Abstract
Purpose
To report the occurrence of a novel mechanism of IOFB with hot, liquefied glass injury.
Methods
Retrospective case series.
Results
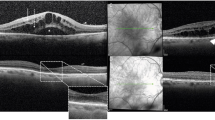
Two patients suffered an injury to their eye with hot, liquefied glass. The ocular findings included a single scleral entry wound with multiple glass fragments located inside the eye. Fragments were found embedded in the retina, as well as mobile on the retinal surface.
Conclusions
This distinctive mechanism involves an initial liquid state of glass causing injury, and results in multiple solidified glass IOFBs despite a single entrance wound. Though intraocular glass is typically inert, the unique characteristics of this injury may warrant a surgical approach. Surgical management proved successful in stabilizing vision and preventing further complications.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ghoraba H . Posterior segment glass intraocular foreign bodies following car accident or explosion. Graefe’s Arch Clin Exp Ophthalmol 2002; 240: 524–528.
Ray S, Friberg T, Beatty R, Loewenstein J . Late posterior migration of glass intraocular foreign bodies. Arch Ophthalmol 2004; 122: 923–926.
Gopal L, Banker AS, Deb N, Badrinath SS, Sharma T, Parikh SN et al. Management of glass intraocular foreign bodies. Retina 1998; 18 (3): 213–220.
Milkowski S . Rare case of spontaneous migration of intraocular glass foreign body 21 years after injury. Wiad Lek 1978; 31 (15): 1065–1069.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ittiara, S., Sanduja, N., Chiranand, P. et al. Hot, liquid glass injury as a novel mechanism for intraocular foreign body. Eye 26, 1145–1149 (2012). https://doi.org/10.1038/eye.2012.140
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2012.140