Abstract
Background
Globe-sparing treatments such as plaque brachytherapy, local or endoresection, and proton beam therapy (PBT) are the treatments of choice for posterior uveal melanoma. However, both early and late complications can arise from these techniques, including vitreous haemorrhage (VH) and retinal detachment (RD). Choroidal melanomas in Scotland are managed by a single unit, the Scottish Ocular Oncology Service (SOOS).
Methods
Indications and outcomes from surgery were analysed for patients undergoing vitrectomy following treatment for uveal melanoma in the SOOS between 1998 and 2013.
Results
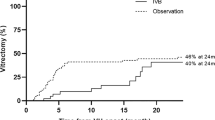
Seventeen from 715 cases (2.4%) required vitrectomy, of which 8/445 (1.8%) followed plaque brachytherapy, 7/43 (16.3%) combined local resection and brachytherapy, and 2/227 (0.9%) PBT. Casenotes were reviewed for 16/17 cases, with surgery indicated for VH in 10 (63%), RD in 5 (31%), and combined VH/RD in 1 (6%). The median interval from initial tumour treatment to vitrectomy was 5.8 months (range 10 days to 8.8 years). Ten (63%) required early vitrectomy (within 6 months), of which the majority (70%) followed combined resection/brachytherapy. Six (37%) required late vitrectomy (after 6 months), of which all were non-clearing VH following plaque brachytherapy, with proliferative retinopathy in 4/6 (67%), and tumour recurrence in 2/6 (33%). Overall vision improved in 8 eyes (50%), remained the same in 2 (12.5%), and deteriorated in 6 (37.5%).
Conclusions
Early vitrectomy was most commonly indicated for RD following local resection, and late vitrectomy for VH due to radiation retinopathy. The majority of patients undergoing vitrectomy gained or maintained vision.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Colloborative Ocular Melanoma Study (COMS) Group. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report No. 28. Arch Ophthalmol 2006; 124 (12): 1684–1693.
Houston SKS, Ardila ML, Markoe A, Murray TG . When to consider vitrectomy in eyes with posterior uveal melanoma. Retinal Physician 2012; 9: 24–28.
http://www.scotlandscensus.gov.uk/en/censusresults/rel1asb.html#5. Accessed 15 December 2013.
http://www.graphpad.com/quickcalcs/contingency1.cfm. Accessed 18 February 2014.
Damato B, Groenewald CP, McGalliard JN, Wong D . Rhegmatogenous retinal detachment after transscleral local resection of choroidal melanoma. Ophthalmology 2002; 109: 2137–2143.
Beykin G, Pe’er J, Hemo Y, Frenkel S, Chowers I . Pars plana vitrectomy to repair retinal detachment following brachytherapy for uveal melanoma. Br J Ophthalmol 2013; 97: 1534–1537.
Tran BK, Schalenbourg A, Bovey E, Zografos L, Wolfensberger TJ . Role of vitreoretinal surgery in maximizing treatment outcome following complications after proton therapy for uveal melanoma. Retina 2013; 33: 1777–1783.
Bansal AS, Bianciotto CG, Maguire JI, Regillo CD, Shields JA, Shields CL . Safety of pars plana vitrectomy in eyes with plaque-irradiated posterior uveal melanoma. Arch Ophthalmol 2012; 130 (10): 1285–1290.
Bianciotto C, Shields CL, Pirondini C, Mashayekhi A, Furuta M, Shields JA . Vitreous haemorrhage after plaque radiotherapy for uveal melanoma. Retina 2012; 32: 1156–1164.
Foster WJ, Harbour JW, Holekamp NM, Shah GK, Thomas MA . Pars plana vitrectomy in eyes containing a treated posterior uveal melanoma. Am J Ophthalmol 2003; 136: 471–476.
Lonngi M, Houston SK, Murray TG, Sisk RA, Decatur CL, Cavalcante M et al. Microincisional vitrectomy for retinal detachment in I-125 brachytherapy-treated patients with posterior uveal malignant melanoma. Clin Ophthalmol 2013; 7: 427–435.
Wilson MW, Hungerford JL . Comparison of episcleral plaque and proton beam radiation therapy for the treatment of choroidal melanoma. Ophthalmology 1999; 106: 1579–1587.
Papageorgiou LI, Cohen VML, Bunce C, Kinsella M, Hungerford JL . Predicting local control of choroidal melanomas following 106Ru plaque brachytherapy. Br J Ophthalmol 2011; 95: 166–170.
Lommatzsch PK, Werschnik C, Schuster E . Long-term follow-up of Ru-106/Rh-106 brachytherapy for posterior uveal melanoma. Graefes Arch Clin Exp Ophthalmol 2000; 238: 129–137.
Hungerford JL . Current trends in the treatment of ocular melanoma by radiotherapy. Clin Experiment Ophthalmol 2003; 31 (1): 8–13.
Shields JA, Shields CL, Donoso LA . Management of posterior uveal melanoma. Surv Ophthalmol 1991; 36: 161–195.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chia, S., Smith, H., Hammer, H. et al. Incidence and indications for pars plana vitrectomy following the treatment of posterior uveal melanomas in Scotland. Eye 29, 748–756 (2015). https://doi.org/10.1038/eye.2015.20
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2015.20