Abstract
Pseudoxanthoma elasticum (PXE) is a heritable disorder of the connective tissue. Mutations in the ABCC6 gene could be linked to this disease and, just recently, the c.3421C>T mutation was also associated with a high risk of coronary artery disease. We have now developed new real-time PCR assays for the accurate and rapid determination of the c.3421C>T genotype. Using our new assay, we analyzed the presence of the c.3421C>T mutation in the largest collection of DNA samples from unrelated German PXE patients (n=64) and in a control cohort (n=910). For assay setup, two sets of samples with known genotype for the c.3421C>T mutation were analyzed over a period of 14 days. Results were confirmed by restriction endonuclease mapping, sequence-specific PCR and DNA sequencing. In order to ensure that no further mutations or deletions interfered with the c.3421C>T genotyping, we scanned the exon 24 of the ABCC6 gene by DHPLC and investigated the presence of the ABCC6del23–29 deletion in all patients. The assay has been set up on a group of patients with known genotype and validated on 64 PXE patients. In this group four PXE patients (6.3%) were found to be homozygous and 25 (39.0%) to be heterozygous carriers of the c.3421C>T mutation. The common ABCC6del23–29 deletion, possibly interfering with genotype determination, was searched and excluded. Furthermore, two novel mutations in the ABCC6 gene could be identified in two patients. The novel mutations c.3389C>T and c.3341G>A did not interfere with our new assay. Our new c.3421C>T genotyping assays can be used for the rapid identification of this frequent mutation in PXE patients and of the recently newly proposed cardiac risk factor in young patients with myocardial infarcts of unknown origin.
Similar content being viewed by others
Main
Pseudoxanthoma elasticum (PXE, Groenblad–Strandberg syndrome, OMIM 177850 and 264800) is a heritable disorder of the connective tissue affecting the extracellular matrix of the skin, the eyes, the gastrointestine and the cardiovascular system.1 This disease is characterized by the accumulation of calcified elastic fibers, resulting in skin lesions, hypertension, retinal angioid streaks and myocardial infarcts at a relatively early age. Skin lesions are the most prevalent characteristic of PXE and consist of typical yellowish papules that coalesce into larger plaques of inelastic skin with primary predilection in the flexural sites.2 These lesions are generally the first physical signs of the developing disease, but are more a cosmetic rather than a life-threatening manifestation. Involvement of the eyes is characterized by the appearance of angioid streaks in the retina. Pathological calcification of the elastic lamina in Bruch's membrane in the retina leads to subsequent fractures and to angioid streaks.3 Neovascularization and bleeding from the newly formed vessels may cause varying degrees of visual impairment up to a total loss of central vision. However, total blindness is a rare complication in PXE patients. The involvement of the cardiovascular system is manifested by intermittent claudication, vessel rupture and early myocardial infarcts with increased morbidity and mortality.4 In addition, mitral valve prolapse is a common complication in PXE patients.5 All symptoms of PXE are highly variable, which makes the correct and fast diagnosis of this rare heritable disease very challenging.
Recently, the PXE candidate gene ABCC6 was identified and the first PXE-associated mutations were found.6, 7, 8, 9 The ABCC6 gene consists of 31 exons and encodes a 165-kDa transmembrane protein which is one of the ATP-binding cassette subfamily C transporters, termed multidrug resistance-associated protein (MRP6).10 The function of MRP6, which is predominantly expressed in the liver and the kidneys, remained unknown for a long time. Recent studies have tried to shed light on the transport function of MRP6, which was shown to transport under in vitro conditions the endothelin receptor antagonist BQ12311, 12, 13 and glutathione conjugates such as glutathione S-conjugates leukotriene C4.11, 12 However, it is not yet known which molecules are transported by MRP6 in vivo and, consequently, the pathobiochemical mechanisms of PXE remain to be elucidated.
The first mutations in the ABCC6 gene were identified in the genomic DNA isolated from PXE patients, and comparative family analysis could confirm most of these mutations to be associated with the PXE phenotype.7, 8, 9, 14, 15, 16, 17, 18 A frequent mutation detected in the ABCC6 gene in PXE patients is the nonsense mutation c.3421C>T (p.R1141X), resulting in a truncated protein that lacks the second ATP-binding domain of the native MRP6.7, 8, 9, 19, 20 Another mutation, which is frequently found in American PXE patients, is a large deletion including exons 23–29,17 which also leads to a loss of the second ATP-binding site of MRP6.
PXE is a rare disease with a highly variable phenotype. Furthermore, it is not present at birth and symptoms are often not observed until the middle of the second decade of life. These characteristics complicate its accurate and rapid diagnosis. Several case reports are known where patients were treated for cardiac or angiological problems for many years before PXE was diagnosed.21 The difficulties observed require the development of new diagnostic tools for the fast and reliable diagnosis of PXE. As long as no specific biochemical markers for the determination of the disease activity are available, the analysis of pathogenic mutations by means of modern molecular biological methods is a valuable tool for the diagnosis of PXE.
In this study, we have developed a rapid-cycle PCR method for the accurate and rapid allelic discrimination of the c.3421C>T mutation in the ABCC6 gene. The new DNA assay uses rapid-cycle PCR and mutation detection with melting curve analysis on the LightCycler and the Rotorgene instruments. Mutation detection with melting curve analysis is based on the detection of two adjacent oligonucleotide probes, through which fluorescence labels communicate. One of the probes is a tightly bound anchor probe and the adjacent sensor probe spans the region of the polymorphism. The detection of the mutation is performed by a post-amplification melting curve analysis of the final PCR product. The sequence alteration is detected as a change in the melting temperature of the sensor probe. For a homozygous wild-type sample, a single melting peak is observed; for mixed alleles, two peaks are observed, and for a homozygous mutated sample, a single peak at a temperature different from the wild-type allele is observed. The temperature shift induced by one mismatched base is between 5 and 8°C and is easily detectable.
Using our new method we analyzed the distribution of the c.3421C>T mutation in German PXE patients and blood donors using the largest collection of DNA samples from German PXE patients.
Materials and methods
Collection of DNA Samples
DNA samples were obtained from 64 unrelated German PXE patients and Westphalian blood donors (n=910). Genomic DNA was isolated from 200 μl EDTA-anti-coagulated whole blood and was purified using the QIAamp blood kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. The purified DNA was eluted in 10 mM Tris-HCl, pH 8.0, and was stored at –20°C. If no whole-blood specimens were available, the genomic DNA was isolated from 0.5 ml of blood plasma using the QIAamp blood kit and a batch spin procedure. A PCR amplification using the actin-specific primers 5–Aktin25 (5′-ATCTGGCACCACACCTTCTACAATG-3′) and 3–Aktin25 (5′-CGTCATACTCCTGCTTGCTGATCCA-3′) in a standard reaction mixture was performed for quality control of the DNA isolation. The diagnosis of PXE in all patients was consistent with the reported consensus criteria.22, 23 The status of the PXE patients was determined by the presence of ocular findings and dermal lesions and was histologically confirmed by the observation of calcification in the elastic fibers in skin biopsies after von Kossa staining. The biopsy samples were taken from lesional skin. All members of the study were thoroughly questioned about their personal diseases, organ involvements and their family history by medical specialists. The study cohort comprises 64 unrelated patients with PXE from non-consanguineous families with an apparently autosomal recessive or sporadic mode of inheritance of the PXE phenotype. The study was approved by the Institutional Review Board, and the PXE patients provided informed consent.
c.3421C>T Genotyping through Restriction Fragment-Length Polymorphism (RFLP) Analysis
The RFLP analysis of the c.3421C>T mutation in the ABCC6 gene was performed as described by Struk et al9 with minor modifications. A 322-bp fragment containing the exon 24 sequence was amplified with the primers E24_F (5′-AGGTCTTCTCTGCCCTGGCTCTTC-3′) and E24_R (5′-CTGGAATCCTGTACTTGGGGCTCTC-3′). The reaction mixture contained 75 ng of the isolated genomic DNA, 25 pmol of each primer (Invitrogen, Leek, Netherlands), a 0.25 mM concentration of each dNTP, 50 mM KCl, 10 mM Tris-HCl (pH 8.3), 1.5 mM MgCl2 and 2.5 U of hot-start Taq polymerase (Qiagen, Hilden, Germany) in a final volume of 50 μl. Amplification was carried out by an initial denaturating step at 95°C for 15 min, followed by 40 cycles at 94°C for 1 min, 63°C for 1 min, and 72°C for 1 min, followed by a final extension step at 72°C for 15 min. The PCR products were digested at 55°C with 5 U BseLI (MBI Fermentas, St Leon-Rot, Germany) for 4 h and separated on a 4.0% agarose gel (BMA, Rockland, USA). The 3421C allele yielded 111-, 89-, 54-, 45-, 12- and 11-bp fragments and the 3421 T allele yielded 123-, 89-, 54-, 45- and 11-bp fragments.
c.3421C>T Genotyping Using an Amplification Refractory Mutation System (ARMS-PCR)
For the analysis of the c.3421C>T mutation, an ARMS-PCR assay with sequence-specific oligonucleotide primers was developed. One upper-strand primer E24Up (5′-ACCCCCCGCCCACCTGCT-3′) and two reverse primers (E24LoWt 5′-CAGTGGTCCGGGCATTCC-3′, E24LoMut 5′-CAGTGGTCCGGGCATTCT-3′) were designed with the 3′-ends of the lower primers located at the position of the mutation. For the detection of the c.3421C>T mutation, two PCR reactions were performed for each patient, one with the primers E24Up and E24LoWt and one with E24Up and E24LoMut. The reaction mixture contained 75 ng of the isolated genomic DNA, 25 pmol of each primer, a 0.25 mM concentration of each dNTP, 50 mM KCl, 10 mM Tris-HCl (pH 8.3), 1.5 mM MgCl2 and 2.5 U of hot-start Taq polymerase in a final volume of 50 μl. Amplification was carried out by an initial denaturating step at 95°C for 15 min, followed by 40 cycles at 94°C for 30 s, 52°C for 30 sec and 72°C for 1 min. The 306-bp PCR products were subjected to agarose gel electrophoresis and visualized after ethidium bromide staining. All results were verified by double-strand DNA sequencing.
Analysis of the c.3421C>T Mutation through Rapid-cycle PCR and Hybridization Analysis with the LightCycler
For the detection of the c.3421C>T mutation with the LightCycler (Roche, Mannheim, Germany), primers and hybridization probes were designed using the LightCycler Probe Design Software (Roche). In our assay a 307-bp fragment containing exon 24 of the human ABCC6 gene is amplified from human genomic DNA with the primers E24LCU (5′-CTCCCATCCATCCTTCT-3′) and E24LCL (5′-CCTCGCTACCATACAATATGA-3′). The detection probe (5′-ATTCCGAACCCAGGCCC-3′) covering the nucleotide at position 3421 was 5′-labeled with LightCycler (LC) Red 640 and phosphorylated at the 3′-end (Operon, Cologne, Germay). The corresponding anchor probe (5′-GGCAGCACAGTGGTCCGG-3′) was fluorescein-labeled at the 3′-end (Operon). When the probes hybridize to the same DNA strand internal of the PCR primers, the probes come in close proximity and produce fluorescence resonance energy transfer (FRET). During FRET, a donor fluorophore, which is excited by a LED light source, transfers its energy to an acceptor fluorophore only when positioned in the direct vicinity of the former. The acceptor fluorophore emits light of a longer wavelength, which is measured by the LightCycler system and is used as an internal amplification control. The reaction mixtures (20 μl) were prepared in glass capillaries according to the manufacturer's instructions containing 625 nM of the primers E24LCU and E24LCL, 150 nM of the detection and the anchor probe, 3 mM MgCl2, 300 μM of each dNTP, 50 ng of genomic DNA and 2 μl of the Fast Start Mix (Roche). The cycling conditions included an initial denaturation step at 95°C for 2 min and 40 cycles of 95°C for 1 s, 56°C for 10 s and 72°C for 20 s. Melting curves were generated by denaturating the reaction at 95°C for 20 s followed by heating the samples from 40°C to 90°C with a temperature transition rate of 0.15°C/s with continuous monitoring of fluorescence. The total volume of the reaction mixtures could be successfully reduced to 10 μl without any adaptation of the cycling conditions or any loss of assay sensitivity. For the use of a standard hot-start Taq polymerase (Qiagen) with the c.3421C>T LightCycler assay, the following reaction mixture was used in a total volume of 20 μl: 625 nM of each primer, 150 nM of each probe, 3 mM MgCl2 and 300 μM of each dNTP, 50 ng of genomic DNA, 2 μl of 10 × PCR reaction buffer and 1.25 U of HotStar Taq DNA polymerase. The cycling conditions were not modified apart from prolonging the initial denaturation step at 95°C for 10 min.
c.3421C>T Mutation Analysis Using the Rotorgene Instrument
For the detection of the c.3421C>T mutation on the Rotorgene instrument (LTF, Wasserburg, Germany), the same primer and probes as in the LightCycler assay were used. In comparison to the LightCycler system, the Rotorgene also utilizes the FRET effect of hybridization probes but it does not require the use of glass capillaries. The use of normal PCR reaction tubes offers advantages in a cost-effective assay design, but also requires intensive adaptation procedures of established LightCycler assays. The PCR reaction and the subsequent melting curve protocol were performed in a final volume of 25 μl containing 40 nM of the primer E24LCU, 900 nM of the primer E24LCL, 120 nM of the detection probe, 120 nM of the anchor probe, 4.5 mM MgCl2 and 500 μM of each dNTP. A total of 75 ng of genomic DNA, 2.5 μl of 10 × PCR reaction buffer and 0.75 U of HotStar Taq DNA polymerase (Qiagen) were added. The cycling conditions included an initial denaturation step at 95°C for 5 min and 40 cycles of 95°C for 30 s, 56°C for 30 s and 72°C for 30 s. Melting curves were generated by denaturating the reaction at 95°C for 1 min followed by 30 s at 45°C and then by heating the samples to 75°C with a temperature transition rate of 0.2°C/s with continuous monitoring of fluorescence.
Detection of Other Mutations in Exon 24 of the ABCC6 Gene Using Denaturating High-Performance Liquid Chromatography (DHPLC) Analysis
DHPLC analysis was carried out on an automated HPLC device equipped with a DNA separation column (Wave System, Transgenomic, San Jose, CA, USA). Duplexes for DHPLC analysis were created by mixing PCR products from a healthy subject with the corresponding amplicon of the PXE patients. The wild-type sequence of the normal control was confirmed by double-strand sequencing. PCR products were examined for heteroduplexes by subjecting 2–7 μl of each PCR product to the reaction mixture, which was denatured for 4 min at 95°C and then gradually reannealed by decreasing the sample temperature from 95 to 25°C over a period of 30 min. The PCR products were then separated at a flow rate of 0.9 ml/min by means of a linear acetonitrile gradient. The column mobile phase consisted of a mixture of 0.1 M triethylamine acetate (pH 7.0) with (buffer B) or without (buffer A) 25% acetonitrile. Gradient parameters were determined based on the size and the G–C content of the amplicon. The following program was used for analysis of the exon 24 amplicons: sample loading was performed at 50% buffer B for 0.1 min, followed by a linear gradient using 50–53% buffer B for 0.5 min and followed by another linear gradient using 53–58% buffer B for 3 min and a step using 58% buffer B for 2.4 min. The column was then washed with 90% buffer B for 1 min and equilibrated with 50% buffer B for 1 min prior to loading a new sample. The temperature for the successful resolution of the heteroduplexes was determined by using the DHPLC melting algorithm of the Wavemaker software and running fragment-specific melting curves. These data revealed an optimal temperature of analysis for each melting domain of the amplicon. At least two different temperatures of analysis were used for each fragment. The PCR products that showed heteroduplexes by DHPLC analysis were sequenced. These specimens were then reanalyzed and sequenced using independently isolated DNA of that blood sample in order to avoid genotype misinterpretation due to amplification errors.
DNA Sequence Analysis
DNA sequencing was performed using the Big Dye Ready reaction sequencing kit (Perkin-Elmer, Foster City, USA) and 2.5 pmol of the sequencing primers. One of each primer used for the PCR amplification was used for sequencing. The nucleotide sequence was then established using an ABI Prism 310 capillary sequencer (Perkin-Elmer). Multiple amplicons were subjected to double-strand sequencing to compensate for misreading.
Analysis of the ABCC6del23–29 Deletion Mutation
For the analysis of the large deletion including exons 23–29 in the human ABCC6 gene, a combined PCR assay with two upper-strand primers and a universal lower-strand primer were used. The upper-strand primer Del_E22(2930)_R (5′-CCTGTGGGCGGACGAC-3′) is located in exon 22, whereas the primer Del_In29_R (5′-CGGCATGACTGAAGTGAA-3′) is complementary to an intron 29 sequence which is omitted in the described deletion. The universal lower-strand primer was Del_E30(4387)_F (5′-AGGCGGTGGGCAATGA-3′). The ABCC6del23–29 deletion allele results in a PCR product with a size of 2800 bp when using the primers Del_E22(2930)_R and Del_E30(4387)_F. However, no amplicon is generated when the primers Del_In29_R and Del_E30(4387)_F are used. The wild-type allele leads to a 900-bp PCR product with the primers Del_In29_R and Del_E30(4387)_F and no amplicon with the primers Del_E22(2930)_R and Del_E30(4387)_F under the PCR conditions used (postulated size of PCR product: approximately 19 kbp). For the detection of the ABCC6del23-29 mutation, two PCR reactions were performed for each patient. Genomic DNA from a wild-type blood donor and commercial cDNA from human liver (Clontech, San Diego, USA) were used as controls. The reaction mixture contained 75 ng of the isolated genomic DNA, 25 pmol of each primer, a 0.25 mM concentration of each dNTP, 50 mM KCl, 10 mM Tris-HCl (pH 8.3), 1.5 mM MgCl2 and 2.5 U of hot-start Taq polymerase in a final volume of 50 μl. Amplification was carried out by an initial denaturating step at 95°C for 15 min, followed by 35 cycles at 94°C for 30 s, at the optimal annealing temperature for 30 s and 72°C for 1 min. The annealing temperature was 58°C for the primers Del_In29_R and Del_E30(4387)_F and 65°C for the primer set Del_E22(2930)_R/Del_E30(4387)_F. The PCR products were subjected to agarose gel electrophoresis and visualized after ethidium bromide staining.
Statistical Analysis
Statistical analysis was performed using t-test and Kolmogorov–Smirnoff test where appropriate. The allelic frequencies were estimated by gene counting and scoring. The significance of the difference in the alleles observed between the groups was tested using χ2-analysis. P-values of 0.05 or less were considered significant.
Results
Development of a Reliable and Rapid Assay for c. 3421C>T Genotyping
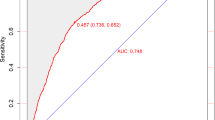
To develop a reliable and rapid genotyping method based on hybridization probe assays, two sequence-specific primers and fluorophore-labeled probes were designed (Figure 1). The homozygous C genotype at position 3421 and the specific hybridization probes form a perfect match, resulting in a melting temperature of about 64.8°C. When the homozygous T genotype is present, one mismatch occurs and the melting temperature is shifted to 55.4°C. Heterozygous genotypes show two melting peaks with the corresponding melting temperatures (Figure 2).
Structure of the MRP6 protein, localization of the mutations and position of the hybridization probes for the detection of the c.3421C>T mutation. (a) Schematic structure of the MRP6 protein and localization of the mutations c.3421C>T (p.R1141X), c.3389C>T (p.T1130 M) and c.3341G>A (p.R1114 H). The predicted topology of MRP6 and the position of the nucleotide binding folds and of the Walker motifs A and B is derived from sequence homology alignments with other MRP transporters and adapted from Le Saux et al.7 The mutations resulting in a change of Thr1130 to Met1130, of Arg1114 to His1114 and the premature stop codon at position 1141 are located in the cytoplasmatic loop between the 15th and the 16th transmembrane domain of MRP6 (magnification). (b) Position and orientation of the fluorophore-labeled hybridization probes for the detection of the c.3421C>T mutation. The localization of the mutation in exon 24 of the ABCC6 gene is indicated by an open box.
Derivative melting curve profiles obtained through rapid-cycle PCR. Melting profiles of representative samples of the three known genotypes at position 3421. (a) Melting peaks obtained with the LightCycler (64.8°C for C allele, 55.4°C for T allele). (b) Melting curves obtained with the Rotorgene are illustrated in panel B (66.6°C for C allele, 56.5°C for T allele). A reliable allelic discrimination was possible in all specimens investigated. The results were verified by sequencing and RFLP analysis. Dotted line, C/C genotype; filled line, C/T genotype; interrupted line, T/T genotype.
In order to develop a c.3421C>T genotyping assay with a broad application range, we also adapted the assay for the Rotorgene instrument. After optimization of the primer and probe concentrations in the reaction mixture, a reliable allelic discrimination with melting temperatures at 66.6 and 56.5°C was possible (Figure 2).
For the determination of the assay characteristics, two sets of 10 evaluation samples containing wild-type, homozygous mutant and heterozygous mutant genotypes were analyzed over a period of 14 days. The intra- and interassay precision of our rapid-cycle assay was 100% with both the LightCycler and the Rotorgene systems. Neither shifts of the hybridization probe melting temperatures nor inaccurate melting curves of individual samples were observed during the whole evaluation period. All results were 100% in concordance with the genotypes determined by restriction endonuclease mapping, sequence-specific primer PCR and DNA sequencing, which were used as comparison methods.
Analysis of the c.3421C>T Mutation in PXE Patients and Blood Donors
The presence of the c.3421C>T mutation was analyzed in apparently unrelated PXE patients (n=64, aged 17–77 years, mean age 46.1±14.3) and healthy controls (n=910, aged 18–65, mean age 39.7±19.3). The patients' characteristics are summarized in Tables 1 and 2. In the PXE patients, four homozygous and 25 heterozygous carriers of the c.3421C>T mutation were found. In the patients' group, no significant correlation between the presence of the c.3421C>T mutation and neither the number of affected organs nor the age of the first PXE diagnosis was observed. Only one of 910 blood donors used as controls carried this ABCC6 gene mutation and the allelic frequency of this mutation in the Westphalian population could be calculated as 0.05%.
Analysis of the ABCC6del23—29 Deletion in the German PXE Cohort
A large deletion in the ABCC6 gene, which was commonly found in PXE patients in the United States, leads to the deletion of exons 23–29. In order to avoid a misinterpretation of the c.3421C>T genotype due to the occurrence of the ABCC6del23–29 mutation, we investigated this deletion with a combined PCR assay as described in the Materials and methods section. None of the PXE patients was found to carry ABCC6del23–29 in either a heterozygous or homozygous state.
Mutation Analysis of Exon 24 of the Human ABCC6 Gene in German PXE Patients
In order to ensure that no further mutations in exon 24 interfered with the accurate interpretation of the c.3421C>T genotyping using the rapid-cycle assay, exon 24 of the ABCC6 gene was scanned by DHPLC in the PXE patients (n=64). The presence of the c.3421C>T mutation in either heterozygous or homozygous state could be reliably detected in all specimens with the DHPLC analysis performed. The retention pattern was found to be specific and reproducible for both the wild-type sequence and the c.3421C>T mutation. Furthermore, DHPLC analysis identified abnormal tracings in two PXE patients. Two novel single-nucleotide substitutions could then be identified in both patients suffering from PXE. The c.3389C>T mutation was present in a homozygous state in one patient and resulted in a substitution of threonine to methionine at position 1130 in the amino-acid sequence of the MRP6 protein. This patient was a 33-year-old female whose eyes and skin were affected by PXE-specific alterations and who was found to be wild type for the c.3421C>T mutation. The second novel mutation was a G → A transition at position 3341, leading to an exchange of Arg1114 to His1114 in the MRP6 protein in a woman, aged 61 years, with eye impairment and skin papules. The c.3341G>A mutation was present in a heterozygous state in this patient, who was identified to be wild type in the c.3421C>T genotyping. Analysis of a blood donor cohort (n=200) revealed that the mutations c.3341G>A and c.3389C>T were not present in normal controls. An alignment of the human MRP proteins using the ClustalW program identified both mutations to alter amino-acid residues which are conserved in the human MRP proteins. Neither novel mutation affected our c.3421C>T rapid-cycle assays as they did not interfere with either the amplification primers or the hybridization probes.
Discussion
In this study, we have developed a rapid-cycle assay for the determination of the c.3421C>T mutation in the ABCC6 gene, which is a frequent mutation found in European PXE patients.15 The standard RFLP assay for the determination of c.3421C>T genotype9 includes a PCR amplification of exon 24 using a block thermocycler followed by a restriction enzyme-mediated digestion of the amplicon and high-resolution gel electrophoresis. The fragments' lengths are then visually analyzed by the investigator after ethidium bromide staining and the c.3421C>T genotype is derived from the occurrence of a specific restriction pattern. Analysis takes 5–6 h, requires a lot of manual interference by the technicians and can hardly be automated. Furthermore, the standard procedure requires open-tube handling of PCR products and is subject to easy contamination by displaced amplicons. Therefore, this assay is not suitable for fast and reliable routine diagnostics. Our rapid-cycle assay with subsequent melting curve analysis is a closed-tube system with a minimized risk of contamination and a low hands-on time, which yields reliable genotyping results within less than 45 min. We could demonstrate that our new assay is easily adaptable to other real-time PCR instruments, as, for example, for the Rotorgene instrument, and that the melting curves were comparable with those obtained with the LightCycler system. The assay precision determined was 100%, with both systems demonstrating a complete reproducibility and stability of our new c.3421C>T genotyping assay.
In order to investigate the validity of our new c.3421C>T genotyping assay, we also scanned the patients' cohort for novel mutations in exon 24 and for the ABCC6del23–29 deletion. Unknown mutations that are located in the binding sites of the hybridization probe might lead to a destabilization of either anchor or sensor probe and to a shift of the melting peak in the melting curve analysis. This is a possible factor for genotype misinterpretation that has to be taken into consideration when designing a versatile rapid-cycle assay suitable for fast routine diagnostics. The ABCC6del23–29 deletion, which was found to be a common mutation in PXE patients from the United States,15 is a 16.5-kb deletion leading to an omission of exons 23–29. In order to avoid misinterpretation of the c.3421C>T genotype due to a loss of at least one exon 24 allele, we analyzed our cohort for the occurrence of the ABCC6del23–29 mutation. No patients were found to carry this deletion in either a heterozygous or homozygous state indicating that this mutation is not frequent in German PXE patients. These results are in accordance with a previous study from Le Saux et al,15 who determined the allelic frequency of the ABCC6del23–29 deletion to be 4.3% in a European and 28.4% in a United States American PXE cohort. However, the absence of the ABCC6del23–29 deletion does not exclude larger deletions on chromosome 16 affecting the whole ABCC6 gene or other smaller deletions. Further haplotype analysis and analysis of first-degree family members would be necessary to exclude other rare genetic disarrangements and deletions. However, other studies have already shown that the investigated ABCC6del23–29 deletion is the only common deletion that was observed in PXE patients.15
Two novel mutations in exon 24 of the ABCC6 gene were identified using DHPLC analysis. Neither mutation is situated in the binding region for the amplification primers and the hybridization probes and, therefore, they do not affect the results of our new c.3421C>T genotyping assay. The c.3389C>T mutation results in a substitution of the hydroxyl amino acid threonine to the hydrophobic amino acid methionine in the intracellular loop between the 15th and the 16th transmembrane domain of the MRP6 protein (Figure 1). This mutation was present in a homozygous state in one patient suffering from PXE and affects an amino-acid residue that is conserved in all human MRP proteins. The second novel mutation c.3341G>A results in a conserved exchange of the basic amino acid arginine to histidine, which also has basic properties. This mutation is also located in the intracellular loop between the 15th and the 16th transmembrane domain of MRP6, affects another residue that is conserved in the human MRP proteins and was present in a heterozygous state in a PXE patient. A G → C mutation leading to a substitution of arginine to proline at the same position of the MRP6 protein was already described to be linked to the PXE phenotype,7 indicating the importance of this position in the amino-acid sequence of MRP6 for this disease.
The secondary structure of the MRP6 protein, which was predicted by sequence homology analysis using similar transporters from the ABC gene family,7 shows this loop to be located near the second nucleotide binding domain and the Walker motif A. The Walker motif A is a conserved motif in ABC-type transporters and was demonstrated to be involved in the ATP hydrolysis necessary for the active transport mechanism.24, 25, 26 Furthermore, some mutations in the ABCC6 gene, such as c.3341G>C or c.3413G>A, which are also linked to the PXE phenotype, have been found to be located in this intracellular loop.7 The c.3421C>T mutation, which was demonstrated to be a frequent mutation in PXE patients in this study, is also positioned in this part of the MRP6 protein. The frequent occurrence of disease-associated mutations in this region of the protein is an indicator for the importance of this loop. However, the crystal structure of the MRP6 protein has not yet been solved. Consequently, further experiments using recombinant MRP6 variants will have to be performed to shed light on the significance of this loop for the biological role of MRP6.
Analysis of the frequency of the 3421 T allele in the blood donor control group revealed this mutation to be a rare variation which was only found in one of 1820 control chromosomes investigated. Trip et al27 recently analyzed the frequency of this c.3421C>T mutation in a Dutch population and found eight heterozygous carriers within their cohort consisting of 2114 control chromosomes. These divergent results indicate the potential need for a population-specific control cohort when analyzing ABCC6 gene mutations and for further investigations on the frequency of the c.3421C>T mutation in different ethnic groups.
In this study, we could demonstrate that the c.3421C>T mutation is a frequent mutation in the ABCC6 gene in German PXE patients and that homozygous carriers all suffer from this disease. Heterozygous carriers of the c.3421C>T mutation were also found in a cohort of not or not yet affected relatives of PXE patients (data not shown). Compound heterozygosity for single-base-pair substitutions in the ABCC6 gene was previously demonstrated by different groups to be associated with the appearance of the PXE phenotype. Therefore, our assay needs to be associated with other mutation screening methods in order to provide a correct diagnosis and appropriate genetic counseling in the patients' families. No significant association between the c.3421C>T genotype and the occurrence of PXE-specific symptoms or organ involvement was possible. This lack of genotype–phenotype connection is in concordance with the results from other studies, where no specific correlation between the PXE phenotype and the type or position of the mutation was found.15 PXE is characterized by a considerable inter- and intrafamilial variability, and future studies should focus on the careful evaluation of environmental factors in order to shed light on the factors that can influence the progression of this disease. This also requires the determination of sequence variations in other genes involved in vessel and connective tissue metabolism, which might serve as modifiers in the onset of the PXE phenotype.
Cardiovascular manifestations are common in PXE patients. Myocardial infarcts occur in PXE patients at a relatively early age,4, 28 probably due to the calcification of the internal elastic lamina of the coronary arteries.29 Just recently, a case–control study in a Dutch population revealed that the c.3421C>T mutation in a heterozygous state is associated with a strong increase in the prevalence of coronary artery disease.27 These results lead us to consider the determination of the c.3421C>T mutation in routine screening for cardiac risk factors. The rapid determination of risk factors is a very important feature for young patients with myocardial infarcts of unknown origin and can be effortlessly performed with our newly developed rapid-cycle assay.
In conclusion, our new c.3421C>T genotyping assays can serve as a valuable diagnostic tool for the rapid and reliable identification of this pathogenic PXE mutation. Furthermore, our method can be easily employed for routine screening of cardiac patients with coronary artery disease and myocardial infarcts of unknown origin.
References
Neldner KH . Pseudoxanthoma elasticum. Int J Dermatol 1988;27:98–100.
Uitto J, Boyd CD, Lebwohl MG, et al. International centennial meeting on pseudoxanthoma elasticum: progress in PXE research. J Invest Dermatol 1998;110:840–842.
Dreyer R, Green WR . The pathology of angioid streaks: a study of twenty-one cases. Trans Pa Acad Ophthalmol Otolaryngol 1978;31:158–167.
Lebwohl M, Halperin J, Phelps RG . Brief report: occult pseudoxanthoma elasticum in patients with premature cardiovascular disease. N Engl J Med 1993;329:1237–1239.
Lebwohl MG, Distefano D, Prioleau PG, et al. Pseudoxanthoma elasticum and mitral-valve prolapse. N Engl J Med 1982;307:228–231.
Cai L, Struk B, Adams MD, et al. A 500-kb region on chromosome 16p13.1 contains the pseudoxanthoma elasticum locus: high-resolution mapping and genomic structure. J Mol Med 2000;78:36–46.
Le Saux O, Urban Z, Tschuch C, et al. Mutations in a gene encoding an ABC transporter cause pseudoxanthoma elasticum. Nat Genet 2000;25:223–227.
Ringpfeil F, Lebwohl MG, Christiano AM, et al. Pseudoxanthoma elasticum: mutations in the MRP6 gene encoding a transmembrane ATP-binding cassette (ABC) transporter. Proc Natl Acad Sci USA 2000;97:6001–6006.
Struk B, Cai L, Zach S, et al. Mutations of the gene encoding the transmembrane transporter protein ABC-C6 cause pseudoxanthoma elasticum. J Mol Med 2000;78:282–286.
Kool M, van der Linden M, de Haas M, et al. Expression of human MRP6, a homologue of the multidrug resistance protein gene MRP1, in tissues and cancer cells. Cancer Res 1999;59:175–182.
Belinsky MG, Chen ZS, Shchaveleva I, et al. Characterization of the drug resistance and transport properties of multidrug resistance protein 6 (MRP6, ABCC6). Cancer Res 2002;62:6172–6177.
Ilias A, Urban Z, Seidl TL, et al. Loss of ATP-dependent transport activity in pseudoxanthoma elasticum-associated mutants of human ABCC6 (MRP6). J Biol Chem 2002;277:16860–16867.
Madon J, Hagenbuch B, Landmann L, et al. Transport function and hepatocellular localization of mrp6 in rat liver. Mol Pharmacol 2000;57:634–641.
Cai L, Lumsden A, Guenther UP, et al. A novel Q378X mutation exists in the transmembrane transporter protein ABCC6 and its pseudogene: implications for mutation analysis in pseudoxanthoma elasticum. J Mol Med 2001;79:536–546.
Le Saux O, Beck K, Sachsinger C, et al. A spectrum of ABCC6 mutations is responsible for pseudoxanthoma elasticum. Am J Hum Genet 2001;69:749–764.
Pulkkinen L, Nakano A, Ringpfeil F, et al. Identification of ABCC6 pseudogenes on human chromosome 16p: implications for mutation detection in pseudoxanthoma elasticum. Hum Genet 2001;109:356–365.
Ringpfeil F, Nakano A, Uitto J, et al. Compound heterozygosity for a recurrent 16.5-kb Alu-mediated deletion mutation and single-base-pair substitutions in the ABCC6 gene results in pseudoxanthoma elasticum. Am J Hum Genet 2001;68:642–652.
Wang J, Near S, Young K, et al. ABCC6 gene polymorphism associated with variation in plasma lipoproteins. J Hum Genet 2001;46:699–705.
Bergen AA, Plomp AS, Schuurman EJ, et al. Mutations in ABCC6 cause pseudoxanthoma elasticum. Nat Genet 2000;25:228–231.
Germain DP, Perdu J, Remones V, et al. Homozygosity for the R1268Q mutation in MRP6, the pseudoxanthoma elasticum gene, is not disease-causing. Biochem Biophys Res Commun 2000;274:297–301.
Araki Y, Yokoyama T, Sagawa N, et al. Pseudoxanthoma elasticum diagnosed 25 years after the onset of cardiovascular disease. Intern Med 2001;40:1117–1120.
Christiano AM, Lebwohl MG, Boyd CD, et al. Workshop on pseudoxanthoma elasticum: molecular biology and pathology of the elastic fibers Jefferson Medical College, Philadelphia, Pennsylvania, June 10, 1992. J Invest Dermatol 1992;99:660–663.
Lebwohl M, Neldner K, Pope FM, et al. Classification of pseudoxanthoma elasticum: report of a consensus conference. J Am Acad Dermatol 1994;30:103–107.
Hung LW, Wang IX, Nikaido K, et al. Crystal structure of the ATP-binding subunit of an ABC transporter. Nature 1998;396:703–707.
Hopfner KP, Karcher A, Shin DS, et al. Structural biology of Rad50 ATPase: ATP-driven conformational control in DNA double-strand break repair and the ABC-ATPase superfamily. Cell 2000;101:789–800.
Diederichs K, Diez J, Greller G, et al. Crystal structure of MalK, the ATPase subunit of the trehalose/maltose ABC transporter of the archaeon Thermococcus litoralis. EMBO J 2000;19:5951–5961.
Trip MD, Smulders YM, Wegman JJ, et al. Frequent mutation in the ABCC6 gene (R1141X) is associated with a strong increase in the prevalence of coronary artery disease. Circulation 2002;106:773–775.
Nolte KB . Sudden cardiac death owing to pseudoxanthoma elasticum: a case report. Hum Pathol 2000;31:1002–1004.
Boutouyrie P, Germain DP, Tropeano AI, et al. Compressibility of the carotid artery in patients with pseudoxanthoma elasticum. Hypertension 2001;38:1181–1184.
Acknowledgements
We thank Alexandra Adam and Anja Reuße-Kaup for excellent technical assistance, Dr Arndt Gröning for help with the statistics and Grainne Delany for linguistic advice. We are very grateful to all the PXE patients and their relatives, whose cooperation made this study possible. Furthermore, we also thank Peter Hof, chairman of the Selbsthilfegruppe für PXE Erkrankte Deutschlands e.V., and the members of the clinical ambulance for PXE at the Bethesda hospital in Freudenberg, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Götting, C., Schulz, V., Hendig, D. et al. Assessment of a rapid-cycle PCR assay for the identification of the recurrent c.3421C>T mutation in the ABCC6 gene in pseudoxanthoma elasticum patients. Lab Invest 84, 122–130 (2004). https://doi.org/10.1038/labinvest.3700004
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/labinvest.3700004
Keywords
This article is cited by
-
Pseudodominante Vererbung von Pseudoxanthoma elasticum
Der Ophthalmologe (2015)
-
Pseudoxanthoma elasticum
Der Ophthalmologe (2006)
-
Elevated xylosyltransferase I activities in pseudoxanthoma elasticum (PXE) patients as a marker of stimulated proteoglycan biosynthesis
Journal of Molecular Medicine (2005)
-
Rapid genotyping for most common TGFBI mutations with real-time polymerase chain reaction
Human Genetics (2005)
-
New ABCC6 gene mutations in German pseudoxanthoma elasticum patients
Journal of Molecular Medicine (2005)