Abstract
Aims/Purpose
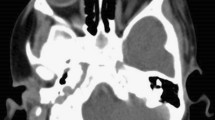
Orbital cellulitis is conventionally managed by intravenous (i.v.) antibiotic therapy, followed by oral antibiotics once the infection shows signs of significant improvement. We report 4 years of experience using primary oral ciprofloxacin and clindamycin in cases of orbital cellulitis. Oral ciprofloxacin and clindamycin have a similar bioavailability to the i.v. preparations and provide an appropriate spectrum of antibiotic cover for the pathogens responsible for orbital cellulitis.
Methods
A retrospective review was performed that identified all patients with orbital cellulitis and treated with primary oral antibiotic therapy admitted to the Manchester Royal Eye Hospital between March 2003 and March 2007. Age, stage of disease, surgical intervention, hospital duration, and complications were obtained. A comparison was made with patients admitted to our unit with orbital cellulitis and treated with primary i.v. antibiotics between March 2000 and March 2003.
Results
Nineteen patients were included in the review for the period March 2003 to March 2007, which comprised of 7 children and 12 adults. Five patients required surgical intervention. All patients responded to the oral regimen, 18 patients had no change to their oral antibiotic therapy. Mean hospital stay was 4.4 days. There were no complications.
Discussion
Empirical oral ciprofloxacin and clindamycin combination may be as safe and effective as i.v. therapy in the management of orbital cellulitis. Oral treatment can offer the advantages of rapid delivery of the first antibiotic dose, fewer interruptions in treatment, and simplified delivery of medication particularly in children.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Chandler JR, Langenbrunner DJ, Stevens ER . The pathogenesis of orbital complications in acute sinusitis. Laryngoscope 1970; 80: 1414–1428.
Smith TF, O'Day D, Wright PF . Clinical implications of preseptal (peri-orbital) cellulitis in childhood. Pediatrics 1978; 62: 1006–1009.
Nelson JD, Ginsburg CM . An hypothesis on the pathogenesis of Hemophilus influenzae buccal cellulitis. J Pediatrics 1976; 88: 709–710.
Goldberg F, Berne AS, Oski FA . Differentiation of orbital cellulitis from preseptal cellulitis by computer tomography. Pediatrics 1978; 62: 1000–1005.
Eustis HS, Armstrong DC, Buncic JR, Morin JD . Staging of orbital cellulitis in children: computerized tomography characteristics and treatment guidelines. J Pediatr Ophthalmol Strabismus 1986; 23: 246–251.
Noël LP, Clarke WN, MacDonald N . Clinical management of orbital cellulitis in children. Can J Ophthalmol 1990; 19: 109–119.
Garcia GH, Harris GJ . Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988–1998. Ophthalmol 2000; 107: 1454–1458.
Rubin SE, Rubin LG, Zito J, Goldstein MN, Eng C . Medical management of orbital subperiosteal abscess in children. J Pediatr Ophthalmol Strabismus 1989; 26: 21–26.
Nageswaran S, Woods CR, Benjamin DK, Givner LB, Shetty AK . Orbital cellulitis in children. Pediatr Infect Dis J 2006; 25: 696–699.
Bergan T, Thorsteinsson SB, Solberg R, Bjornskau L, Kolstad IM, Johnsen S . Pharmacokinetics of ciprofloxacin: intravenous and increasing oral doses. AJM 1987; 82 (4A): 97–102.
Hornblass A, Herschorn BJ, Stern K, Grimes C . Orbital abscess: review. Surv Ophthalmol 1984; 29: 169–178.
Bergin DJ, Wright JE . Orbital cellulitis. Br J Ophthalmol 1986; 70: 174–178.
Harris GJ, Garcia GH . Nonsurgical management of subperiosteal abscess of the orbit. Ophthalmol 2001; 108: 1167–1169.
Schramm VL, Curtin HD, Kennerdell JS . Evaluation of orbital cellulitis and results of treatment. Laryngoscope 1982; 92 (7): 732–738.
Weiss A, Friendly D, Eglin K . Bacterial periorbital and orbital cellulitis in childhood. Ophthalmol 1983; 90: 195–203.
Rahbar R, Robson CD, Petersen RA, DiCanzio J, Rosbe KW, McGill TJ et al. Management of orbital subperiosteal abscess in children. Arch Otolaryngol Head Neck Surg 2001; 127: 281–286.
Kagel EM, Rayan GM . Intravenous catheter complications in the hand and forearm. J Trauma 2004; 56 (1): 123–127.
Al-Nammari S, Roberton B, Ferguson C . Should a child with preseptal periorbital cellulitis be treated with intravenous or oral antibiotics? Emerg Med J 2007; 24: 128–129.
Harris GJ . Subperiosteal abscess of the orbit. Older children and adults require aggressive treatment. Ophthal Plast Reconstr Surg 2001; 17 (6): 395–397.
Ramirez-Ronda CH, Saavedra S, Rivera-Vázquez CR . Comparative, double-blind study of oral ciprofloxacin and intravenous cefotaxime in skin and skin structure infections. Am J Med 1987; 82 (4A): 220–223.
Tuncer I, Topcu N, Durmus A, Turkdogan MK . Oral ciprofloxacin versus intravenous ceftriaxone in the treatment of spontaneous bacterial peritonitis. Hepatogastroenterology 2003; 50 (53): 1426–1430.
Author information
Authors and Affiliations
Corresponding author
Additional information
Interests, financial or other: none.The authors declare no conflict of interest.
Presentations: This paper was presented at the ESOPRS meeting in Ljubljana, Slovenia in September 2007.
Rights and permissions
About this article
Cite this article
Cannon, P., Keag, D., Radford, R. et al. Our experience using primary oral antibiotics in the management of orbital cellulitis in a tertiary referral centre. Eye 23, 612–615 (2009). https://doi.org/10.1038/eye.2008.44
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2008.44
Keywords
This article is cited by
-
A case report of exudative retinal detachment derived from orbital cellulitis in mainland China
BMC Ophthalmology (2020)
-
Applying Pharmacodynamics and Antimicrobial Stewardship to Pediatric Preseptal and Orbital Cellulitis
Pediatric Drugs (2019)
-
Spontaneously resolved exudative retinal detachment caused by orbital cellulitis in an immunocompromised adult
Eye (2014)