Abstract
Purpose
Glaucoma is initially asymptomatic, but untreated can result in progressive visual field loss and eventual blindness. With adequate therapy progression can be halted, but poor adherence with medical therapy is a significant issue requiring further research. The aim of the present study was to gain a better understanding of the obstacles to, and the motivations for, adherence with glaucoma medication and explore potential methods to improve adherence.
Methods
Participants had moderate/severe glaucoma diagnosed for >1 year, had seen ⩾2 NHS ophthalmologists, and were prescribed ⩾2 topical medications. Qualitative methodology was utilized to investigate aspects of adherence. Recruited patients either attended a focus group or had a home-based semi-structured interview. The transcripts were member-checked and the resulting data were analysed using ‘Framework’ analysis. The analysis was verified by a co-investigator and NVIVO Software was used to check data reliability.
Results
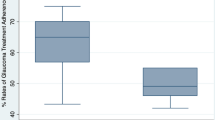
Multiple obstacles to adherence were identified, including poor education, lack of motivation, forgetfulness, drop application, and other practical issues, together with specific individual and age differences. Motivation for adherence was determined by fear of blindness and a faith in drop efficacy.
Conclusions
Specific obstacles to adherence with anti-glaucomatous therapy should be identified as early as possible after diagnosis. A tailored approach to patient care with initial education about the consequences of non-adherence and longer-term feedback about drop efficacy may improve patients' motivations for adherence. Future research should focus on investigating methods by which initial education about glaucoma and its management should best be delivered to patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Olthoff CMG, Schouten JSAG, Bart W, Webbers CAB . Non-compliance with ocular hypertensive treatment in patients with glaucoma or ocular hypertension, an evidence based review. Ophthalmology 2005; 112: 953–960.
Ethical Strategies Ltd.. The costs of blindness. An analysis of the costs of visual impairment and blindness in the United Kingdom. [serial online] 2003 [cited 2006 Sept 30]; [1-65]. Available from URL:http://www.healthyeyes.org.uk/fileadmin/healthy-eyes/downloads/costs-of-blindness.doc.
Mitchell P, Smith W, Attebo K, Healy PT . Prevalence of open angle glaucoma in Australia: the blue mountains study. Ophthalmology 1996; 103: 1661–1669.
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW . Compliance barriers in glaucoma: a systematic classification. J Glaucoma 2003; 12: 393–398.
Quigley H, Goldberg I, Kitazawa Y, Halprin R, Hitchings R, Gross R et al. Cooperation with medical therapy, report from the global AIGS committee on cooperation with therapy. In: Greve EL (ed). International Glaucoma Review, Supplement 2006, vol. 7. Kugler Publications: The Netherlands, 2006, pp 354–359.
Green J, Britten N . Qualitative research and evidence based medicine. BMJ 1998; 316: 1230–1232.
Taylor SA, Galbraith SM, Mills RP . Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther 2002; 18: 401–409.
Lincoln YS, Guba EG . Naturalistic Inquiry. Sage: Beverly Hills, 1985, pp 314–316.
Ritchie J, Spencer L . Qualitative data analysis for applied policy research.In: Bryman A, Burgess R (eds). Analysing Qualitative Data. Routledge: London, 1994, pp 173–194.
Armstrong D, Gosling A, Weinman J, Marteau T . The place of inter-rater reliability in qualitative research: an empirical study. Sociology 1997; 31: 597–606.
Zimmerman T, Zalta A . Facilitating patient compliance in glaucoma therapy. Surv Ophthalmol 1993; 28: 252–257.
Roth H, Caron H . Accuracy of doctors’ estimates and patients’ statements on adherence to a drug regime. Clin Pharmacol Ther 1978; 23: 361–370.
Kass M, Gordon M, Meltzer D . Can ophthalmologists correctly identify patients defaulting from pilocarpine therapy? Am J Ophthalmol 1986; 101: 524–530.
Berger BA . Improving treatment adherence (medication compliance) a motivational interviewing approach. [serial online] 2007 [cited 2007 August 10]; [1–33]. Available from URL:https://webapp.walgreens.com/cePharmacy/programsHTML/compliance.html.
Willig C . Introducing Qualitative Research in Psychology: Adventures in Theory and Method. Open University Press: Buckingham, 2001, pp 16–19.
Acknowledgements
The study was funded by the Norwich Glaucoma Research Fund. We thank Tom Eke, Consultant Ophthalmologist at the Cromer and District Hospital, for identifying suitable participants, staff at both the Norfolk and Norwich University Hospital and the Cromer and District Hospital for allowing recruitment from their clinics and, above all, the participants for their time and input.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jenny Lacey was winner of the Norfolk and Norwich Bicentenary Trust Annual Presentation Prize, August 2007 for this study. The authors had no proprietary interests relating to this study.
Rights and permissions
About this article
Cite this article
Lacey, J., Cate, H. & Broadway, D. Barriers to adherence with glaucoma medications: a qualitative research study. Eye 23, 924–932 (2009). https://doi.org/10.1038/eye.2008.103
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2008.103
Keywords
This article is cited by
-
Adherence to topical glaucoma therapy in patients attending virtual clinics
Eye (2023)
-
Treatment expectations in glaucoma: what matters most to patients?
Eye (2023)
-
Adherence and Persistence to Medical Therapy in Glaucoma: An Overview
Ophthalmology and Therapy (2023)
-
Reasons for choice of glaucoma surgery in eyes not treated with anti-glaucoma medications
BMC Ophthalmology (2022)
-
The development of a glaucoma-specific health-related quality of life item bank supporting a novel computerized adaptive testing system in Asia
Journal of Patient-Reported Outcomes (2022)