Abstract
Purpose
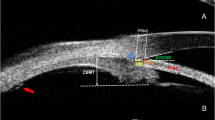
To characterise and differentiate posterior microphthalmos (PM) and nanophthalmos (NO) using morphometric parameters.
Patients and methods
Consecutive case database of patients with hyperopia >+7.00 D sphere was analysed retrospectively for clinical and biometric characterisation. Thirty-eight consecutive high-hyperopic subjects (75 eyes) with axial lengths <20.5 mm underwent uniform comprehensive ocular evaluation. Twenty-five subjects were diagnosed as PM and 13 as NO based on the horizontal corneal diameter. Parameters analysed included visual acuity, refraction, horizontal corneal diameter, anterior chamber depth, lens thickness, axial length, fundus changes, and associated ocular pathology. Primary outcome measures: ocular biometry difference between PM and NO. Secondary outcome measures: differences in associated ocular pathologies between PM and NO.
Results
Hyperopia ranged from +7 to +17 D and was similar in the two groups. Lens thickness was statistically more in NO than in PM group (4.53±0.75 mm vs 3.82±0.48 mm, P <0.001), whereas anterior chamber depth was more in the PM than in NO group (3.26±0.36 mm, vs 2.59±0.37 mm, P<0.001). NO had higher association with angle-closure glaucoma (66.7% vs 0%) and pigmentary retinopathy (38.5 vs 8.0%) but lesser association with macular folds (0% vs 24%) as compared with PM. NO was associated with poorer visual acuity.
Conclusion
PM and NO have significant differences in lens thickness, anterior chamber depth, prevalence of glaucoma, pigmentary retinopathy, macular pathology, and visual acuity while being similar in hyperopic refraction.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Elder MJ . Aetiology of severe visual impairment and blindness in microphthalmos. Br J Ophthalmol 1994; 78 (5): 332–334.
Singh OS, Sofinski SJ . Anomalies in the size of the eye. In: Duke-Elder S (ed). System Of Ophthalmology. CV Mosby: St Louis, USA, 1963, pp 488–495.
Weiss AH, Kousseff BG, Ross EA, Longbottom J . Simple microphthalmos. Arch Ophthalmol 1989; 107 (11): 1625–1630.
Vingolo EM, Steindl K, Forte R, Zompatori L, Iannaccone A, Sciarra A et al. Autosomal dominant simple microphthalmos. J Med Genet 1994; 31 (9): 721–725.
Weiss AH, Kousseff BG, Ross EA, Longbottom J . Complex microphthalmos. Arch Ophthalmol 1989; 107 (11): 1619–1624.
Ryan EA, Zwaan J, Chylack LT . Nanophthalmos with uveal effusion: clinical and embryologic considerations. Ophthalmology 1982; 89 (9): 1013–1017.
Crespí J, Buil JA, Bassaganyas F, Vela-Segarra JI, Díaz-Cascajosa J, Ayala-Ramírez R et al. A novel mutation confirms MFRP as the gene causing the syndrome of nanophthalmos-renititis pigmentosa-foveoschisis-optic disk drusen. Am J Ophthalmol 2008; 146 (2): 323–328.
Mandal AK, Das T, Gothwal VK . Angle closure glaucoma in nanophthalmos and pigmentary retinal dystrophy: a rare syndrome. Indian J Ophthalmol 2001; 49 (4): 271–272.
MacKay CJ, Shek MS, Carr RE, Yanuzzi LA, Gouras P . Retinal degeneration with nanophthalmos, cystic macular degeneration, and angle closure glaucoma. A new recessive syndrome. Arch Ophthalmol 1987; 105 (3): 366–371.
Serrano JC, Hodgkins PR, Taylor DS, Gole GA, Kriss A . The nanophthalmic macula. Br J Ophthalmol 1998; 82 (3): 276–279.
Buys YM, Pavlin CJ . Retinitis pigmentosa, nanophthalmos, and optic disc drusen: a case report. Ophthalmology 1999; 106 (3): 619–622.
Yue BY, Kurosawa A, Duvall J, Goldberg MF, Tso MO, Sugar J . Nanophthalmic sclera. Fibronectin studies. Ophthalmology 1988; 95 (1): 56–60.
Boynton JR, Purnell EW . Bilateral microphthalmos without microcornea associated with unusual papillomacular retinal folds and high hyperopia. Am J Ophthalmol 1975; 79 (5): 820–826.
Ryckewaert M, Zanlonghi X, Bertrand-Cuignet H, Constantinides G . High hyperopia with papillomacular fold. Ophthalmologica 1992; 204 (1): 49–53.
Spitznas M, Gerke E, Bateman JB . Hereditary posterior microphthalmos with papillomacular fold and high hyperopia. Arch Ophthalmol 1983; 101 (3): 413–417.
Lee S, Ai E, Lowe M, Wang T . Bilateral macular holes in sporadic posterior microphthalmos. Retina 1990; 10 (3): 185–188.
Nowilaty SR, Khan AO, Aldahmesh MA, Tabbara KF, Al-Amri A, Alkuraya FS . Biometric and molecular characterization of clinically diagnosed posterior microphthalmos. Am J Ophthalmol 2013; 155 (2): 361–372.e7.
Nguyen ATQ, Johnson MA, Hutcheson KA . Good visual function in posterior microphthalmos. J AAPOS 2000; 4 (4): 240–242.
Adler FH . Physiology of the eye: Clinical Application. 4th edn. Mosby-Year Book: St Louis, MO, USA, 1965.
Khairallah M, Messaoud R, Zaouali S, Ben Yahia S, Ladjimi A, Jenzri S . Posterior segment changes associated with posterior microphthalmos. Ophthalmology 2002; 109 (3): 569–574.
Proença H, Castanheira-Dinis A, Monteiro-Grillo M . Bilateral nanophthalmos and pigmentary retinal dystrophy—an unusual syndrome. Graefes Arch Clin Exp Ophthalmol 2006; 244 (9): 1203–1205.
Ayala-Ramirez R, Graue-Wiechers F, Robredo V, Amato-Almanza M, Horta-Diez I, Zenteno JC . A new autosomal recessive syndrome consisting of posterior microphthalmos, retinitis pigmentosa, foveoschisis, and optic disc drusen is caused by a MFRP gene mutation. Mol Vis 2006; 12: 1483–1489.
Pehere N, Jalali S, Deshmukh H, Kannabiran C . Posterior microphthalmos pigmentary retinopathy syndrome. Doc Ophthalmol 2011; 122 (2): 127–132.
Acknowledgements
No external funding support was obtained for the purpose of this study. The study was supported by Hyderabad eye research foundation. There are no financial disclosures to be made. Contribution of authors—design and conduct of the study (SJ); collection (SJ, UM, LB), management (SJ), analysis and interpretation of the data (SJ, NR, HLR); manuscript preparation (SJ, NR, UM, LB, NP), review (SJ, NR, HLR, NP), or approval of the manuscript (SJ, NR, HLR, NP,UM,LB). IRB approval was obtained before the analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Relhan, N., Jalali, S., Pehre, N. et al. High-hyperopia database, part I: clinical characterisation including morphometric (biometric) differentiation of posterior microphthalmos from nanophthalmos. Eye 30, 120–126 (2016). https://doi.org/10.1038/eye.2015.206
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2015.206
This article is cited by
-
A unique case of bilateral nanophthalmos and pigmentary retinal abnormality with unilateral angle closure glaucoma and optic disc pit
BMC Ophthalmology (2023)
-
Genetic analysis assists diagnosis of clinical systemic disease in children with excessive hyperopia
BMC Pediatrics (2022)
-
Comparisons of size of foveal avascular zone area among children with posterior microphthalmos, high hyperopia, and normal eyes
International Ophthalmology (2022)
-
Phacoemulsification with double-in-bag intraocular lens implantation in nanophthalmic eyes with angle-closure glaucoma
International Ophthalmology (2022)
-
Clinical spectrum and treatment outcomes of patients with nanophthalmos
Eye (2021)