Abstract
Purpose To report the clinical features and topographic findings of superior pellucid marginal corneal degeneration (PMCD).
Methods Retrospective chart review of 15 eyes of eight patients of superior PMCD. Detailed history, visual acuity at presentation, degree of astigmatism, slit-lamp examination findings, topographic features, and Orbscan findings were noted where available. Improvement in visual acuity with spectacles or contact lens correction, surgical procedure if any, and final visual acuity were analysed.
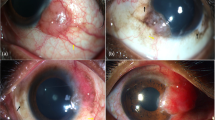
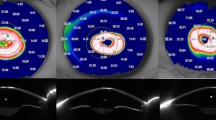
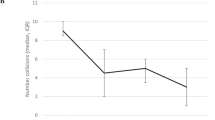
Results In all, six patients were males and two were females. All cases except one were bilateral. The patients ranged in age from 18 to 48 years. All cases had isolated superior PMCD. One patient was a diagnosed case of vernal keratoconjunctivitis. The visual acuity at presentation ranged from hand motions to 20/25. The degree of thinning varied from 30 to 90%. The extent of thinning was commonly seen between the 10 and 2 o'clock positions. Ectasia was seen below the site of thinning in all the cases of superior PMCD. Topographic features including vertical corridor of reduced power, against-the-rule astigmatism and superior loop cylinder were seen in 10 eyes. Orbscan was carried out in two eyes of one patient and revealed an area of increased elevation in relation to the best-fit sphere superiorly corresponding to the area of ectasia in both the eyes. The visual acuity improved with rigid gas-permeable contact lens in six eyes and the final visual acuity ranged from 20/400 to 20/30. Two eyes were subjected to surgical intervention (peripheral annular graft=1 and lamellar graft=1).
Conclusions PMCD can occur superiorly. It should be considered in the differential diagnosis of superior ectatic disorders. The topographic findings, of reduced power in the vertical meridian and superior loop cylinder, are typical of superior pellucid marginal degeneration. Visual rehabilitation is usually possible with contact lenses, with surgical management required in selected cases.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Krachmer JH . Pellucid marginal degeneration. Arch Ophthalmol 1978; 96: 1217.
Karabatsas CH, Cook SD . Topograhic analysis in pellucid marginal degeneration and keratoglobus. Eye 1996; 10: 451–455.
Cameron JA, Mahmood MA . Superior corneal thinning with pellucid marginal degeneration. Am J Ophthalmol 1990; 109: 486–487.
Maguire LJ, Klyce SD, McDonald MB, Kaufman HE . Corneal topograhpy of pellucid marginal degeneration. Ophthalmology 1987; 94: 519–524.
Wagenhorst BB . Unilateral Pellucid marginal degeneration in an elderly patient. Br J Ophthalmol 1996; 80: 927–928.
Basak SK, Hazar TK, Bhattacharya D, Sinha TK . Unilateral pellucid marginal degeneration. Indian J Ophthalmol 2000; 48(3): 233–234.
Bower KS, Dhaliwal DK, Barnhorst Jr DA, Warnicke J . Pellucid marginal degeneration with superior corneal thinning. Cornea 1997; 16: 483–485.
Rao SK, Fogla R, Padmanabhan P et al. Corneal topography in atypical pellucid marginal degeneration. Cornea 1999; 18(3): 265–272.
Tagalia DP, Sugar J . Superior pellucid marginal corneal degeneration with Hydrops. Arch Ophthalmol 1997; 115: 274–275.
Wilson SE, Lin DTC, Klyce SD et al. Terrien's marginal degeneration: corneal topography. Refract Corn Surg 1990; 6: 15–20.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sridhar, M., Mahesh, S., Bansal, A. et al. Superior pellucid marginal corneal degeneration. Eye 18, 393–399 (2004). https://doi.org/10.1038/sj.eye.6700643
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.eye.6700643
Keywords
This article is cited by
-
Laser in situ keratomileusis (LASİK) in patients with superior steepening on corneal topography: Is it safe and predictable?
International Ophthalmology (2020)