Abstract
Data sources
PubMed, Web of Science and the Cochrane Oral Health Group Trials Register, www.clinicaltrials.gov, www.centerwatch.com and www.clinicalconnection.com databases. Manual searches of a number of dental journals and the reference lists of identified studies were undertaken.
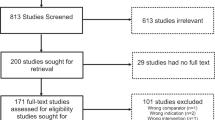
Study selection
Human clinical studies comparing implant failure rates in diabetic and non-diabetic patients were considered. Three reviewers independently selected studies.
Data extraction and synthesis
The definition of implant failure used was complete loss of the implant. Study quality was assessed using the Cochrane risk of bias approach. A narrative summary of the studies and meta-analysis are presented.
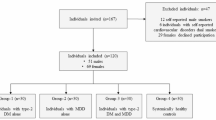
Results
Fourteen studies were included (one randomised controlled trial, six controlled clinical trials and seven retrospective analysis); all 14 were considered to be at high risk of bias. Meta-analysis (14 studies) found no significant difference between diabetic and non-diabetic patients; risk ratio of 1.07 (95% CI = 0.80, 1.44)(p = 65). A meta-analysis of two studies found a statistically significant difference (mean difference =0.20, 95% CI = 0.08, 0.31 p = 001;) between diabetic and non-diabetic patients concerning marginal bone loss, favouring non-diabetic patients. Meta-analysis was not possible for postoperative infections.
Conclusions
The results of the present systematic review should be interpreted with caution because of the presence of uncontrolled confounding factors in the included studies. Within the limits of the existing investigations, the difference between the insertion of dental implants in non-diabetic and diabetic patients did not statistically affect the implant failure rates.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Box 6.3.a pp 122, Cochrane Handbook for Systematic Reviews of Interventions. Higgins JPT, Green S, editors. Chichester, West Sussex: The Cochrane Collaboration and John Wiley & Sons Ltd; 2009.
Sanderson S, Tatt ID, Higgins JP . Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 2007; 36: 666–676. PubMed PMID: 17470488. Epub 2007/05/02. eng.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. PubMed PMID: 19621070. Pubmed Central PMCID: 2707010. Epub 2009/07/22. eng.
Author information
Authors and Affiliations
Additional information
Address for correspondence: B. Chrcanovic, Department of Prosthodontics, Faculty of Odontology, Malmö University, Malmö, Sweden. E-mail: bruno.chrcanovic@mah.se
Chrcanovic BR, Albrektsson T, Wennerberg A. Diabetes and oral implant failure: a systematic review. J Dent Res 2014; 93: 859–867.
Rights and permissions
About this article
Cite this article
Hurst, D. Evidence unclear on whether Type I or II diabetes increases the risk of implant failure. Evid Based Dent 15, 102–103 (2014). https://doi.org/10.1038/sj.ebd.6401057
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ebd.6401057
This article is cited by
-
Retrospective cohort study of a tapered implant with high primary stability in patients with local and systemic risk factors—7-year data
International Journal of Implant Dentistry (2018)