose therapy followed by autologous stem-cell transplantation in randomized, controlled clinical trials, especially in comparison to radioimmunotherapy or allogeneic transplantation approaches.
References
Harris NL, Jaffe ES, Diebold J et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting – Airlie House, Virginia, November 1997. J Clin Oncol 1999; 17: 3835–3849.
Sutcliffe SB, Gospodarowicz MK, Bush RS et al. Role of radiation therapy in localized non-Hodgkin's lymphoma. Radiother Oncol 1985; 4: 211–223.
Gallagher CJ, Gregory WM, Jones AE et al. Follicular lymphoma: prognostic factors for response and survival. J Clin Oncol 1986; 4: 1470–1480.
Acker B, Hoppe RT, Colby TV et al. Histologic conversion in the non-Hodgkin's lymphomas. J Clin Oncol 1983; 1: 11–16.
Horning SJ, Rosenberg SA . The natural history of initially untreated low-grade non-Hodgkin's lymphomas. N Engl J Med 1984; 311: 1471–1475.
Bird JM, Luger S, Mangan P et al. 4-Hydroperoxycyclophosphamide purged autologous bone marrow transplantation in non-Hodgkin's lymphoma patients at high risk of bone marrow involvement. Bone Marrow Transplant 1996; 18: 309–313.
van Besien K, Loberiza Jr FR, Bajorunaite R et al. Comparison of autologous and allogeneic hematopoietic stem cell transplantation for follicular lymphoma. Blood 2003; 102: 3521–3529.
Stein RS, Greer JP, Goodman S et al. High-dose therapy with autologous or allogeneic transplantation as salvage therapy for small cleaved cell lymphoma of follicular center cell origin. Bone Marrow Transplant 1999; 23: 227–233.
Freedman AS, Neuberg D, Mauch P et al. Long-term follow-up of autologous bone marrow transplantation in patients with relapsed follicular lymphoma. Blood 1999; 94: 3325–3333.
Apostolidis J, Gupta RK, Grenzelias D et al. High-dose therapy with autologous bone marrow support as consolidation of remission in follicular lymphoma: long-term clinical and molecular follow-up. J Clin Oncol 2000; 18: 527–536.
Berglund A, Enblad G, Carlson K et al. Long-term follow-up of autologous stem-cell transplantation for follicular and transformed follicular lymphoma. Eur J Haematol 2000; 65: 17–22.
Cao TM, Horning S, Negrin RS et al. High-dose therapy and autologous hematopoietic-cell transplantation for follicular lymphoma beyond first remission: the Stanford University experience. Biol Blood Marrow Transplant 2001; 7: 294–301.
Seyfarth B, Kuse R, Sonnen R et al. Autologous stem cell transplantation for follicular lymphoma: no benefit for early transplant? Ann Hematol 2001; 80: 398–405.
Schouten HC, Qian W, Kvaloy S et al. High-dose therapy improves progression-free survival and survival in relapsed follicular non-Hodgkin's lymphoma: results from the randomized European CUP trial. J Clin Oncol 2003; 21: 3918–3927.
Mahe B, Milpied N, Mellerin MP et al. PCR detection of residual Bcl-2/IgH-positive cells after high-dose therapy with autologous stem cell transplantation is a prognostic factor for event-free survival in patients with low-grade follicular non-Hodgkin's lymphoma. Bone Marrow Transplant 2003; 31: 467–473.
Corradini P, Ladetto M, Zallio F et al. Long-term follow-up of indolent lymphoma patients treated with high-dose sequential chemotherapy and autografting: evidence that durable molecular and clinical remission frequently can be attained only in follicular subtypes. J Clin Oncol 2004; 22: 1460–1468.
Schouten HC, Bierman PJ, Vaughan WP et al. Autologous bone marrow transplantation in follicular non-Hodgkin's lymphoma before and after histologic transformation. Blood 1989; 74: 2579–2584.
Bastion Y, Brice P, Haioun C et al. Intensive therapy with peripheral blood progenitor cell transplantation in 60 patients with poor-prognosis follicular lymphoma. Blood 1995; 86: 3257–3262.
Foran JM, Apostolidis J, Papamichael D et al. High-dose therapy with autologous haematopoietic support in patients with transformed follicular lymphoma: a study of 27 patients from a single centre. Ann Oncol 1998; 9: 865–869.
Chen CI, Crump M, Tsang R et al. Autotransplants for histologically transformed follicular non-Hodgkin's lymphoma. Br J Haematol 2001; 113: 202–208.
Williams CD, Harrison CN, Lister TA et al. High-dose therapy and autologous stem-cell support for chemosensitive transformed low-grade follicular non-Hodgkin's lymphoma: a case-matched study from the European Bone Marrow Transplant Registry. J Clin Oncol 2001; 19: 727–735.
Press OW, Eary JF, Gooley T et al. A phase I/II trial of iodine-131-tositumomab (anti-CD20), etoposide, cyclophosphamide, and autologous stem cell transplantation for relapsed B-cell lymphomas. Blood 2000; 96: 2934–2942.
Vose JM, Bierman PJ, Enke C et al. Phase I trial of iodine-131 tositumomab with high-dose chemotherapy and autologous stem-cell transplantation for relapsed non-Hodgkin's lymphoma. J Clin Oncol 2005; 23: 461–467.
Gopal AK, Gooley TA, Maloney DG et al. High-dose radioimmunotherapy versus conventional high-dose therapy and autologous hematopoietic stem cell transplantation for relapsed follicular non-Hodgkin lymphoma: a multivariable cohort analysis. Blood 2003; 102: 2351–2357.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andreadis, C., Schuster, S., Chong, E. et al. Long-term event-free survivors after high-dose therapy and autologous stem-cell transplantation for low-grade follicular lymphoma. Bone Marrow Transplant 36, 955–961 (2005). https://doi.org/10.1038/sj.bmt.1705178
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bmt.1705178
Keywords
This article is cited by
-
Impact of prior treatment on outcome of transformed follicular lymphoma and relapsed de novo diffuse large B cell lymphoma: a retrospective multicentre analysis
Annals of Hematology (2015)
-
Limited clinical benefit for surveillance PET-CT scanning in patients with histologically transformed lymphoma in complete metabolic remission following primary therapy
Annals of Hematology (2014)
-
Disulfide-stabilized diabody antiCD19/antiCD3 exceeds its parental antibody in tumor-targeting activity
Cellular Oncology (2012)
-
Transformation in Follicular Lymphoma: Biology, Prognosis, and Therapeutic Options
Current Oncology Reports (2012)