Abstract
A number of effective therapies for the treatment of osteoporosis have become available in recent years. However, uncertainty exists regarding their long-term use and effectiveness. Bisphosphonate treatment, unlike hormone replacement, denosumab or teriparatide, is associated with benefits extended even after treatment discontinuation. The extended benefits are most apparent for alendronate (ALN) and zoledronate (ZOL). A drug holiday might be considered in patients at low-moderate risk and who have been fully compliant with treatment, and who have had a response to treatment. In patients at low-moderate risk of fractures the decision to consider a drug holiday should be balanced also with the safety profile of each treatment.
Similar content being viewed by others
Introduction
The aim of osteoporosis treatment is to prevent fragility fractures. Pharmacological treatment for osteoporosis is only indicated when the fracture risk is considered unacceptably high (1), such that treatment benefits overwhelmingly exceed the risks.
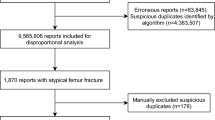
Pharmacological treatment should be continued while the fracture risk is high. Osteoporosis drugs may result in persistent structural benefits and a drug holiday may be considered. The issue of treatment duration for anti-reabsorptive drugs arises from potential risks related to long-term treatment, such as the risk of breast cancer with hormonal therapy or the risk of so-called osteonecrosis of the jaw, or atypical sub-trochanteric fractures (2,3) with bisphosphonates and denosumab. These adverse events are related to treatment duration and represent the most common cause of treatment discontinuation. Obviously, treatment discontinuation may lead to an increased risk of fracture within a certain time-frame, which might be considerably different among available therapies.
In this article we will summarize the available data concerning the consequences of anti-reabsorptive treatment discontinuation and the benefit/drawback ratio of discontinuation in relationship also with long term safety proifile.
The case of alendronate (ALN)
The first phase 3 study with ALN (4) for the treatment of postmenopausal osteoporosis (PMO) included three arms: placebo, 5 mg per day, and 10 mg per day. The placebo arm was abandoned after three years, while subjects on ALN continued treatment for two more years. At the end of the fifth year, subjects on 10 mg per day were randomized to continue the treatment, or to stop treatment with an additional 5 years of follow-up (5). Bone mineral density BMD changes clearly dissociated with the two ALN dosages after the first year, and for this reason all subjects on ALN were put on 10 mg per day in the FIT trial (6).
In the subjects who took 10 mg per day of ALN for 10 years, lumbar spine BMD rapidly increased after the first year (+5,5%). This was followed by an increase of 1.5% per year through to the 10th year of observation. Femoral BMD increased rapidly during the first two years (about +5%); followed by a slight increase (about 0.1% per year) thereafter. In subjects who discontinued ALN treatment, lumbar spine BMD remained unchanged over the five years of follow-up, but femoral BMD decreased within one year of treatment cessation. After 5 years of followup, the mean difference versus baseline in lumbar and femoral BMD between subjects who continued treatment and those who discontinued was 4.8% and 1.8%, respectively (Figure 1).
Variations of femoral or lumbar spine BMD and of two bone turnover markers (urine NTX or bone alkaline phosphatases) in the extension of phase 3 study with Alendronate in postmenopausal osteoporosis (5).
For a subset of subjects, the measurement of bone resorption (urine NTX) and bone formation markers (bone alkaline phosphatase or BALP) was available. At variance with BMD, bone turnover markers quickly increased within the first year following discontinuation of treatment. It is difficult to determine whether bone turnover markers fully returned to baseline levels, considering the effect of calcium and vitamin D supplementation, which were continued in all patients. From the placebo group data, only treated with calcium and vitamin D, during the first three years of treatment, it seems that all bone turnover markers remain somewhat suppressed by 10–20% even five years after treatment discontinuation. Subjects included in the extension of the study were of insufficient number for any analysis of the consequences of treatment cessation on the incidence of osteoporotic fractures.
The FIT pivotal trial of ALN for postmenopausal osteoporosis (FIT study)(6) included 6 459 subjects with only moderate osteoporosis (6–7). This was the first study with a primary end point fracture rate and still offers outstanding efficacy data on fracture risk.
The FIT study, with the inclusion of a placebo group, was extended for four years. Four months after the end of the controlled trial, approximately one thousand subjects were randomized to continue treatment with 5 or 10 mg per day ALN or placebo in the FLEX study (8), with five years of additional follow-up. No relevant differences were noted between subjects receiving 5 or 10 mg per day, and thus the two groups were analysed together versus the placebo group.
In subjects who continued treatment, lumbar spine BMD increased continuously by about 1% per year, while femoral BMD remained relatively stable. In the placebo group, lumbar spine BMD remained relatively stable, while hip BMD decreased to pre-treatment levels. At the end of the follow-up for the FLEX study, the difference between the treated and non-treated subjects was 3.8% and 2.4% for lumbar spine BMD and hip BMD, respectively (Figure 2).
Densitometric and bone turnover marker variations during the FIT study (Alendronate in postmenopausal osteoporosis) and its extension in the FLEX study. In the FLEX study patients previously treated with Alendronate were randomized to continue Alendronate or to placebo (9).
Bone turnover markers remained suppressed in subjects who continued treatment, while they gradually increased to baseline levels (pre-FIT) in placebo subjects (Figure 2).
The final results did not show differences in fracture counts between patients who continued and those who discontinued treatment. However, a statistically significant difference of 55% was observed for clinical vertebral fracture risk, i.e. the fractures diagnosed through the appearance of obvious symptoms. The risk of morphometric vertebral fractures was reduced by 14% (Figure 3).
Fracture incidence in the FLEX study, the extension of the FIT study only for previously treated patients with Alendronate (9).
The incidence of non-vertebral fractures was reanalysed post-hoc. Subjects were divided according to the severity of osteoporosis at the moment of inclusion in the FLEX study (9). Among patients with a diagnosis of osteoporosis according to the WHO (T score <−2.5), treatment with ALN was also associated with a significant 50% risk reduction of non-vertebral fractures (Figure 3).
Conclusions
The results on BMD and bone turnover markers in subjects who discontinued ALN treatment are similar after five and four years of treatment in the phase 3 trial and in the FLEX study, respectively. The cessation of ALN treatment was associated with long-term persistence of the positive BMD effects at the lumbar spine, while hip BMD slowly decreased. As compared to subjects who continued treatment, a clinically meaningful difference in BMDs (e.g.: > 2%) was apparent after more than two years of drug holiday.
Recently, McNabb et al. (10) showed that, in approximately one-third of patients who discontinued treatment in the FLEX study, total hip BMD decreased by more than 5% over the next five years. The authors could not define specific characteristics of the patients who experienced this bone loss and an association with fracture rate lacked any reasonable statistical power. The distribution of the bone loss was “normal” and this per se excludes the presence of a specific subpopulation.
In both ALN studies, bone turnover markers increased quickly within the first six months and then more slowly with the restoration of the original pre-treatment values within around five years.
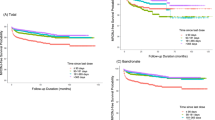
The results on fracture risk are not conclusive due to inadequate statistical power. However, in the FLEX study, the two lines of the incidence of clinical vertebral fractures seem to diverge only after year one (Figure 4).
Relative risk (RR) of non-vertebral fractures during FLEX study (Alendronate versus placebo) in patients ranked according with femoral neck BMD (T-score) values. In patient with persistent osteoporosis (T-score <−2.5) prosecution of treatment leads to an additional advantage also for non-vertebral fractures (10).
The case of risedronate
The clinical use of risedronate (RIS) includes three studies. One study was designed to verify the effectiveness on femoral fracture risk (HIP study) (11). The two studies with the goal of evaluating vertebral fracture risk reduction (VERT studies) were conducted in North America (VERT-NA) (12) and one in several other countries around the world (VERT-MN) (13). The VERT-NA study included a follow-up of one year after 3 years of RIS 5 mg per day or placebo (14). In the active group, the cessation of treatment was associated with a significant decrease within a year of the densitometric values to almost pre-treatment values for femoral BMD, while urine NTX (bone reabsorption marker) quickly returned to the values of the the placebo group (calcium and vitamin D).
Even if the duration of ALN treatment was slightly longer, the difference between the two bisphosphonates is evident. The tail-effect (i.e., the extension of the effects after treatment discontinuation) of ALN is about five times longer: the return to pre-treatment levels of bone turnover and BMD occurs after about one year in patients treated with RIS, and after about five years in those treated with ALN for four years (Figure 5).
The extension of VERT-MN study was more complex (15). The effect of treatment discontinuation was studied after two and seven years in subjects treated in the first three years with RIS or placebo. Also, with this study, the return to pre-treatment values of femoral neck BMD occurred within two years, while urine NTX levels returned to basal levels within six months, (Figure 6) independent of previous treatment duration.
Changes in femoral neck BMD and urine NTX in patients of VERT-MN study participating in the extension study. The open circle and the black triangle indicate the patients randomized to placebo and Risedronate respectively, in the first three years of the trial. The dashed line indicates the period in which the patients were on placebo and the continuous line patients when assuming RIS (15).
Conclusions:
ALN and RIS clearly differ regarding the “tail effect” in the clinical setting of trials differing marginally with each other. The tail effect is about five times longer for ALN: the return to pre-treatment levels of bone turnover and BMD occurs after about one year in patients treated with RIS and five years in those treated with ALN for 4 years. The duration of the treatment with RIS does not affect the duration of the tail effect.
The case of zoledronate
The original trial HORIZON with Zoledronic Acid (ZOL) versus placebo was carried out for three years (16). The subjects in the active group received three infusions of ZOL 5 mg. At the end of this period, the patients of the active group were randomized to continue or not the treatment with three years of follow-up. Densitometric difference between the two groups after the three years of follow-up was 1–2% due to the marginal decrease in femoral neck BMD in untreated subjects and to constant increases of lumbar spine BMD in subjects who received two additional ZOL infusions (Figure 7) (17).
Densitometric variations in the extension study with ZOL. The patients treated during the first three years with ZOL were randomized to continue or not treatment (17).
During the three years of follow-up, the two groups were undistinguishable in terms of the incidence of new non-vertebral fractures, while the incidence of vertebral fractures was significantly reduced by continuing treatment (Figure 8) (17).
Vertebral and non-vertebral fracture incidence in patients in the extension trial with ZOL. The patients treated in the first three years with ZOL were randomized to continue (Z6) or not (Z3P3) treatment (17).
From a recent sub-analysis (18), it has emerged that, in the subjects who received only one infusion of the drug, the reduction of clinical fracture risk (of any kind) was equal (−32%) to that observed in the subjects who received three infusions.
Conclusions:
The “tail effect” of ZOL appears to be quite important and apparently superior to that observed with ALN. Also with ZOL, treatment discontinuation is associated with a partial loss of efficacy on vertebral fracture risk, but not for non-vertebral fractures.
The case of other anti-resorptive agents
There is little data available on the tail effect of Ibandronate. What exists is limited to phase 2 studies (19). The emerging pattern shows a clear resemblance with RIS, with the restoration of bone turnover within 6–12 months from treatment cessation (Figure 9).
Bone turnover markers variation after ceasing of the treatment with Ibandronate (19).
There is no “tail effect” for treatment with estrogens and SERMS (Raloxifene and Basedoxifene) since, with their discontinuation, bone turnover returns to baseline levels within a few weeks, and all densitometric increases observed during treatment are lost within one year (20).
The effect of anti-RANKL treatment with Denosumab on bone turnover markers is rapidly lost with an apparent re-bound, values exceeding baseline values, lasting for a few months. This is associated with the rapid loss of all densitometric gains achieved during treatment (Figure 10) (21).
BMD and serum CTX variation (bone turnover marker) after discontinuing treatment with denosumab (shadowed area). Serum CTX increases to levels higher than baseline (21).
Data regarding the consequences of discontinuation of the treatment with Strontium Ranelate are limited and inconclusive due to the very small variations of bone turnover markers observed during treatment (22). The densitometric increases observed during treatment are related to an undefined effect of the atomic weight of strontium (much higher than that of calcium) absorbed in the bone tissue. This uncertainty is inevitably conveyed to the interpretation of the changes in BMD after treatment discontinuation.
The case of anabolic agents
The landmark trial with teriparatide (a drug with anabolic properties on bone) was discontinued after approximately 20–24 months of treatment (23). Due to the limited duration of the trial, we do not know whether the efficacy of treatment would have persisted if treatment was extended for the pre-planned 3 years, even though a loss of the full anabolic efficacy with time has been recently postulated (24).
The other anabolic agent registered in some European countries (not in North America) is PTH 1–84. Based on the experience with teriparatide, the majority of the patients were treated for only for 18 months with this drug (25).
Little is known about what takes place after discontinuing teriparatide treatment, but the available data indicates that bone formation markers rapidly returned to pre-treatment levels and most of the BMD gains were rapidly lost (26,27).
Safety profile of osteoporosis treatments
The ideal treatment duration and then the possibility to consider a treatment holiday is depending on the expected carry over effect (tail effect) of the ongoing treatment but also on the benefit/drawback ratio which is related also to the long-term safety profile of each treatment.
The safety profile of hormonal therapy was well scrutinized by the WHI studies (28). The increased risk of stroke and venous thromboembolic disease was confirmed, while the risk of coronary heart disease and breast cancer is significantly increased only for women taking combined estrogen plus progestin rather than estrogen-only therapy. Consequently, the use of hormonal therapy in management of osteoporosis was restricted to second-line by health authorities worldwide.
Chronic administration of selective estrogen receptor modulators such as raloxifene, reduces the risk of estrogen receptor positive breast cancer but increases the risk of venous thromboembolism and of fatal stroke (29).
The safety profile of bisphosphonates has been extensively investigated over the last two decades (30). The most common adverse events are gastrointestinal side effects for oral administration and acute influenza-like symptoms for intravenous administration. This route of administration may lead also to renal toxicity, possibly related to rapid infusion rates of high doses of bisphosphonates in subjects with impaired renal function. Adequate hydration prior to treatment and careful control of infusion rates are advocated, and under these circumstances renal toxicity is rare in patients with preserved renal function (30).
Causality between bisphosphonate administration and esophageal cancer, and atrial fibrillation has not been proven (31) while atypical femur fractures and osteonecrosis of the jaw (ONJ) have been considered strongly related with long term bisphosphonate treatment. The risk of ONJ is quite high in patients given cumulative high doses of bisphosphonates while its incidence in patients with osteoporosis is much lower, possibly related with exposure duration (31).
A potential association between prolonged bisphosphonate use and increased risk of atypical (subtrochanteric and femoral shaft) femur fractures has recently been identified and discussed by health authorities (32). It was stated that the risk of atypical subtrochanteric femur fractures increases by twofold after long-term exposure to bisphosphonates (more than 5 years) but that the number of atypical subtrochanteric fractures in association with bisphosphonates is small (an estimated 1 per 1 000 per year) (33). Owing to the well documented reduction of osteoporotic hip fractures in patients receiving treatment, the available evidence indicates that the benefit of preventing osteoporotic fractures in patients with osteoporosis over 3 to 5 years considerably outweighs the potential risk of atypical fractures (33). The risks and benefits for longer-term therapy remains uncertain and should be esteemed also taking into consideration the issue addressed in this review regarding the “tail effect” of some bisphosphonates.
The safety profile of Denosumab is still relatively limited since has only been available to physicians for 3–4 years. The concern regarding a potential negative effect on the immune system remains conjectural but an extended pharmacovigilance is still warranted. ONJ has been reported in patients in the extension study of FREEDOM (34). As with zoledronic acid, high-dose denosumab treatment for cancer was associated with higher rates of ONJ than that with osteoporosis doses (35). No cases of atypical femur fractures have been reported, but data are limited to 5 years in the FREEDOM extension and are only a short time postmarketing.
The treatment duration of teriparatide was fixed first to18 months and then to 24 months. The original reason for this was the observation of an increased risk of osteosarcomas in rats after long-term exposure to the drug. Recently a US post-marketing surveillance study, after 10 years of use, did not support any relationship between teriparatide treatment and osteosarcoma in humans (36,37). Additionally, there is an issue of bone safety with long-term treatment using bone anabolic agents, which might favour bone growth at sites where it is not desirable (osteophytes). Similar concerns regarding the long-term use are shared by the new anabolic drugs under development, such as anti-sclerostin antibodies.
The safety profile of strontium ranelate has been updated after the EMA found that its use in postmenopausal osteoporotic women increases the risk of serious heart problems. These new findings were of particular concern in view of previous findings of increased incidence of venous thromboembolism in people taking strontium ranelate (38).
Discussion
The impact of treatment discontinuation in postmenopausal osteoporosis varies in relation to the adopted treatment. Five distinct scenarios should be considered.
Teriparatide-PTH1-84 discontinuation
There is agreement on the need to start treatment with anti-reabsorptive drugs soon after the treatment course with Teriparatide serves to preserve the acquired benefits (39,40).
Denosumab discontinuation
In patients treated with Denosumab, treatment discontinuation is followed by a rebound of bone turnover with an impact on fracture risk that is poorly understood (41). In patients at very high risk, it is appropriate to recommend a therapeutic course with bisphosphonates immediately after Denosumab discontinuation, if a rebound in fracture rate is of concern.
Estrogens or SERMS discontinuation
After discontinuation of hormones, bone turnover and BMD return to pre-treatment levels within a few weeks. Therefore, a re-assessment of fracture risk is warranted in order to verify the opportunity to start an alternative treatment.
Ibandronate and Risedronate discontinuation
The “tail effect” of these bisphosphonates is relatively limited and bone turnover and BMD levels return to baseline levels within a year. If an interruption of the treatment is planned (for example for a surgical or a dental operation) this should not exceed 6 months in patients at high risk of fracture.
Alendronate or Zoledronate discontinuation
ALN and ZOL are among the drugs with the largest body of evidence that they reduce the risk of all kinds of fractures. These are also the drugs with the most persistent “tail effect” concerning bone turnover, BMD values, and fracture risk. The anti-fracture efficacy is partially lost after treatment discontinuation for vertebral fractures, while the protection is extended for at least two years for the risk of non-vertebral fractures. Therefore, for these two drugs, treatment discontinuation is conceivable.
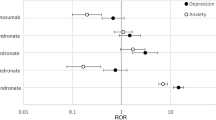
The selection of patients suitable for a period of drug holiday has recently been addressed by the NIH (USA). As we have seen, with treatment discontinuation, vertebral fracture risk is slightly increased, with the Relative Risk (Figure 11) rising by 50% for both ALN and ZOL versus subjects who continue treatment. However, the Absolute Reduction, and therefore the NNT (the number of patients to treat for preventing a fracture) depends on the original risk of fracture. For ALN, in the whole population included in the FLEX trial (9), the NNT was 34. However, in subjects at high risk, (those with previous vertebral or femoral fracture or BMD values<−3.0) the NNT is merely 17 (Figure 11). In high risk patients (Figure 4) the extension of treatment grants also a significantly higher level of protection from non-vertebral fractures (10).
These evaluations are the basis of the recommendations recently published by NIH (3). Treatment with ALN or ZOL may be interrupted after 3–5 years, only in patients in whom fracture risk is low or lowered because of the treatment itself. It is recommended to never discontinue treatment in patients with one or more prevalent osteoporotic fractures or in whom the BMD values are still below −2.5 (T score).
The NIH recommendations do not take into consideration treatment adherence (3). By assuming that, after 5 years of continuous treatment with either ZOL or ALN with full adherence, one year of drug discontinuation is recommended, but with an adherence < 80%, treatment should never be discontinued.
The duration of the interruption after five or more years of treatment with either ALN or ZOL should be planned on an individual basis. It is generally recommended (3,41) that BMD values be reassessed after 1–2 years. However, one should recognize that BMD changes over a short lag time on an individual basis are often inaccurate (42). In addition, the relationship between BMD changes and fracture risk is still debated. Most of the anti-fracture efficacy of all anti-resorptive reaches its peak within less than a year (39), while the maximum BMD increases are achieved within two or more years, depending on the drug and on the skeletal site. Thus, the anti-fracture efficacy seems to be related more to the degree of suppression of bone turnover, than to BMD changes (2), which are mostly related to increased mineralization of the existing bone tissue rather than increased bone mass (43). Thus, in individual patients in whom a discontinuation of ZOL or ALN treatment is recommended, the duration of this drug holiday should be more accurately monitored by measuring biochemical markers of bone turnover. Since, in the available ALN studies, bone turnover rises to values close to baseline 12 months after discontinuing treatment, it appears more appropriate to resume anti-resorptive treatment after 8–12 months, at least in patients with moderate to high risk of fracture
The discontinuation period for ZOL cannot be easily established, but it may exceed a year (therefore more than two years since last infusion).
Conclusions
The pharmacological treatment for postmenopausal osteoporosis is justified only for patients at very high risk of fracture and when benefits out-weight the risks associated with treatment. This benefits/risks ratio changes with treatment duration. After a few years of treatment fracture risk decreases while the risk of side effects is increasing. Thus, the incidence of two important side effects of treatment with bisphosphonates and denosumab, osteonecrosis of the jaw (ONJ) and atypical fractures (44), increases with duration of treatment and this should be taken into account while esteeming the benefits/risks balance after a few years of treatment and a drug holiday may be considered, persisting with supplementation with calcium and vitamin D and reduction of lifestyle risk factors.
The decision to discontinue treatment depends also on the drug used and on the re-assessment of fracture risk after at least 3–5 years of treatment. A treatment course with Teriparatide must always be followed by therapy with anti-reabsorptives (e.g.: bisphosphonates). Denosumab should never be discontinued; however, if discontinuation occurs, a treatment course with bisphosphonates should be considered in order to prevent the rebound of bone turnover. Discontinuation of estrogens, SERMs, RIS, and Ibandronate is associated with the quick loss of the acquired benefits, and therefore the discontinuation should never exceed 6 months.
Treatment with ALN and ZOL is characterized by an important “tail effect”. Thus, after five years of optimal adherence, a treatment discontinuation might be planned in low-moderate risk patients, but the treatment holiday should rarely exceed 1–2 years with ALN and ZOL, respectively.
References
Adami S, Bertoldo F, Brandi ML, Cepollaro C, Filipponi P, Fiore E, Frediani B, Giannini S, Gonnelli S, Isaia GC, Luisetto G, Mannarino E, Marcocci C, Masi L, Mereu C, Migliaccio S, Minisola S, Nuti R, Rini G, Rossini M, Varenna M, Ventura L, Bianchi G . Guidelines for the diagnosis, prevention and treatment of osteoporosis. Reumatismo. 2009;61:260–284.
Whitaker M, Guo J, Kehoe T, Benson G . Bisphosphonates for osteoporosis-Where do we go from here? N Engl J Med. 2012;366:2048–2051.
Black DM, Bauer DC, Schwartz AV, Cummings SR, Rosen CJ . Continuing bisphosphonate treatment for osteoporosis—for whom and for how long? N Engl J Med. 2012;366:2051–2053.
Liberman UA, Weiss SR, Bröll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW Jr., Dequeker J, Favus M . Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med. 1995;333:1437–1443.
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA ; Alendronate Phase III Osteoporosis Treatment Study Group. Ten years' experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004;350:1189–1199.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE . Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541.
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR ; Fracture Intervention Trial. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–4124.
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR ; FLEX Research Group. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927–2938.
Schwartz AV, Bauer DC, Cummings SR, Cauley JA, Ensrud KE, Palermo L, Wallace RB, Hochberg MC, Feldstein AC, Lombardi A, Black DM ; FLEX Research Group. Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res. 2010;25:976–982.
McNabb BL, Vittinghoff E, Schwartz AV, Eastell R, Bauer DC, Ensrud K, Rosenberg E, Santora A, Barrett-Connor E, Black DM . BMD changes and predictors of increased bone loss in postmenopausal women after a 5-year course of alendronate. J Bone Miner Res. 2013;28:1319–1327.
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY ; Hip Intervention Program Study Group. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344:333–340.
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD . Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–1352.
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R . Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int. 2000;11:83–91.
Watts NB, Chines A, Olszynski WP, McKeever CD, McClung MR, Zhou X, Grauer A . Fracture risk remains reduced one year after discontinuation of risedronate. Osteoporos Int. 2008;19:365–372.
Eastell R, Hannon RA, Wenderoth D, Rodriguez-Moreno J, Sawicki A . Effect of stopping risedronate after long-term treatment on bone turnover. J Clin Endocrinol Metab. 2011;96:3367–3373.
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR ; HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822.
Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R . The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27:243–254.
Reid IR, Black DM, Eastell R, Bucci-Rechtweg C, Su G, Hue TF, Mesenbrink P, Lyles KW, Boonen S ; HORIZON Pivotal Fracture Trial and HORIZON Recurrent Fracture Trial Steering Committees. Reduction in the risk of clinical fractures after a single dose of zoledronic Acid 5 milligrams. J Clin Endocrinol Metab. 2013;98:557–563.
Ravn P, Christensen JO, Baumann M, Clemmesen B . Changes in biochemical markers and bone mass after withdrawal of ibandronate treatment: prediction of bone mass changes during treatment. Bone. 1998;22:559–564.
Naylor KE, Clowes JA, Finigan J, Paggiosi MA, Peel NF, Eastell R . The effect of cessation of raloxifene treatment on bone turnover in postmenopausal women. Bone. 2010;46:592–597.
Bone HG, Bolognese MA, Yuen CK, Kendler DL, Miller PD, Yang YC, Grazette L, San Martin J, Gallagher JC . Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J Clin Endocrinol Metab. 2011;96:972–980.
Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD, Cannata J, Balogh A, Lemmel EM, Pors-Nielsen S, Rizzoli R, Genant HK, Reginster JY . The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–468.
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH . Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441.
Gatti D, Viapiana O, Idolazzi L, Fracassi E, Rossini M, Adami S . The waning of teriparatide effect on bone formation markers in postmenopausal osteoporosis is associated with increasing serum levels of DKK1. J Clin Endocrinol Metab. 2011;96:1555–1559.
Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, Blosch CM, Mathisen AL, Morris SA, Marriott TB ; Treatment of Osteoporosis with Parathyroid Hormone Study Group. Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med. 2007;146:326–339.
Lindsay R, Scheele WH, Neer R, Pohl G, Adami S, Mautalen C, Reginster JY, Stepan JJ, Myers SL, Mitlak BH . Sustained vertebral fracture risk reduction after withdrawal of teriparatide in postmenopausal women with osteoporosis. Arch Intern Med. 2004;164:2024–2030.
Adami S, San Martin J, Muñoz-Torres M, Econs MJ, Xie L, Dalsky GP, McClung M, Felsenberg D, Brown JP, Brandi ML, Sipos A . Effect of raloxifene after recombinant teriparatide [hPTH(1–34)] treatment in postmenopausal women with osteoporosis. Osteoporos Int. 2008;19:87–94.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J ; Writing Group for the Women's Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321–333.
Mosca L, Grady D, Barrett-Connor E, Collins P, Wenger N, Abramson BL, Paganini-Hill A, Geiger MJ, Dowsett SA, Amewou-Atisso M, Kornitzer M . Effect of raloxifene on stroke and venous thromboembolism according to subgroups in postmenopausal women at increased risk of coronary heart disease. Stroke. 2009;40:147–155.
Adami S, Zamberlan N . Adverse effects of bisphosphonates. A comparative review. Drug Saf. 1996;14:158–170.
Abrahamsen B . Adverse effects of bisphosphonates. Calcif Tissue Int. 2010;86:421–435.
US Food and Drug Administration (FDA). Zoledronic acid for osteoporosis (marketed as Reclast): renal impairment and acute renal failure. Drug Safety Newsletter. 2009;2:13–15.
Rizzoli R, Reginster JY, Boonen S, Bréart G, Diez-Perez A, Felsenberg D, Kaufman JM, Kanis JA, Cooper C . Adverse reactions and drug-drug interactions in the management of women with postmenopausal osteoporosis. Calcif Tissue Int. 2011;89:91–104.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C ; FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765.
Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, Jiang Q, Tadros S, Dansey R, Goessl C . Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377:813–822.
Andrews EB, Gilsenan AW, Midkiff K, Sherrill B, Wu Y, Mann BH, Masica D . The US postmarketing surveillance study of adult osteosarcoma and teriparatide: study design and findings from the first 7 years. J Bone Miner Res. 2012;27:2429–2437.
Cipriani C, Irani D, Bilezikian JP . Safety of osteoanabolic therapy: a decade of experience. J Bone Miner Res. 2012;27:2419–2428.
European Medicines Agency. Recommendation to restrict the use of Protelos/Osseor (strontium ranelate). 2013. http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2013/04/WC500142507.pdf
Brown JP, Roux C, Törring O, Ho PR, Beck Jensen JE, Gilchrist N, Recknor C, Austin M, Wang A, Grauer A, Wagman RB . Discontinuation of denosumab and associated fracture incidence: analysis from the Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Months (FREEDOM) trial. J Bone Miner Res. 2013;28:746–752.
Papapoulos SE . Bone diseases: Bisphosphonates in osteoporosis-beyond 5 years. Nat Rev Rheumatol. 2013;9:263–264.
Writing Group for the ISCD Position Development Conference. Indications and reporting for dual-energy x-ray absorptiometry. J Clin Densitom. 2004;7:37–44.
Roux C, Seeman E, Eastell R, Adachi J, Jackson RD, Felsenberg D, Songcharoen S, Rizzoli R, Di Munno O, Horlait S, Valent D, Watts NB . Efficacy of risedronate on clinical vertebral fractures within six months. Curr Med Res Opin. 2004;20:433–439.
Boivin GY, Chavassieux PM, Santora AC, Yates J, Meunier PJ . Alendronate increases bone strength by increasing the mean degree of mineralization of bone tissue in osteoporotic women. Bone. 2000;27:687–694.
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP . Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29:1–23.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adami, S., Idolazzi, L., Fracassi, E. et al. Osteoporosis Treatment: When to Discontinue and When to Re-start. Bone Res 1, 323–335 (2013). https://doi.org/10.4248/BR201304003
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.4248/BR201304003
This article is cited by
-
Anti-resorptive therapy in the osteometabolic patient affected by periodontitis. A joint position paper of the Italian Society of Orthopaedics and Traumatology (SIOT) and the Italian Society of Periodontology and Implantology (SIdP)
Journal of Orthopaedics and Traumatology (2023)
-
Polylactic acid reinforced with nano-hydroxyapatite bioabsorbable cortical screws for bone fracture treatment
Journal of Polymer Research (2023)
-
Deprescribing: Right-Sizing Medication Regimens to Optimize Outcomes in Palliative Care
Current Geriatrics Reports (2019)
-
Multiple Vertebral Osteonecroses (Kümmell’s Disease) After 10 Years on Denosumab: Is Osteocyte Apoptosis to Blame?
Calcified Tissue International (2018)
-
GRAND-4: the German retrospective analysis of long-term persistence in women with osteoporosis treated with bisphosphonates or denosumab
Osteoporosis International (2016)