Abstract
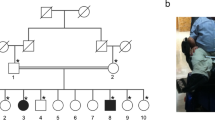
Autosomal recessive lethal and severe osteogenesis imperfecta (OI) is caused by the deficiency of cartilage-associated protein (CRTAP) and prolyl-3-hydroxylase 1 (P3H1) because of CRTAP and LEPRE1 mutations. We analyzed five families in which 10 individuals had a clinical diagnosis of lethal and severe OI with an overmodification of collagen type I on biochemical testing and without a mutation in the collagen type I genes. CRTAP mutations not described earlier were identified in the affected individuals. Although it seems that one important feature of autosomal recessive OI due to CRTAP mutations is the higher consistency of radiological features with OI type II-B/III, differentiation between autosomal dominant and autosomal recessive OI on the basis of clinical, radiological and biochemical investigations proves difficult in the affected individuals reported here. These observations confirm that once a clinical diagnosis of OI has been made in an affected individual, biochemical testing for overmodification of collagen type I should always be combined with molecular genetic analysis of the collagen type I genes. If no mutations in the collagen type I genes are found, additional molecular genetic analysis of the CRTAP and LEPRE1 genes should follow. This approach will allow proper identification of the genetic cause of lethal or severe OI, which is important in providing prenatal diagnosis, preimplantation genetic diagnosis and estimating recurrence risk.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Baljet B : Aspects of the history of osteogenesis imperfecta (Vrolik's syndrome). Ann Anat 2002; 184: 1–7.
Sillence DO, Senn A, Danks DM : Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 1979; 16: 101–116.
Sillence DO, Barlow KK, Garber AP, Hall JG, Rimoin DL : Osteogenesis imperfecta type II delineation of the phenotype with reference to genetic heterogeneity. Am J Med Genet 1984; 17: 407–423.
Young ID, Thompson EM, Hall CM, Pembrey ME : Osteogenesis imperfecta type IIA: evidence for dominant inheritance. J Med Genet 1987; 24: 386–389.
Thompson EM, Young ID, Hall CM, Pembrey ME : Recurrence risks and prognosis in severe sporadic osteogenesis imperfecta. J Med Genet 1987; 24: 390–405.
Chu ML, Williams CJ, Pepe G, Hirsch JL, Prockop DJ, Ramirez F : Internal deletion in a collagen gene in a perinatal lethal form of osteogenesis imperfecta. Nature 1983; 304: 78–80.
Cohn DH, Starman BJ, Blumberg B, Byers PH : Recurrence of lethal osteogenesis imperfecta due to parental mosaicism for a dominant mutation in a human type I collagen gene (COL1A1). Am J Hum Genet 1990; 46: 591–601.
Cohen-Solal L, Bonaventure J, Maroteaux P : Dominant mutations in familial lethal and severe osteogenesis imperfecta. Hum Genet 1991; 87: 297–301.
Byers PH, Tsipouras P, Bonadio JF, Starman BJ, Schwartz RC : Perinatal lethal osteogenesis imperfecta (OI type II): a biochemically heterogeneous disorder usually due to new mutations in the genes for type I collagen. Am J Hum Genet 1988; 42: 237–248.
Byers PH, Wallis GA, Willing MC : Osteogenesis imperfecta: translation of mutation to phenotype. J Med Genet 1991; 28: 433–442.
Wallis GA, Sykes B, Byers PH, Mathew CG, Viljoen D, Beighton P : Osteogenesis imperfecta type III: mutations in the type I collagen structural genes, COL1A1 and COL1A2, are not necessarily responsible. J Med Genet 1993; 30: 492–496.
Rauch F, Glorieux FH : Osteogenesis imperfecta. Lancet 2004; 363: 1377–1385.
Ward LM, Rauch F, Travers R et al: Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone 2002; 31: 12–18.
Morello R, Bertin TK, Chen Y, Hicks J, Tonachini L, Monticone M. et al. CRTAP is required for Prolyl 3-Hydroxylation and mutations cause recessive osteogenesis imperfecta. Cell 2006; 127: 291–304
Barnes AM, Chang W, Morello R et al: Deficiency of cartilage-associated protein in recessive lethal osteogenesis imperfecta. N Engl J Med 2006; 355: 2757–2764.
Cabral WA, Chang W, Barnes AM et al: Prolyl 3-hydroxylase 1 deficiency causes a recessive metabolic bone disorder resembling lethal/severe osteogenesis imperfecta. Nat Genet 2007; 39: 359–365.
Marini JC, Cabral WA, Barnes AM, Chang W : Components of the collagen prolyl 3-hydroxylation complex are crucial for normal bone development. Cell Cycle 2007; 6: 1675–1681.
Prockop DJ, Constantinou CD, Dombrowski KE et al: Type I procollagen: the gene-protein system that harbors most of the mutations causing osteogenesis imperfecta and probably more common heritable disorders of connective tissue. Am J Med Genet 1989; 34: 60–67.
Canty EG, Kadler KE : Procollagen trafficking, processing and fibrillogenesis. J Cell Sci 2005; 118: 1341–1353.
Trackman PC : Diverse biological functions of extracellular collagen processing enzymes. J Cell Biochem 2005; 96: 927–937.
Korkko J, la-Kokko L, De PA, Nuytinck L, Earley J, Prockop DJ : Analysis of the COL1A1 and COL1A2 genes by PCR amplification and scanning by conformation-sensitive gel electrophoresis identifies only COL1A1 mutations in 15 patients with osteogenesis imperfecta type I: identification of common sequences of null-allele mutations. Am J Hum Genet 1998; 62: 98–110.
Baldridge D, Schwarze U, Morello R et al: CRTAP and LEPRE1 mutations in recessive osteogenesis imperfecta. Hum Mutat 2008; 29: 1435–1442.
Spotila LD, Colige A, Sereda L et al: Mutation analysis of coding sequences for type I procollagen in individuals with low bone density. J Bone Miner Res 1994; 9: 923–932.
Cole WG, Chan D, Chow CW, Rogers JG, Bateman JF : Disrupted growth plates and progressive deformities in osteogenesis imperfecta as a result of the substitution of glycine 585 by valine in the alpha 2 (I) chain of type I collagen. J Med Genet 1996; 33: 968–971.
Obafemi AA, Bulas DI, Troendle J, Marini JC : Popcorn calcifications in osteogenesis imperfecta: incidence, progression and molecular correlation. Am J Med Gen A Sept 2008; 146A: 2725–2732.
Nikkels PGJ : The skeletal system; in Keeling JW, Kong TY (eds): Fetal and Neonatal Pathology, 4 edn. Springer, 2008. pp 770–795.
Acknowledgements
We thank the parents for their kind cooperation and we thank clinical geneticist, JJ van der Smagt, at the Department of Clinical Genetics, University Medical Center Utrecht, The Netherlands for his advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
Supplementary information
Rights and permissions
About this article
Cite this article
Van Dijk, F., Nesbitt, I., Nikkels, P. et al. CRTAP mutations in lethal and severe osteogenesis imperfecta: the importance of combining biochemical and molecular genetic analysis. Eur J Hum Genet 17, 1560–1569 (2009). https://doi.org/10.1038/ejhg.2009.75
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ejhg.2009.75
Keywords
This article is cited by
-
MBTPS2, a membrane bound protease, underlying several distinct skin and bone disorders
Journal of Translational Medicine (2021)
-
Collagen transport and related pathways in Osteogenesis Imperfecta
Human Genetics (2021)
-
Evidence for a de novo, dominant germ-line mutation causative of osteogenesis imperfecta in two Red Angus calves
Mammalian Genome (2019)
-
Comparison of Bone Microarchitecture Between Adult Osteogenesis Imperfecta and Early-Onset Osteoporosis
Calcified Tissue International (2018)
-
Comparative X-ray morphometry of prenatal osteogenesis imperfecta type 2 and thanatophoric dysplasia: a contribution to prenatal differential diagnosis
La radiologia medica (2017)