Abstract
Background: Stereotactic incisional core breast biopsy (SCBB) is a highly specific technique for diagnosing ductal carcinoma in situ (DCIS) in patients with suspicious mammographic microcalcifications. However, its sensitivity for excluding the presence of coexisting occult invasive disease in this setting is not fully established. Design: We correlated SCBB findings to subsequent lumpectomy/mastectomy (lx/mx) results in 122 cases of DCIS. In 29 of these cases, the SCBB showed microscopic invasion (n = 15) or foci that were suspicious for invasion (n = 14). Likelihood for invasive disease in subsequent lx/mx samples from each case then was compared with various parameters, including DCIS grade, extent and mammographic findings. Results: Overall, 13% of cases in which the SCBB showed DCIS only (i.e., without any evidence of invasion), had invasive disease in the subsequent excision. This finding was significantly correlated with DCIS grade (low: 0/26 [0%], intermediate: 2/31 [6%], high: 10/36 [28%], P < .001). Invasive lesions were usually small (nine T1a, one T1b, and two T1c) and typically present within more extensive fields of DCIS (no invasion: 1.5 cm DCIS size; invasion: 2.8 cm mean DCIS size, P = .01). This was reflected by greater extent of involvement in the SCBB (5/8 cases with invasion had >15 ducts involved, versus 4/23 with <15 ducts involved, P = .03). SCBB that were suspicious or positive for microinvasion demonstrated invasion in most subsequent excision (susp: 7/14 [50%], microinv: 11/15 [73%]), generally of significant extent (11/18 T1b-c). Conclusions: 1. Patients with SCBB showing high grade DCIS and DCIS suspicious or positive for microinvasion have a significant and high likelihood, respectively, of harboring occult invasive neoplasm. They should accordingly be carefully evaluated radiographically, and possibly with sentinel node biopsy to facilitate axillary staging. 2. Likelihood of occult invasion is correlated with overall DCIS size/extent.
Similar content being viewed by others
INTRODUCTION
Stereotactic incisional core breast biopsy (SCBB) has been shown to be a useful method for investigating nonpalpable masses or suspicious calcifications that are detected on screening mammogram (1, 2, 3, 4, 5, 6). In many specialized centers, it has become the preferred method of tissue sampling for such lesions. It has the advantage of being a minimally invasive approach to establishing the diagnosis of ductal carcinoma in situ (DCIS) in a manner that facilitates planning of optimal (i.e., one stage) surgical excision (7, 8). Exclusion of invasive neoplasm in this setting is important because it obviates the need for staging of axillary lymph nodes at the time of lumpectomy (lx).
There are potential problems, however, with initiating surgical therapy for DCIS based on a diagnosis obtained using SCBB. First, some cases of mammographically detected DCIS are accompanied by occult invasive neoplasm. If such areas are not sampled on the SCBB, these patients may need to return for a separate axillary staging procedure. Second, SCBB showing DCIS that is accompanied by microscopic stromal invasion may be difficult for pathologists to assess due to incomplete sampling or fragmentation of tissue cores. In such cases, estimates of invasive tumor size may be misleading. If there is residual, unsampled invasive disease identified in the subsequent lx tissues, the inability to reconstruct lesional microanatomy may potentially result in staging ambiguity (9). Finally, microscopic invasion is sometimes difficult to distinguish from tangentially sectioned ducts or lobules that contain in situ neoplasm, particularly if there is a proliferative stromal reaction. In such cases, the diagnosis of invasion on SCBB may be equivocal.
In this study we report our experience with staging and surgical treatment of a consecutive series of patients with DCIS, with and without microinvasion, diagnosed using SCBB. Our objectives are, first, to define the frequency and causes of understaging of patients by SCBB and, second, to investigate histologic or radiographic criteria that may be used to better define disease stage (i.e., with respect to degree of invasion).
METHODS AND MATERIALS
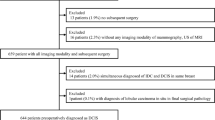
Surgical pathology reports of all ultrasound-guided and stereotactic incisional core breast biopsies performed at Harper University Hospital and Karmanos Cancer Institute from 1997 to 2000 were reviewed. All patients having a diagnosis of DCIS (n = 93), DCIS with microscopic invasion (n = 15), or DCIS with foci suspicious for invasion (n = 14) were recovered. Only cases having subsequent lx or mastectomy (mx) performed in our institution were further evaluated. Cases in which core biopsies were performed to evaluate calcifications when a known ipsilateral invasive neoplasm was present were also excluded (n = 8), leaving a total of 122 patients. The average age of patients at the time of biopsy was 59.5 years.
SCBB performed to evaluate suspicious calcifications accounted for most cases, but all 11 ultrasound-guided cores and eight SCBB in patients with microcalcifications were also associated with a mammographic mass. American College of Radiology (ACR) classification of 4 or 5 was assigned to the mammographic abnormalities with one exception (ACR 3) (10).
All SCBB (n = 111) were performed using a Fisher stereotactic table. The calcifications were localized and an 11 gauge Mammotome probe was introduced into the breast. Typically, 12 to 15 core biopsies were taken. The ultrasound-guided core biopsies (n = 11) were performed under direct ultrasound visualization. A 14-gauge Bard disposable core biopsy needle was inserted, and five to six biopsies were obtained. Routine processing with zinc-formalin and paraffin embedding was completed and five hematoxylin- and eosin-stained levels were prepared on tissue blocks for each specimen. All SCBB biopsy cores were placed on a quadrant-labeled Petri dish that was radiographed, thereby confirming lesional representation and permitting the directed recutting of the blocks in cases where the initial sections failed to reveal microcalcifications.
Grading of DCIS was performed (prospectively) according to the criteria of the Consensus Committee Report (11), which emphasizes the cytologic features of neoplastic cells. Cases in which neoplastic cells have small monotonous nuclei are considered low grade and cases with large, pleomorphic angular nuclei, frequent mitoses and prominent nucleoli are considered high grade. Intermediate grade tumors exhibit cytologic features between these two ends of the spectrum. So-called comedo-type necrosis is absent or, at most, extremely focal/limited, in low grade lesions and nearly always present, often extensive, in high grade lesions. Cribriform or papillary architecture, in contrast, is more characteristic of low grade DCIS. These criteria are illustrated in Figure 1. Lesions with grade heterogeneity were put into the higher category if at least 30% of sampled ducts were involved by the cytologically more aggressive cells.
DCIS grading. A, Low grade DCIS with small monotonous cells forming a cribriform architectural pattern. Mitotic activity and nucleoli are not readily identified. B, Intermediate grade DCIS with larger, more pleomorphic nuclei. Some of the nuclei have nucleoli. C, High grade DCIS with large, pleomorphic, angular nuclei and prominent nucleoli. Mitotic activity is present. (Hematoxylin and eosin stain, magnification ×100.)
Microinvasion was defined as one or more tissue cores having one or more nodules of invading neoplastic cells in periductal or perilobular stroma, with none exceeding 1.0 mm (see Fig. 2). Stromal microinvasion was typically associated with a cellular reaction characterized by fibroblast proliferation, collagenization and focal inflammatory cell infiltrates. In cases diagnosed as suspicious for invasion, the periductal or perilobular stroma contained either isolated individual neoplastic cells or rare clusters of cells thought to be neoplastic (see Fig. 2). Review of multiple levels from these cases failed to demonstrate continuity of such cells/groups with adjacent in situ neoplasm or underlying residual epithelial structures.
Microinvasion and suspicious for invasion. A, Microinvasion. Photomicrograph shows multiple single neoplastic cells (invasive cells lower left) invading into the periductal stroma. B, C, D, suspicious for invasion. These photomicrographs show individual cells (B, arrowhead; C, arrowhead) or a small nest of three to four cells invading the periductal stroma (D, arrowhead). Note periductal proliferative/inflammatory stromal reaction. (Hematoxylin and eosin stain, magnification ×100 for all four panels.)
Quantitation of DCIS extent was performed by retrospective study of the tissue sections from all cases of SCBB showing high grade DCIS. Using an Olympus BH-4 microscope, hematoxylin- and eosin-stained tissue sections from each block were used to count the number of ducts involved by in situ neoplasm. Adjacent duct lumens with DCIS that clearly represented cross-sections from one duct were counted only once. The presence of comedonecrosis was assessed based on the presence of eosinophilic material containing cellular debris filling the lumina of ducts involved by in situ neoplasm. The presence of a stromal reaction was defined as fibroblast proliferation, collagenization and inflammatory cell infiltrates surrounding ducts involved by in situ neoplasm.
RESULTS
Overall, 55 (45%) of the SCBB showed high grade DCIS, 37 (30%) showed intermediate grade DCIS, and 30 (25%) showed low grade DCIS. A small, but significant, proportion of cases diagnosed as pure DCIS in the SCBB (n = 12, 13%) showed invasive disease in subsequent lx/mx specimens. Incidence of invasion in open excisions was strongly correlated with DCIS grade in SCBB (low grade: 0/26 [0%], intermediate grade: 2/31 [6%], high grade: 10/36 [28%], P < .001). The extent of invasive disease in this subset of cases, however, was typically limited (see Table 1). Most were T1a (0–5 mm [n = 9]) with the remainder T1b (6–10 mm [n = 1]) and T1c (11–20 mm [n = 2]). DCIS size (as measured on excision samples) was significantly larger in the cases that were invasive (DCIS only: 0.2 cm to 3.4 cm, ave 1.5 cm, versus invasive: 0.6 cm to 6.5 cm, ave 2.8 cm, P = .01). In the excisions that revealed invasion, 8/11 (73%) cases had a field of DCIS greater than 2.0 cm in diameter and an additional patient had diffuse multiquadrant disease. In contrast, only 12% of high grade cases (2/17) without invasion had greater than 2 cm of DCIS in the excision (P = .003). One case with T1c disease at excision had multiquadrant disease and the second had a 6-cm field of DCIS with multifocal invasion.
Most of the cases with a suspicious mammographic nodule (58%) were found to harbor invasive disease, either on the core or in the subsequent excision (ultrasound cores: 7/11, stereotactic cores: 4/8, Table 2). Of the ultrasound-guided core biopsies shown to be invasive in the excision, however, three were suspicious for invasion on biopsy, two were microinvasive, and the remaining two showed only DCIS in the biopsy. One additional ultrasound core biopsy showed microinvasion, but only DCIS was found in the subsequent excision. Four of the seven cases were T1a lesions (Table 2). Of the four SCBB shown to be invasive on subsequent excision; two showed microinvasion on the core and remaining two cases were suspicious for invasion on the core. On subsequent excision, two were T1a lesions, one was T1b, and one was T1c.
In SCBB showing high grade DCIS without evidence of invasion, presence of invasive disease in subsequent therapeutic excisions was correlated with the number of ducts involved by neoplasm. These data are summarized in Table 3. Twenty percent of cases showed invasion in lx/mx if <5 ducts were involved by DCIS and 17% were invasive if 5 to 15 ducts were involved, but 63% showed invasion when >15 ducts in the SCBB contained neoplasm. Presence of a periductal stromal reaction was not correlated with occult invasion (i.e., in SCBB showing high grade DCIS, data not shown).
A small but significant number of cases with SCBB showing DCIS, 12% overall (n = 11), were negative for residual neoplasm in the subsequent excision specimens. Most of these cases (9/11) had low or intermediate grade DCIS in SCBB. In all of the cases that were negative for residual neoplasm on excision, the extent of disease in the SCBB samples was microfocal, involving fewer than seven duct lumens in each.
Most of the core biopsies showing microscopic invasion or foci suspicious for invasion exhibited high grade DCIS (19/29, 66%), and only 14% (4/29) had low grade in situ neoplasm. Invasive neoplasm in lx/mx was less likely, but still frequent, in patients whose SCBB was suspicious for invasion (7/14, 50%), compared with cases in which the SCBB was microinvasive (11/15, 73%). In contrast to the extent of invasive disease when SCBB showed DCIS only, most of these patients had more significant (T1b/T1c) invasion (11/18) (see Table 4). As noted above, the size of the DCIS in subsequent lx/mx cases was significantly larger in the cases that were invasive (DCIS only: 0.6 cm to 1.7 cm, ave 1.3 cm versus invasive: 1.8 cm to 17 cm, ave 4.9 cm). Nodal metastases were eventually identified in 33% (n = 6) of the 18 patients in this group who underwent axillary sampling.
DISCUSSION
Others have reported occult invasion in 9 to 29% of excisions after SCBB showing DCIS (1, 4, 5, 6, 8, 12). Our study shows that invasive carcinoma is present in 13% of the cases in which SCBB showed DCIS without any evidence of invasion. Thus, SCBB is associated with a significant “false negative,” or understaging, rate. However, our observations extend previous studies by noting that most cases with invasion undiagnosed by SCBB had high grade DCIS (10/12, 83%) and that 28% of high grade DCIS were associated with invasion. These findings underscore the divergent biology of aggressive high grade versus indolent, low grade, DCIS. We believe that grade should therefore be carefully assessed on all SCBB specimens to convey the risk for underlying occult invasion to clinicians. Among high grade DCIS, the lesion size/extent was another parameter we have identified that was related to likelihood of occult invasion; most such cases were associated with >2.0 cm of in situ disease. Accordingly, patients having SCBB showing greater than 15 ducts with high grade DCIS were at greater risk. The association with extensive disease, in conjunction with the finding that most (75%) invasive lesions missed on SCBB were T1a, implies that understaging reflects an artifact attributable to limited tissue sampling. Taken together, our findings imply that patients with high grade DCIS on SCBB, especially if there is evidence of more extensive disease, should be considered for either sentinel node biopsy or, perhaps, additional biopsy sampling to exclude occult invasion.
In contrast to our findings, Lee et al. reported that no histologic parameter correlated with increased risk for occult invasion (12). These authors evaluated mean number of core samples per biopsy, the size of lesion as well as nuclear grade. Almost half of the cases in their study utilized a 14-gauge needle to retrieve approximately five cores, compared with 12 to 15 11-gauge cores in our study. We believe a smaller number of cases (n = 59), combined with more limited sampling in their series, likely accounts for the discrepancy between the two studies.
Most patients in our study underwent significant tissue sampling with SCBB, with aggregate specimen weights typically greater than 1 gm, resulting in biopsy cavities of approximately 1 cm in diameter. Due to relatively liberal sampling, we believe that attempts to estimate tumor size/extent on SCBB reflect actual disease burden. Nevertheless, even this degree of sampling was insufficient to fully characterize some lesions that, as it turned out, were in fact greater than 2.0 cm. Clearly, more limited sampling (i.e., five cores or less) would provide even less reliable estimates of tumor extent. We do not interpret our results as sufficient reason to advocate the method of DCIS quantitation described herein, but rather as evidence that DCIS burden in SCBB likely has clinical relevance. Recommendations for reporting SCBB results (i.e., apart from diagnosis) should, in our opinion, await the outcome of other studies.
Complete removal of carcinoma (invasive or in situ) has been previously reported in 17 to 24% of cases (3, 8) compared with the 12% reported in this study. Our data indicate that absence of residual disease in such cases reflects small tumor size/extent. All cases in our study that were negative for residual neoplasm on excision had microfocal DCIS on SCBB involving fewer than seven duct lumens. Thus, assessment of DCIS extent on SCBB may, in some cases, be the only means of evaluating tumor size, further underscoring the relevance of attempts to quantify disease in biopsy samples.
Partial lesion representation in SCBB may complicate grading of DCIS. Intratumoral morphologic heterogeneity is common in DCIS, and may complicate histologic assessments of grade even in open biopsies. In this study, a DCIS lesion with heterogeneity on SCBB was assigned to the higher grade category whenever it comprised at least 30% of the sampled lesion. However, 8/30 (22%) high grade DCIS cases in our study exhibited admixed intermediate grade neoplasm and 9/31 (29%) intermediate grade cases contained rare foci of high grade DCIS on SCBB. Thus, it is perhaps not surprising that grade assessments on SCBB were different from those on excision in 17% of cases (see Table 1).
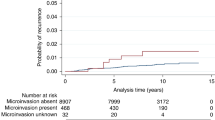
Another potential method of estimating DCIS extent is by measuring the size of the clusters of microcalcifications on mammograms. This prompted us to compare mammographic DCIS extent to that assessed on pathologic tissue examination. Among 68 high and intermediate grade lesions in which films were available for review, mammographic measurements of clusters of microcalcifications agreed with the DCIS size on pathology reports (i.e., within ±5 mm) in only 30% of cases. In 47% of cases, the mammogram overestimated DCIS size by at least 5 mm. Others have reported similar findings (12, 13) that likely reflect radiographic overestimates due to microcalcifications in areas of fibrocystic change at the periphery of DCIS lesions. Mammographic calcification extent was useful for assessing presence or absence of invasion only when size of the cluster was less than 1.0 cm (n = 14); none of these cases had invasive disease. If the size of the calcifications was 1.0 to 5.0 cm (n = 41), 34% had invasion, but if calcifications measured >5.0 cm (n = 13) only slightly more patients (38%) had invasion (Fig. 3). It is noteworthy that, unlike DCIS extent in SCBB, the findings in Figure 3 appear to show that mammographic calcification size is most useful as a predictor for absence (versus presence) of invasion. However, distribution of mammographic findings was potentially useful. Thirty-two percent (23/71) of cases had multifocal clusters of microcalcifications; of these (15/23, 65%) were invasive on excision, thus reinforcing our earlier statement that invasive tumors “missed” on SCBB reflect sampling error on cases with widespread (and likely multifocal) disease. These findings imply that presurgical estimates of DCIS extent (and, for that matter, likelihood of occult invasion) are best made using a combination of radiographic and pathologic data. We should note that the degree of tissue sampling in our series was not uniform; this is another factor that affects detection of occult invasion.
CONCLUSION
Microscopic invasion or foci suspicious for invasion are a frequently encountered problem in core biopsies showing DCIS, collectively accounting for 24% of our cases. We would emphasize that cases of DCIS may have a periductal stromal reaction that can be difficult to distinguish from a desmoplastic reaction associated with true invasion. It should be noted, however, that 21% (6/29) of the microinvasive/suspicious for invasion cases were associated with a suspicious mass on the mammogram (ultrasound-guided cores excluded). These cases present two problems with respect to case management. On the one hand, most were invasive on lx/mx and 38% harbored significant (T1b or T1c) invasion within unsampled tissue. Thus, specimens diagnosed as microinvasive or suspicious should be carefully evaluated histologically and mammographically with consideration given to sentinel node biopsy. Because these patients had extensive DCIS on core biopsy, assessments of disease extent may have utility in predicting likelihood of invasive disease. On the other hand, SCBB removes all invasive neoplasm in at least some cases (27% in our study) (9) and pathologists should thus be prepared to provide estimates of invasive tumor size from core biopsy samples.
References
Brenner RJ, Bassett LW, Fajardo LL, et al. Stereotactic core-needle breast biopsy: a multi-institutional prospective trial. Radiology 2001; 218: 866–872.
Dahlstrom JE, Sutton S, Jain S . Histologic-radiologic correlation of mammographically detected microcalcification in stereotactic core biopsies. Am J Surg Pathol 1998; 22: 256–259.
Gajdos C, Levy M, Herman Z, Herman G, Bleiweiss IJ, Tartter PI . Complete removal of nonpalpable breast malignancies with a stereotactic percutaneous vacuum-assisted biopsy instrument. J Am Coll Surg 1999; 189: 237–240.
Latosinsky S, Cornell D, Bear HD, Karp SE, Little S, Paredes ED . Evaluation of stereotactic core needle biopsy (SCNB) of the breast at a single institution. Breast Cancer Res Treat 2000; 60: 277–283.
Rich PM, Michell MJ, Humphreys S, Howes GP, Nunnerley HB . Stereotactic 14G core biopsy of non-palpable breast cancer: what is the relationship between the number of core samples taken and the sensitivity for detection of malignancy? Clin Radiol 1999; 54: 384–389.
Won B, Reynolds HE, Lazaridis CL, Jackson VP . Stereotactic biopsy of ductal carcinoma in situ of the breast using an 11-gauge vacuum-assisted device: persistent underestimation of disease. AJR Am J Roentgenol 1999; 173: 227–229.
Jimenez RE, Bongers S, Bouwman D, Segel M, Visscher DW . Clinicopathologic significance of ductal carcinoma in situ in breast core needle biopsies with invasive cancer. Am J Surg Pathol 2000; 24: 123–128.
Burak WE JR, Owens KE, Tighe MB, et al. Vacuum-assisted stereotactic breast biopsy: histologic underestimation of malignant lesions. Arch Surg 2000; 135: 700–703.
Liberman L, Zakowski MF, Avery S, et al. Complete percu-taneous excision of infiltrating carcinoma at stereotactic breast biopsy: how can tumor size be assessed? AJR Am J Roentgenol 1999; 173: 1315–1322.
American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS™). 3rd ed. Reston, VA: American College of Radiology; 1998.
Consensus Conference Committee. Consensus conference on the classification of ductal carcinoma in situ. Cancer 1997; 80: 1798–1802.
Lee CH, Carter D, Philpotts LE, et al. Ductal carcinoma in situ diagnosed with stereotactic core needle biopsy: can invasion be predicted? Radiology 2000; 217: 466–470.
Liberman L, Drotman M, Morris EA, et al. Imaging-histologic discordance at percutaneous breast biopsy. Cancer 2000; 89: 2538–2546.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonnett, M., Wallis, T., Rossmann, M. et al. Histologic and Radiographic Analysis of Ductal Carcinoma In Situ Diagnosed Using Stereotactic Incisional Core Breast Biopsy. Mod Pathol 15, 95–101 (2002). https://doi.org/10.1038/modpathol.3880497
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.3880497
Keywords
This article is cited by
-
The role of breast MR imaging in pre-operative determination of invasive disease for ductal carcinoma in situ diagnosed by needle biopsy
European Radiology (2012)
-
Predictors of invasion in needle core biopsies of the breast with ductal carcinoma in situ
Modern Pathology (2010)
-
Diagnosing breast lesions by fine needle aspiration cytology or core biopsy: which is better?
Breast Cancer Research and Treatment (2010)
-
Flat DIN 1 (flat epithelial atypia) on core needle biopsy: 63 cases identified retrospectively among 1,751 core biopsies performed over an 8-year period (1992–1999)
Virchows Archiv (2007)