Abstract
Purpose
Limited data exist detailing the normal range of intraocular pressure (IOP) for healthy school age children. This study aims to describe the mean and normal range of IOP measurements that may be expected using the Icare rebound tonometer and to examine associations between visual function measures and IOP.
Methods
Six measurements of IOP from each eye were obtained from 211 normal children aged 6–15 years (79 females and 132 males) using the Icare tonometer. Other measures of visual function obtained included: visual acuity, non-cycloplegic retinoscopy, amplitude of accommodation, accommodative facility, and accommodative response.
Results
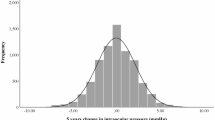
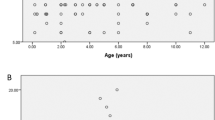
Statistical analysis (Mann–Whitney U test) demonstrated that the male subjects were more likely to have higher IOP measurements than the female subjects (mean IOP males 15.02 mm Hg (SD 2.19), mean IOP females 14.44 (SD 2.01) P=0.041). Analysis (Spearman's rho) showed a statistically significant association between age and IOP (right eye) in males (P<0.001) but no association for females (P=0.459). Using Spearman's rank analysis, statistically significant associations were found between IOP and amplitude of accommodation in males, for the whole data set (P=0.09) and for data up to age 11 (P<0.001). For females no statistically significant association was found for the whole data set (P=0.253) or for data up to age 11 (P=0.08). IOP was not significantly associated with visual acuity, refractive error, accommodative facility, or accommodative response.
Conclusion
This study provides useful normative IOP data using the Icare tonometer for a European cohort of school age children.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Biglan AW . Glaucoma in children: are we making progress? JAAPOS 2006; 10: 7–21.
Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ . Comparison of three methods of intraocular pressure measurement and their relation to central corneal thickness. Eye 2010; 24: 1165–1170.
Bhan A, Brown AC, Shah S, Hamilton R, Dave D, Dua HS . Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applantion tonometer, and Tono-Pen. Invest Ophthalmol Vis Sci 2002; 43: 1389–1392.
Gunvant P, Newcomb RD, Kirstein EM, Malinovsky VE, Madonna RJ, Meetz RE . Measuring accurate IOPs: does correction factor help or hurt? Clin Ophthalmol 2010; 4: 611–616.
Kontiola AL . A new induction-based impact method for measuring intraocular pressure. Acta Ophthalmol Scand 2000; 78: 142–145.
Fernandes P, Díaz-Rey JA, Queirós A, Gonzalez-Meijome JM, Jorge J . Comparison of the ICare® rebound tonometer with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt 2005; 25: 436–440.
Lundvall A, Svedberg H, Chen E . Application of the ICare rebound tonometer in healthy infants. J Glaucoma 2011; 20: 7–9.
Chan WH, Lloyd IC, Ashworth JL, May K, Bhojwani D, Biswas S . Measurement of intraocular pressure in children in the UK. Eye 2011; 25: 119–120.
Kageyama M, Hirooka K, Baba T, Shiraga F . Comparison of ICare rebound tonometer with noncontact tonometer in healthy children. J Glaucoma 2011; 20: 63–66.
Pakrou N, Gray T, Mills R, Landers J, Craig J . Clinical comparison of the Icare tonometer and Goldmann applanation tonometry. J Glaucoma 2008; 17: 43–47.
Jorge J, Fernandes P, Queirós A, Ribeiro P, Garcês C, Gonzalez-Meijome JM . Comparison of the IOPen and iCare rebound tonometers with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt 2010; 30: 108–112.
Asrani S, Chatterjee A, Wallace DK, Santiago-Turla C, Stinnett S . Evaluation of the ICare rebound tonometer as a home intraocular pressure monitoring device. J Glaucoma 2011; 20 (2): 74–79.
Abraham LM, Epasinghe NCR, Selva D, Casson R . Comparison of the ICare® rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye 2008; 22: 503–506.
Sahin A, Basmak H, Niyaz L, Yildirim N . Reproducibility and tolerability of the ICare rebound tonometer in school children. J Glaucoma 2007; 16: 185–188.
Nakamura M, Darhad U, Tatsumi Y, Fujioka M, Kusuhara A, Maeda H et al. Agreement of rebound tonometer in measuring intraocular pressure with three types of applanation tonometers. Am J Ophthalmol 2006; 142: 332–334.
Richter S, Horn D, Bergknoff H . A survey of intraocular pressures with emphasis on patients under ten years of age. Am J Optom Physiol Opt 1979; 56: 193–196.
Duckman RH, Fitzgerald DE . Evaluation of intraocular pressure in a paediatric population. Optom Vis Sci 1992; 69: 705–709.
Pensiero S, Da Pozzo S, Perissutti P, Cavallini GM, Guerra R . Normal intraocular pressure in children. J Ped Ophthalmol Strabismus 1992; 29: 79–84.
Bauman HE . Use of the polatest in practice. Ophthalmologica 1969; 158: 612–621.
Brautaset RL, Jennings JA . Associated phoria and the measuring and correcting methodology after H-J. Haase (MKH). Strabismus 2001; 9: 165–176.
Goss DA . Clinical accommodation testing. Curr Opin Ophthalmol 1992; 31: 78–82.
Rutstein RP, Fuhr PD, Swiatocha J . Comparing the amplitude of accommodation determined objectively and subjectively. Optom Vis Sci 1993; 70: 496–500.
Chen AH, O'Leary DJ, Howell ER . Near visual function in young children. Part I: near point of convergence. Part II: amplitude of accommodation. Part III: near heterophoria. Ophthalmic Physiol Opt 2000; 20: 185–198.
Zellers JA, Alpert TL, Rouse MW . A review of the literature and a normative study of accommodative facility. J Am Optom Assoc 1984; 55: 31–37.
Locke LC, Somers W . A comparison study of dynamic retinoscopy techniques. Optom Vis Sci 1989; 66: 540–544.
Youn DH, Yu YS, Park IW . Intraocular pressure and axial length in children. Korean J Ophthalmol 1990; 4: 26–29.
Sihota R, Tuli D, Dada T, Gupta V, Sachdeva MM . Distribution and determinants of intraocular pressure in a normal pediatric population. J Pediatr Ophthalmol Strabismus 2006; 43: 14–18.
Jaafar MS, Kazi GA . Normal intraocular pressure in children: a comparative study of the Perkins applanation tonometer and the pneumatonometer. J Pediatr Ophthalmol Strabismus 1993; 30: 284–287.
Schacknow PN, Samples JN . The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care. 1st edn. Springer-Verlag Press: New York, 2010.
Pediatric Eye Disease Investigator Group Bradfield YS, Melia BM, Repka MX, Kaminski BM, Davitt BV, Johnson DA et al. Central corneal thickness in children. Arch Ophthalmol 2011; 129: 1132–1138.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dusek, W., Pierscionek, B. & McClelland, J. Age variations in intraocular pressure in a cohort of healthy Austrian school children. Eye 26, 841–845 (2012). https://doi.org/10.1038/eye.2012.54
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2012.54
Keywords
This article is cited by
-
Distribution and analysis of intraocular pressure and its possible association with glaucoma in children
International Ophthalmology (2021)