Abstract
uPM3 is the first urine-based genetic test that is highly specific for detecting prostate cancer. The histopathologic characteristics of uPM3-detected cancer in radical prostatectomy specimens have not been previously described. We evaluated a consecutive series of radical prostatectomies to determine the extent, zonal distribution and other features of prostate cancer following uPM3 detection. A total of 24 whole-mounted, totally embedded radical prostatectomy specimens were evaluated. All patients had clinically localized cancer and none received preoperative therapy. Zonal location of cancer, distance to the urethra, cancer volume, Gleason grade and multicentricity were recorded; volume of cancer was measured using the grid-counting method. Patients ranged in age from 43 to 75 years (mean 65 years). In 21/24 cases, cancer involved the transition and peripheral zones and was multicentric (87%). Mean cancer volume was 3.96 cm3 (range 0.08–16.86 cm3). Mean distance to the urethra was 0.50 cm for the closest cancer and 0.61 cm for the most distant cancer. Mean Gleason score was 7 (range 5–9); pathologic stage was pT2 for 17 cases and pT3 for seven cases. The uPM3 is an independent and specific biomarker that detects prostate cancers of similar volume, location, extent and grade as other tests for early detection. uPM3 does not preferentially identify large or aggressive prostate cancers.
Similar content being viewed by others
Main
Prostate carcinoma is the most common visceral cancer in men; it was estimated that in 2005 in the USA 232 090 new cases were diagnosed, and that 30 350 men died of the disease.1 If prostate carcinoma is detected while still limited to its primary site, radical prostatectomy or radiotherapy is in most cases successful in controlling it;2, 3 thus, early diagnosis is a key element in its management.
The specificity of the serum PSA test is not ideal; approximately 20% of men with PSA levels of 2.5–4 ng/ml will have prostatic carcinoma.4, 5, 6 The PSA derivatives, for example, correlations of serum levels with prostatic volume, levels changes over time, and the addition of statistical methods improve the test's specificity but the underlying problems remain essentially unsolved.7, 8, 9 Therefore, it is evident that more specific clinical markers for early prostate cancer are needed.
The PCA3DD3 gene is localized at chromosome 9q21–22; and by Northern blot analysis was noted to be up to 100 times overexpressed in 53/56 prostate cancers while it was not expressed in adjacent noncancerous prostate tissues.10 Moreover, applying the more sensitive reverse transcriptase polymerase chain reaction (RT-PCR), no PCA3DD3 transcripts could be detected in a wide range of human extraprostatic normal and cancerous tissues suggesting that PCA3DD3 is the most specific prostate cancer gene identified to date.11, 12 The PCA3DD3 mRNA includes a high density of stop codons; thus, it does not have an open reading frame resulting in a noncoding RNA.12
The degree of specificity of the PCA3DD3 test makes its incorporation into the prostate cancer diagnostic armamentarium highly desirable; however, quantitative RT-PCR techniques require a complex laboratory infrastructure thus rendering its routine clinical application impractical. Recently, an assay for qualitative simultaneous detection of PCA3DD3 RNA and PSA mRNA as a marker for prostatic cells in urine samples has been introduced; it was designated as NASBA (nucleic acid sequence-based amplification), (uPM3, DiagnoCure, Quebec, Canada).12, 13 Independent studies showed that this test is a very promising adjunct tool for the early diagnosis of prostate cancer.13, 14 In this investigation based on a series of radical prostatectomies, we attempted to determine if results of the uPM3 test may help in predicting tumor size, extent, grade and other parameters in addition to simply detecting the presence of prostate cancer.
Materials and methods
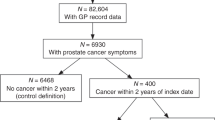
Twenty-four cases were selected from the surgical pathology files of the University of Vienna from patients who had a retropubic radical prostatectomy and bilateral pelvic lymphadenectomy between 2000 and 2003. All carcinomas were limited to the prostate and none had received any preoperative therapy. The uPM3 test had been performed on all patients prior to surgery (Table 1).
All prostate specimens were formalin fixed in their entirety and serially sliced at 5 mm intervals perpendicular to the posterior aspect of the gland. All slices were sequentially and entirely embedded and mounted. For every block, a single complete 5 μm section was cut, stained with hematoxylin and eosin, and examined independently by two pathologists (DGB and JQ). All foci of cancer were outlined directly on each slide, and were considered separate if they were 2 mm or more apart as previously described.15, 16 In addition, all slides from all specimens were examined to ascertain whether or not the mapped carcinoma foci were separate and distinct in deeper and/or superficial sections throughout the prostate. The volume of each focus of carcinoma was calculated by the grid-counting method, and the largest or dominant cancer focus was determined.15, 16
Results
Clinicopathologic data including patients' age, serum PSA, prostate weight, tumor stage and Gleason score, uPM3, tumor volume, tumor distance to the urethra, tumor location and multicentricity are outlined in Table 1.
Patients ranged from 43 to 75 years (mean 65 years). All patients were positive for uPM3 testing. Mean serum PSA was 12.50 ng/ml (range 0.59–27.70 ng/ml). Mean prostate weight was 46 g (range 23–112 g). In 21 cases, prostate cancer involved the transition and the peripheral zones while in the remaining three cases tumor was limited to the peripheral zone. Multicentricity, defined by the presence of two or more independent tumors, was noted in 21/24 cases (88%). Mean cancer volume was 3.96 cm3 (range 0.08–16.86 cm3). Mean distance to the urethra was 0.50 cm for the closest and 0.61 cm for the most distant cancers (range 0–1.2 cm). Mean Gleason score was 7 (range 5–9). Pathologic stage was pT2 for 17 cases and pT3 for the remaining seven cases. There was no notable difference in cancer volume, location, distance to the urethra, Gleason score, pathologic stage or patients' age between these uPM3 positive group and those conventionally diagnosed.15, 16
Discussion
In recent years, the widespread application of the serum PSA test led to the diagnosis of a large number of prostate cancers confined to their primary site. However, the PSA test has a rather low specificity and even the combination of PSA in its various forms plus DRE results in a significant number of futile biopsies while still missing a not inconsiderable number of cancers at the lower end of the PSA level.4, 5, 6 In this context, the emergence of the uPM3 test as a biomarker for prostate cancer detection is highly promising.
PCA3DD3 was found to be notably overexpressed in the vast majority of prostate carcinomas and their metastases.10 Furthermore, with the RT-PCR method, PCA3DD3 was not detected in normal tissues or in cancers other than those originating in the prostate, nor could PCA3DD3 be detected in a number of tumor-derived cell lines save for the LNCaP line which is prostate cancer derived.10 Studies comparing the value of PCA3DD3 as a prostate cancer biomarker with that of the telomerase transcriptase (hTERT gene) found the former to be overall superior, even in a background of abundant non-neoplastic prostate tissue.11 It was also shown that PCA3DD3 could be identified in prostate cancer cells shedded into the urine subsequent to rectal palpation of the prostate, and a nucleic acid sequence amplification assay (uPM3™) was developed for detecting PCA3DD3 RNA in urine samples. This method proved to be successful in several studies.12, 13, 14
The uPM3 test represents a significant improvement over current methods for the detection of early prostate cancer; a notable feature was its 89% specificity in a series of 443 patients.13 Moreover, uPM3 may be regarded as a molecular test; and, it was noted that patients with a positive uPM3 were at higher risk of cancer than those with high grade PIN.13
Recently, a large multi-institutional study on the uPM3 test obtained results notably similar13 to those previously found in single institutions.12, 14 Given that the presence of prostate cells in the urine is sine qua non for performing the uPM3 test, standardization of the DRE procedure may be important for optimizing results;13 modifications of the kit used for RNA isolation may also lead to improvements.17, 18, 19 Finally, a key variable is the number of biopsy cores obtained considering that cancer may be missed in cases in which positive uPM3 results strongly suggest its presence.
Based on literature review, there was no notable difference in cancer volume, location, distance to the urethra, Gleason score, pathologic stage, serum PSA or patients' age between these uPM3 positive group and those conventionally diagnosed.15, 16, 20, 21, 22 Our observations on radical prostatectomy specimens removed for carcinoma with positive preoperative uPM3 testing indicate that uPM3 is a significant and independent biomarker that detects prostate cancers of similar volume, location, extent and grade as other tests for early detection. uPM3 does not preferentially identify large or aggressive prostate cancers.
References
Jemal A, Murray T, Ward E, et al. Cancer statistics, 2005. CA Cancer J Clin 2005;55:10–30.
Kupelian PA, Eshaihk M, Reddy CA, et al. Comparison of the efficacy of local therapies for localized prostate cancer in the PSA era: large single institution experience with radical prostatectomy and external beam radiotherapy. J Clin Oncol 2002;20:3376–3385.
Kupelian PA, Potters L, Khuntia D, et al. Radical prostatectomy, external beam radiotherapy <72 Gy, external beam radiotherapy ≥72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T 1-T2 prostate cancer. Intl J Radiat Oncol Biol Phys 2004;58:25–33.
Babaian RJ, Johnston DA, Naccarato W, et al. The incidence of prostate cancer in a screening population with a serum prostate specific antigen between 2.5 and 4.0 ng/ml: relationship to biopsy strategy. J Urol 2001;165:757–760.
Catalona WJ, Smith DS, Ornstein DK . Prostate cancer detection in men with serum PSA concentrations of 2.6 to 4.0 ng/ml and benign prostatic examination: enhancement of specificity with free PSA measurements. JAMA 1997;277:1452–1455.
Thompson TM, Pauler DK, Goodman PJ, et al. Prevalence of prostate cancer among men with a prostate-specific antigen of 4.0 ng per milliliter. N Engl J Med 2004;350:2239–2246.
Mikolajczyk SD, Marks LS, Partin AW, et al. Free prostate-specific antigen in serum is becoming more complex. Urology 2002;59:797–802.
Sokoll U, Chan DW, Mikolajczyk SD, et al. Proenzyme PSA for the early detection of prostate cancer in the 2.5–4.0 ng/ml total PSA range: preliminary analysis. Urology 2003;6T:274–276.
Roehl KA, Antenor JAV, Catalona WJ . Robustness of free prostate specific antigen measurements to reduce unnecessary biopsies in the 2.6 to 4.0 ng/ml range. J Urol 2002;168:922–925.
Bussemakers MJG, van Bokhoven A, Verhargh GW, et al. DD3: a new prostate-specific gene, highly overexpressed in prostate cancer. Cancer Res 1999;59:5975–5979.
de Kok JB, Verhaegh OW, Roelofs RW, et al. DD3 (PCA3), a very sensitive and specific marker to detect prostate cancer. Cancer Res 2002;62:2695–2698.
Hessels D, Klein Gunnewiek JMT, van Oort I, et al. DD3 (PCA3)-based molecular urine analysis for the diagnosis of prostate cancer. Eur Urol 2003;44:8–16.
Fradet Y, Saad F, Aprikian A, et al. uPM3, a new molecular urine test for the detection of prostate cancer. Urology 2004;64:311–316.
Tinzl M, Marberger M, Horvath S, et al. DD3 (PCA3) RNA analysis in urine. A new perspective for detecting prostate cancer. Eur Urol 2004;46:182–187.
Qian J, Bostwick DG, Takahashi S, et al. Chromosomal anomalies in prostatic intraepithelial neoplasia and carcinoma detected by fluorescence in situ hybridization. Cancer Res 1995;55:5408–5414.
Qian J, Wollan P, Bostwick DG . The extent and multicentricity of high grade intraepithelial neoplasia in clinically localized prostatic adenocarcinoma. Hum pathol 1997;28:143–148.
Meid FH, Gygi CM, Leisinger H-J, et al. The use of telomerase activity for the detection of prostate cancer cells after prostatic massage. J Urol 2001;165:1802–1805.
Goessl C, Mueller M, Heicapell R, et al. DNA-based detection of prostate cancer in urine after prostatic massage. Urology 2001;58:335–338.
Goessl C, Krause H, Mueller M, et al. Fluorescent methylation-specific polymerase chain reaction for CAN-based detection of prostate cancer in bodily fluids. Cancer Res 2000;60:5941–5945.
Eichelberger LE, Koch MO, Eble JN, et al. Maximum tumor diameter is an independent predictor of prostate-specific antigen recurrence in prostate cancer. Mod Pathol 2005;18:886–890.
Herman CM, Kattan MW, Ohori M, et al. Primary Gleason pattern as a predictor of disease progression in gleason score 7 prostate cancer: a multivariate analysis of 823 men treated with radical prostatectomy. Am J Surg Pathol 2001;25:657–660.
Moul JW, Connelly RR, Mooneyhan RM, et al. Racial differences in tumor volume and prostate specific antigen among radical prostatectomy patients. J Urol 1999;162:394–397.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bostwick, D., Gould, V., Qian, J. et al. Prostate cancer detected by uPM3: radical prostatectomy findings. Mod Pathol 19, 630–633 (2006). https://doi.org/10.1038/modpathol.3800583
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.3800583
Keywords
This article is cited by
-
Prediction of prostate cancer to urethra distance by a pretreatment nomogram: urethral thermoprotection implication in cryoablation
Prostate Cancer and Prostatic Diseases (2013)
-
Identification of PCA3 (DD3) in prostatic carcinoma by in situ hybridization
Modern Pathology (2007)