Abstract
Purpose
Five-year prospective data on children enrolled in the Infant Aphakia Treatment Study (IATS) provided an opportunity to explore ocular and systemic associations in patients with a unilateral congenital cataract.
Methods
Infants <7 months of age with a unilateral cataract were eligible for IATS screening. We reviewed data pertaining to the exclusion of patients as well as data collected on standardized study forms used at any time for documentation of ocular or systemic disorders.
Results
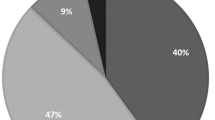
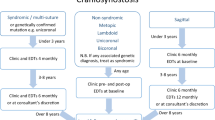
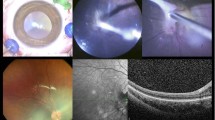
Overall, 227 infants were referred for possible enrollment. Of these, 10 had insignificant cataracts and 32 refused to participate. Of those excluded, 3 were premature, 27 had significant ocular disease (usually persistent fetal vasculature (PFV) or corneal diameter <9 mm), and 4 had systemic disorders. An additional 26 were excluded at the time of the first EUA, most often because of PFV or variants thereof. On follow-up, in the 114 enrolled patients, the following disorders were diagnosed: Stickler syndrome (1), mitochondrial disease (1), autism (1), and presumed congenital rubella syndrome (1). No patient developed a cataract in the fellow eye.
Discussion
Some conditions that can feature unilateral cataracts are diagnosed at birth or very early in life, but others may be diagnosed at varying periods thereafter. PFV and its variants are the most common associated ocular findings in about a quarter of cases of unilateral congenital cataracts.
Conclusion
Although patients with a unilateral cataract may have significant associated abnormalities in the affected eye, most commonly PFV and its variants, the prevalence of associated significant systemic disease is quite low.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Cassidy L, Taylor D . Congenital cataract and multisystem disorders. Eye (Lond) 1999; 13 (Pt 3b): 464–473.
Gillespie RL, O'Sullivan J, Ashworth J, Bhaskar S, Williams S, Biswas S et al. Personalized diagnosis and management of congenital cataract by next-generation sequencing. Ophthalmology 2014; 121: 2124–2137.
Infant Aphakia Treatment Study G Infant Aphakia Treatment Study G Lambert SR Infant Aphakia Treatment Study G Buckley EG Infant Aphakia Treatment Study G Drews-Botsch C Infant Aphakia Treatment Study G DuBois L Infant Aphakia Treatment Study G Hartmann E et al. The infant aphakia treatment study: design and clinical measures at enrollment. Arch Ophthalmol 2010; 128: 21–27.
Infant Aphakia Treatment Study G Infant Aphakia Treatment Study G Lambert SR Infant Aphakia Treatment Study G Buckley EG Infant Aphakia Treatment Study G Drews-Botsch C Infant Aphakia Treatment Study G DuBois L Infant Aphakia Treatment Study G Hartmann EE et al. A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: grating acuity and adverse events at age 1 year. Arch Ophthalmol 2010; 128: 810–818.
Edwards AO . Clinical features of the congenital vitreoretinopathies. Eye (Lond) 2008; 22: 1233–1242.
Yusuf IH, Sandford V, Hildebrand GD . Congenital cataract in a child with pyridoxine-dependent epilepsy. J AAPOS 2013; 17: 315–317.
Baldwin A, Risma J, Longmuir S . Transient leopard spot corneal endothelial staining with trypan blue during cataract surgery in a child with congenital rubella syndrome. J AAPOS 2013; 17: 629–631.
Acknowledgements
The study was funded by research grants EY13272 and EY13287 from the National Eye Institute. It was also supported in part by a NIH Departmental Core Grant EY006360 and Research to Prevent Blindness Inc., New York, NY, USA.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Writing Committee: The following members of the IATS take authorship responsibility: lead author: Scott R. Lambert, MD; Additional writing committee members: Michael J Lynn, MS, E Eugenie Hartmann, PhD, Lindreth DuBois, MEd MMSc, Carolyn Drews-Botsch, PhD, Sharon F Freedman, MD, David A Plager, MD, Edward G Buckley, MD, M Edward Wilson, MD. Administrative Units and Participating Clinical Centers Clinical Coordinating Center (Emory University): Scott R Lambert, MD (Study Chair); Lindreth Dubois, MEd, MMSc (National Coordinator) Data Coordinating Center (Emory University): Michael Lynn MS (Director), Betsy Bridgman, BS; Marianne Celano PhD; Julia Cleveland, MSPH; George Cotsonis, MS; Carey Drews-Botsch, PhD; Nana Freret, MSN; Lu Lu, MS; Seegar Swanson; Thandeka Tutu-Gxashe, MPH Vision and Developmental Testing Center (University of Alabama, Birmingham): E Eugenie Hartmann, PhD (Director); Anna K Carrigan, MPH; Clara Edwards; Eye Movement Reading Center (University of Alabama, Birmingham and Retina Foundation of the Southwest, Dallas, TX): Claudio Busettini, PhD, Samuel Hayley, Joost Felius, PhD Steering Committee: Scott R Lambert, MD; Edward G Buckley, MD; David A Plager, MD; M Edward Wilson, MD; Michael Lynn, MS; Lindreth Dubois, Med MMSc; Carolyn Drews-Botsch, PhD; E Eugenie Hartmann, PhD; Donald F Everett, MA Contact Lens Committee: Buddy Russell, COMT; Michael Ward, MMSc Participating Clinical Centers (In order by the number of patients enrolled) Medical University of South Carolina; Charleston, South Carolina (14): M Edward Wilson, MD; Margaret Bozic, CCRC, COA Harvard University; Boston, Massachusetts (14): Deborah K Vanderveen, MD; Theresa A Mansfield, RN; Kathryn Bisceglia Miller, OD University of Minnesota; Minneapolis, Minnesota (13): Stephen P Christiansen, MD; Erick D Bothun, MD; Ann Holleschau, BA; Jason Jedlicka, OD; Patricia Winters, OD; Jacob Lang, OD Cleveland Clinic; Cleveland, Ohio (10): Elias I Traboulsi, MD; Susan Crowe, BS, COT; Heather Haseley Cimino, OD Baylor College of Medicine; Houston, Texas (10): Kimberly G Yen, MD; Maria Castanes, MPH; Alma Sanchez, COA; Shirley York Oregon Health and Science University; Portland, Oregon (9): David T Wheeler, MD; Ann U Stout, MD; Paula Rauch, OT, CRC; Kimberly Beaudet, CO, COMT; Pam Berg, CO, COMT Emory University; Atlanta, Georgia (9): Scott R Lambert, MD; Amy K Hutchinson, MD; Lindreth Dubois, Med, MMSc; Rachel Robb, MMSc; Marla J Shainberg, CO Duke University; Durham, North Carolina (8): Edward G Buckley, MD; Sharon F Freedman, MD; Lois Duncan, BS; BW Phillips, FCLSA; John T Petrowski, OD Vanderbilt University: Nashville, Tennessee (8): David Morrison, MD; Sandy Owings COA, CCRP; Ron Biernacki CO, COMT; Christine Franklin, COT Indiana University, Indianapolis, Indiana (7): David A Plager, MD; Daniel E Neely, MD; Michele Whitaker, COT; Donna Bates, COA; Dana Donaldson, OD Miami Children’s Hospital, Miami, Florida (6): Stacey Kruger, MD; Charlotte Tibi, CO; Susan Vega University of Texas Southwestern; Dallas, Texas (6): David R Weakley, MD; David R Stager Jr MD; Joost Felius, PhD; Clare Dias, CO; Debra L Sager; Todd Brantley, OD Case Western Reserve, Cleveland, Ohio (1): Faruk Orge, MD. Data and Safety Monitoring Committee: Robert Hardy, PhD (Chair); Eileen Birch, PhD; Ken Cheng, MD; Richard Hertle, MD; Craig Kollman, PhD; Marshalyn Yeargin-Allsopp, MD (resigned); Cyd McDowell; Donald F Everett, MA (ex officio) Medical Safety Monitor: Allen Beck, MD
Rights and permissions
About this article
Cite this article
Traboulsi, E., Vanderveen, D., Morrison, D. et al. Associated systemic and ocular disorders in patients with congenital unilateral cataracts: the Infant Aphakia Treatment Study experience. Eye 30, 1170–1174 (2016). https://doi.org/10.1038/eye.2016.124
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2016.124
This article is cited by
-
Systemic and ocular associations in pediatric patients undergoing cataract surgery
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Variants in PAX6, PITX3 and HSF4 causing autosomal dominant congenital cataracts
Eye (2022)