Abstract
Purpose
To study the visual outcomes of congenital and developmental cataract surgery and determine variables for presentation for pediatric cataract surgery in KwaZulu Natal province of South Africa.
Methods
Care-givers of children presenting with cataract to a quaternary centre were asked when they first detected the condition. The reasons for delay between detection and surgery were studied. The children underwent a comprehensive eye examination and then appropriate surgery. They were prospectively followed up for 3 months and visual acuity and stereopsis were noted. Delay in presentation for surgery and visual outcomes were co-related with demographic and clinical factors.
Results
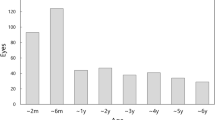
Eighty-three non-traumatic cataract surgeries in 50 children were studied. Twenty-six (52%) were males, mean age was 3 years 10 months (SD 3yrs 4 months). The mean delay between identification and surgery was 20.7 months (SD 18 months). Twenty-six (52%) children had >15 months interval between diagnosis and surgery. Only mother’s occupation was significantly associated with delay (P=0.017). Post-surgery 17/69 (24.7%) had visual acuity ≥6/18, 20/69 (29.0%) had vision between 6/24–6/60, whereas 32/69 (46.3%) had visual acuity ≤6/60. The final vision was associated with age (P=0.031), delay between diagnosis and surgery (P<0.001), type of surgery (P=0.046) and preoperative vision (P<0.001).
Conclusion
Although the children’s vision improved substantially, a longer follow-up and amblyopia treatment would be necessary to optimize the visual outcome, which depended on age and preoperative vision. Health promotion activities aimed at mothers are important in improving visual outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gilbert C, Foster A . Childhood blindness in the context of VISION 2020—the right to sight. Bull World Health Organ 2001; 79 (3): 227–232.
Rahi JS, Gilbert CE, Foster A, Minassian DC . Measuring the burden of childhood blindness. Br J Ophthalmol 1999; 83: 387–388.
Gogate P, Muhit M . Childhood blindness and cataract in developing countries. Community Eye Health 2009; 22 (69): 4–5.
Gilbert CE, Rahi JS, Quinn GE . Visual impairment and blindness in children. In: Johnson GJ, Weale R, Minassian DC, West SK (eds). The Epidemiology of Eye Disease, 2nd edn. Arnold: London, UK, 2003.
Ram J, Brar GS, Kaushik S, Gupta A, Gupta A . Role of posterior capsulotomy with vitrectomy and intraocular lens design and material in reducing posterior capsule opacification after pediatric cataract surgery. J Cataract Refract Surg 2003; 29: 1579–1584.
Wilson ME, Trivedi RH, Bartholomew LR, Pershing S . Comparison of anterior vitrectorhexis and continuous curvilinear capsulorhexis in pediatric cataract and intraocular lens implantation surgery: a 10-year analysis. J AAPOS 2007; 11 (5): 443–447.
Ledoux DM, Trivedi RH, Wilson ME, Payne JF . Pediatric cataract extraction with IOL: visual acuity outcome when measured at age 4years and older. J AAPOS 2007; 11: 218–224.
Chak M, Wade A, Rahi JS . British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Invest Ophthalmol Vis Sci 2006; 47 (10): 4262–4269.
Gogate PM, Sahasrabudhe M, Shah M, Patil S, Kulkarni AN, Trivedi R et al. Long term outcomes of bilateral congenital and developmental cataracts operated in Maharashtra, India. Indian J Ophthalmol 2014; 62 (2): 186–195.
Thakur J, Reddy H, Wilson ME Jr, Paudyal G, Gurung R, Thapa S et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg 2004; 30: 1629–1635.
You C, Wu X, Zhang Y, Dai Y, Huang Y, Xie L . Visual impairment and delay in presentation for surgery in chinese pediatric patients with cataract. Ophthalmology 2011; 118 (1): 17–23.
Bhusal S, Ram J, Sukhija J, Pandey S, Kaushik SS . Comparison of the outcome of implantation of hydrophobic acrylic versus silicone intraocular lenses in pediatric cataract: prospective randomized study. Can J Ophthalmol 2010; 45 (5): 531–536.
Gogate P, Khandekar R, Srisimal M, Dole K, Taras S, Kulkarni S et al. Delayed presentation of cataracts in children: are they worth operating upon? Ophthalmic Epidemiol 2010; 17 (1): 25–33.
Yorston D, Wood M, Foster A . Results of cataract surgery in young children in east Africa. Br J Ophthalmol 2001; 85 (3): 267–271.
Bowman R, Karibu J, Negretti G, Wood M . Outcome of bilateral cataract surgery in Tanzanian children. Ophthalmology 2007; 114 (12): 2287–2292.
Msukwa G, Ninguna M, Tumweisgye C, Shilo B, Courtright P, Lewallen S . Cataracts in children attending schools for the blind and resource centers in Eastern Africa. Ophthalmology 2009; 116: 1009–1012.
Dahan E, Drusedau MU . Choice of lens and dioptric power in pediatric pseudophakia. J Cataract Refract Surg 1997; 23: 618–623.
Mwende J, Bronsard A, Mosha M, Bowman R, Geneau R, Courtright P . Delay in presentation to hospital for surgery for congenital and developmental cataract in Tanzania. Br J Ophthalmol 2005; 89: 1478–1482.
Park JH, Yu YS, Kim JH, Kim SJ, Choung HK . Visual function after primary posterior chamber intraocular lens implantation in pediatric unilateral cataract: stereopsis and visual acuity. Korean J Ophthalmol 2007; 21 (4): 195–200.
Congdon NG, Ruiz S, Suzuki M, Herrera V . Determinants of pediatric cataract program outcomes and follow up in a large series in Mexico. J Cataract Refract Surg 2007; 33: 1775–1780.
Schulze Schwering M, Finger RP, Barrows J, Nyrenda M, Kalua K . Barriers to uptake of free pediatric cataract surgery in Malawi. Ophthalmic Epidemiol 2014; 21 (3): 138–143.
Gogate P, Patil S, Kulkarni A, Mahadik A, Tamboli R, Mane R et al. Barriers to follow-up for pediatric cataract surgery in Maharashtra, India. How regular follow-up is important for good outcome. Indian J Ophthalmol 2014; 62 (3): 327–332.
Pon JA, Bevin TH, Herbison P, Taylor BJ, Sanderson G . A novel instrument for assessing the retinal red reflex for non-ophthalmic health professionals. Clin Exp Optom 2005; 88 (3): 160–164.
Msukwa G, Njuguna M, Tumwesigye C, Shilio B, Courtright P, Lewallen S . Cataract in children attending schools for the blind and resource centers in eastern Africa. Ophthalmology 2009; 116 (5): 1009–1012.
Kishiki E, Shirima S, Lewallen S, Courtright P . Improving postoperative follow-up of children receiving surgery for congenital or developmental cataracts in Africa. J AAPOS 2009; 13 (3): 280–282.
Acknowledgements
We thank Jill Sloan, Nafisa Baboo, Hendrik Grobbelaar, Musa Gumede and Mbali Mpungose from Orbis Africa for help in logistics and data collection. Shrivallabh Sane of Data Clinic, Pune and Bharti Vidyapeeth Medical College, Pune for statistical analysis. We also thank Jyoti Jaggernath, African Vision Research Institute for her inputs. The study was funded by the Pediatric Cataract Initiative, Bausch and Lomb and Lions International.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gogate, P., Parbhoo, D., Ramson, P. et al. Surgery for sight: outcomes of congenital and developmental cataracts operated in Durban, South Africa. Eye 30, 406–412 (2016). https://doi.org/10.1038/eye.2015.211
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2015.211
This article is cited by
-
Limitations in cataract surgical services for children in Ethiopia: a nationwide survey of pediatric cataract surgeons
BMC Ophthalmology (2021)
-
Visual Outcome and Related Factors in Bilateral Total Congenital Cataract Patients: A Prospective Cohort Study
Scientific Reports (2016)
-
Surgery for sight: outcomes of congenital and developmental cataracts operated in Durban, South Africa
Eye (2016)
-
Surgery for sight: outcomes of congenital and developmental cataracts operated in Durban, South Africa
Eye (2016)