Abstract
Purpose
To evaluate the outcome of penetrating keratoplasty in patients with bilateral corneal blindness.
Methods
Bilaterally blind patients who had undergone optical penetrating keratoplasty (PK) were evaluated on optical and refractive parameters and presence of complications if any. The results at 3 months, 6 months, and 1 year were compared with age-matched and indication-matched unilaterally blind controls.
Results
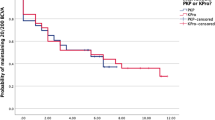
The most common indication for surgery in both the groups was the presence of a corneoiridic scar. Best corrected visual acuity of ⩾6/18 was seen in five (16.66%) patients in the study group and in 11 (36.66%) patients in the control group (P=0.14). In all, 15 (50%) grafts in the study group and six (20%) in the control group failed (P=0.03). The most common cause of failure was graft infection (40%) in the study group and post-PK glaucoma (20%) in the control group. The percentage of graft rejection as a cause of graft failure was the same in both the groups. A composite socioeconomic status scale based on family literacy and income suggested that 70% of the cases in the study group and 30% in the control group belonged to the low socioeconomic group (P=0.004).
Conclusion
The outcome of optical penetrating keratoplasty in patients with bilaterally blinding corneal disease is poorer than those who are unilaterally blind. Low socioeconomic status may be a contributing factor for the poor outcome.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Thylefors B, Negrel AD, Pararajasegaram R, Dadzie KY . Global data on blindness. Bull World Health Organ 1995; 73: 115–121.
Dandona R, Dandona L . Corneal blindness in a southern Indian population: need for health promotion strategies. Br J Ophthalmol 2003; 87: 133–141.
Vail A, Gore SM, Bradley BA, Easty DL, Rogers CA . Corneal graft survival and visual outcome. A Multicenter Study. Cornea Follow-up Study Collaborators. Ophthalmology 1994; 101: 120–127.
Volker-Dieben HJ, D'Amaro J, Kok-Van Alphen CC . Hierarchy of prognostic factors for corneal allograft survival. Aust NZ J Ophthalmol 1987; 15: 11–18.
Williams KA, Roder D, Esterman A, Muehlberg SM, Coster DJ . Factors predictive of corneal graft survival Report from Australian Corneal Graft Registry. Ophthalmology 1992; 99: 403–414.
Stulting RD, Sumers KD, Cavanagh HD, Waring GO 3rd, Gammon JA . Penetrating keratoplasty in children. Ophthalmology 1984; 91: 1222–1230.
Jager MJ, Hermans LJA, Kok JHC . Visual results after corneal transplantation. Doc Ophthalmol 1989; 72: 265–271.
Dandona L, Naduvilath TJ, Janarthanan M, Ragu K, Rao GN . Survival analysis and visual outcome in a large series of corneal transplants in India. Br J Ophthalmol 1997; 81: 726–731.
Dandona L, Naduvilath TJ, Janarthanan M, Rao GN . Causes of corneal graft failure in India. Indian J Ophthalmol 1998; 46: 149–152.
Dandona R, Dandona L . Socioeconomic status and blindness. Br J Ophthalmol 2001; 85: 1484–1488.
Williams KA, Ash JK, Pararajasegaram P, Harris S, Coster J . Long term outcome after corneal transplantationVisual result and patient perception of success. Ophthalmology 1991; 98: 651–657.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the Annual Conference of the Royal College of Ophthalmologists, UK held in Birmingham from 20 to 22 May 2003
Rights and permissions
About this article
Cite this article
Sinha, R., Vanathi, M., Sharma, N. et al. Outcome of penetrating keratoplasty in patients with bilateral corneal blindness. Eye 19, 451–454 (2005). https://doi.org/10.1038/sj.eye.6701534
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.eye.6701534