Abstract
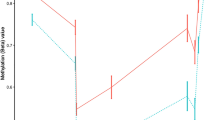
Recently, constitutional MLH1 epimutations have been identified in a subset of Lynch syndrome (LS) cases. The aim of this study was the identification of patients harboring constitutional MLH1 epimutations in a set of 34 patients with a clinical suspicion of LS, MLH1-methylated tumors and non-detected germline mutations in mismatch repair (MMR) genes. MLH1 promoter methylation was analyzed in lymphocyte DNA samples by MS-MLPA (Methylation-specific multiplex ligation-dependent probe amplification). Confirmation of MLH1 constitutional methylation was performed by MS-MCA (Methylation-specific melting curve analysis), bisulfite sequencing and pyrosequencing in different biological samples. Allelic expression was determined using heterozygous polymorphisms. Vertical transmission was evaluated by MS-MLPA and haplotype analyses. MS-MLPA analysis detected constitutional MLH1 methylation in 2 of the 34 individuals whose colorectal cancers showed MLH1 methylation (5.9%). These results were confirmed by bisulfite-based methods. Both epimutation carriers had developed metachronous early-onset LS tumors, with no family history of LS-associated cancers in their first-degree relatives. In one of the cases, the identified MLH1 constitutional methylation was monoallelic and results in MLH1 and EPM2AIP1 allele-specific transcriptional silencing. It was present in normal somatic tissues and absent in spermatozoa. The methylated MLH1 allele was maternally transmitted and methylation was reversed in a daughter who inherited the same allele. MLH1 methylation screening in lymphocyte DNA from patients with early-onset MLH1-methylated LS-associated tumors allows the identification of epimutation carriers. The present study adds further evidence to the emerging entity of soma-wide MLH1 epimutation and its heritability.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Accession codes
References
Lynch HT, Lynch JF, Lynch PM, Attard T : Hereditary colorectal cancer syndromes: molecular genetics, genetic counseling, diagnosis and management. Fam Cancer 2008; 7: 27–39.
Vasen HF, Moslein G, Alonso A et al: Guidelines for the clinical management of Lynch syndrome (hereditary non-polyposis cancer). J Med Genet 2007; 44: 353–362.
Marra G, Boland CR : Hereditary nonpolyposis colorectal cancer: the syndrome, the genes, and historical perspectives. J Natl Cancer Inst 1995; 87: 1114–1125.
Peltomaki P, Vasen H : Mutations associated with HNPCC predisposition -- update of ICG-HNPCC/INSiGHT mutation database. Dis Markers 2004; 20: 269–276.
Hitchins MP, Ward RL : Constitutional (germline) MLH1 epimutation as an aetiological mechanism for hereditary non-polyposis colorectal cancer. J Med Genet 2009; 46: 793–802.
Kuiper RP, Vissers LE, Venkatachalam R et al: Recurrence and variability of germline EPCAM deletions in Lynch syndrome. Hum Mutat 2011; 32: 407–414.
Hesson LB, Hitchins MP, Ward RL : Epimutations and cancer predisposition: importance and mechanisms. Curr Opin Genet Dev 2010; 20: 290–298.
Ligtenberg MJ, Kuiper RP, Chan TL et al: Heritable somatic methylation and inactivation of MSH2 in families with Lynch syndrome due to deletion of the 3′ exons of TACSTD1. Nat Genet 2009; 41: 112–117.
Auclair J, Vaissiere T, Desseigne F et al: Intensity-dependent constitutional MLH1 promoter methylation leads to early onset of colorectal cancer by affecting both alleles. Genes Chromosomes Cancer 2011; 50: 178–185.
Crepin M, Dieu MC, Lejeune S et al: Evidence of constitutional MLH1 epimutation associated to transgenerational inheritance of cancer susceptibility. Hum Mutat 2012; 33: 180–188.
Gazzoli I, Loda M, Garber J, Syngal S, Kolodner RD : A hereditary nonpolyposis colorectal carcinoma case associated with hypermethylation of the MLH1 gene in normal tissue and loss of heterozygosity of the unmethylated allele in the resulting microsatellite instability-high tumor. Cancer Res 2002; 62: 3925–3928.
Goel A, Nguyen TP, Leung HC et al: De novo constitutional MLH1 epimutations confer early-onset colorectal cancer in two new sporadic Lynch syndrome cases, with derivation of the epimutation on the paternal allele in one. Int J Cancer 2011; 128: 869–878.
Gylling A, Ridanpaa M, Vierimaa O et al: Large genomic rearrangements and germline epimutations in Lynch syndrome. Int J Cancer 2009; 124: 2333–2340.
Hitchins M, Owens S, Kwok CT, Godsmark G, Algar U, Ramesar R : Identification of new cases of early-onset colorectal cancer with an MLH1 epimutation in an ethnically diverse South African cohort. Clin Genet 2011; 80: 428–434.
Hitchins M, Williams R, Cheong K et al: MLH1 germline epimutations as a factor in hereditary nonpolyposis colorectal cancer. Gastroenterology 2005; 129: 1392–1399.
Hitchins MP, Rapkins RW, Kwok CT et al: Dominantly inherited constitutional epigenetic silencing of MLH1 in a cancer-affected family is linked to a single nucleotide variant within the 5′UTR. Cancer Cell 2011; 20: 200–213.
Hitchins MP, Wong JJ, Suthers G et al: Inheritance of a cancer-associated MLH1 germ-line epimutation. N Engl J Med 2007; 356: 697–705.
Miyakura Y, Sugano K, Akasu T et al: Extensive but hemiallelic methylation of the hMLH1 promoter region in early-onset sporadic colon cancers with microsatellite instability. Clin Gastroenterol Hepatol 2004; 2: 147–156.
Morak M, Koehler U, Schackert HK et al: Biallelic MLH1 SNP cDNA expression or constitutional promoter methylation can hide genomic rearrangements causing Lynch syndrome. J Med Genet 2011; 48: 513–519.
Morak M, Schackert HK, Rahner N et al: Further evidence for heritability of an epimutation in one of 12 cases with MLH1 promoter methylation in blood cells clinically displaying HNPCC. Eur J Hum Genet 2008; 16: 804–811.
Suter CM, Martin DI, Ward RL : Germline epimutation of MLH1 in individuals with multiple cancers. Nat Genet 2004; 36: 497–501.
Valle L, Carbonell P, Fernandez V et al: MLH1 germline epimutations in selected patients with early-onset non-polyposis colorectal cancer. Clin Genet 2007; 71: 232–237.
van Roon EH, van Puijenbroek M, Middeldorp A et al: Early onset MSI-H colon cancer with MLH1 promoter methylation, is there a genetic predisposition? BMC Cancer 2010; 10: 180.
Gausachs M, Mur P, Corral J et al: MLH1 promoter hypermethylation in the analytical algorithm of Lynch syndrome: a cost-effectiveness study. Eur J Hum Genet 2012 (in press).
Dausset J, Cann H, Cohen D, Lathrop M, Lalouel JM, White R : Centre d’etude du polymorphisme humain (CEPH): collaborative genetic mapping of the human genome. Genomics 1990; 6: 575–577.
Deng G, Peng E, Gum J, Terdiman J, Sleisenger M, Kim YS : Methylation of hMLH1 promoter correlates with the gene silencing with a region-specific manner in colorectal cancer. Br J Cancer 2002; 86: 574–579.
Azuara D, Rodriguez-Moranta F, de Oca J et al: Novel methylation panel for the early detection of colorectal tumors in stool DNA. Clin Colorectal Cancer 2010; 9: 168–176.
Mueller J, Gazzoli I, Bandipalliam P, Garber JE, Syngal S, Kolodner RD : Comprehensive molecular analysis of mismatch repair gene defects in suspected Lynch syndrome (hereditary nonpolyposis colorectal cancer) cases. Cancer Res 2009; 69: 7053–7061.
Borras E, Pineda M, Blanco I et al: MLH1 founder mutations with moderate penetrance in Spanish Lynch syndrome families. Cancer Res 2010; 70: 7379–7391.
Hitchins MP, Ward RL : Erasure of MLH1 methylation in spermatozoa-implications for epigenetic inheritance. Nat Genet 2007; 39: 1289.
Whiffin N, Broderick P, Lubbe SJ et al: MLH1-93G>A is a risk factor for MSI colorectal cancer. Carcinogenesis 2011; 32: 1157–1161.
Allan JM, Shorto J, Adlard J et al: MLH1 -93G>A promoter polymorphism and risk of mismatch repair deficient colorectal cancer. Int J Cancer 2008; 123: 2456–2459.
Chen H, Taylor NP, Sotamaa KM et al: Evidence for heritable predisposition to epigenetic silencing of MLH1. Int J Cancer 2007; 120: 1684–1688.
Mrkonjic M, Roslin NM, Greenwood CM et al: Specific variants in the MLH1 gene region may drive DNA methylation, loss of protein expression, and MSI-H colorectal cancer. PLoS One 2010; 5: e13314.
Campbell PT, Curtin K, Ulrich CM et al: Mismatch repair polymorphisms and risk of colon cancer, tumour microsatellite instability and interactions with lifestyle factors. Gut 2009; 58: 661–667.
Perera S, Mrkonjic M, Rawson JB, Bapat B : Functional effects of the MLH1-93G>A polymorphism on MLH1/EPM2AIP1 promoter activity. Oncol Rep 2011; 25: 809–815.
Perez-Carbonell L, Alenda C, Paya A et al: Methylation analysis of MLH1 improves the selection of patients for genetic testing in Lynch syndrome. J Mol Diagn 2010; 12: 498–504.
Acknowledgements
We thank the patients who participated in this study, Gemma Aiza for technical assistance, Javier Carmona for his assistance with pyrosequencing and Dr Juana Fernández for her assistance in skin fibroblast isolation and culture. This work was supported by grants from Ministerio de Ciencia e Innovación (SAF 06-06084; 09-07319), Fundació Gastroenterologia Dr Francisco Vilardell (F05-01), Ministerio de Educación y Ciencia Spanish Networks RTICCC (RD06/0020/1050, 1051), Acción en Cáncer (Instituto de Salud Carlos III), Fundación Científica AECC and NCI U19 CA 148107-02.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Pineda, M., Mur, P., Iniesta, M. et al. MLH1 methylation screening is effective in identifying epimutation carriers. Eur J Hum Genet 20, 1256–1264 (2012). https://doi.org/10.1038/ejhg.2012.136
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ejhg.2012.136
Keywords
This article is cited by
-
Identifying primary and secondary MLH1 epimutation carriers displaying low-level constitutional MLH1 methylation using droplet digital PCR and genome-wide DNA methylation profiling of colorectal cancers
Clinical Epigenetics (2023)
-
Highly sensitive MLH1 methylation analysis in blood identifies a cancer patient with low-level mosaic MLH1 epimutation
Clinical Epigenetics (2019)
-
Primary constitutional MLH1 epimutations: a focal epigenetic event
British Journal of Cancer (2018)
-
Prevalence and clinicopathologic/molecular characteristics of mismatch repair-deficient colorectal cancer in the under-50-year-old Japanese population
Surgery Today (2017)
-
Finding the needle in a haystack: identification of cases of Lynch syndrome with MLH1 epimutation
Familial Cancer (2016)