Abstract
Purpose
To assess the diagnostic accuracy of the Edinburgh diplopia diagnostic algorithm.
Methods
This was a prospective study. Details of consecutive patients referred to ophthalmology clinics at Falkirk Community Hospital and Princess Alexandra Eye Pavilion, Edinburgh, with double vision were collected by the clinician first seeing the patient and passed to the investigators. The investigators then assessed the patient using the algorithm. An assessment of the degree of concordance between the ‘algorithm assisted’ diagnosis and the ‘gold standard’ diagnosis, made by a consultant ophthalmologist was then carried out. The accuracy of the pre-algorithm diagnosis made by the referrer was also noted.
Results
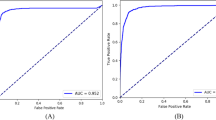
All patients referred with diplopia were eligible for inclusion. Fifty-one patients were assessed; six were excluded. The pre-algorithm accuracy of referrers was 24% (10/41). The algorithm assisted diagnosis was correct 82% (37/45) of the time. It correctly diagnosed: cranial nerve (CN) III palsy in 6/6, CN IV palsy in 7/8, CN VI palsy in 12/12, internuclear ophthalmoplegia in 4/4, restrictive myopathy in 4/4, media opacity in 1/1, and blurred vision in 3/3. The algorithm assisted diagnosis was wrong in 18% (8/45) of the patients.
Conclusions
The baseline diagnostic accuracy of non-ophthalmologists rose from 24 to 82% when patients were assessed using the algorithm. The improvement in the diagnostic accuracy resulting from the use of the algorithm would, hopefully, result in more accurate triage of patients with diplopia that are referred to the hospital eye service. We hope we have demonstrated its potential as a learning tool for inexperienced clinicians.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Timlin H, Butler L, Wright M . The accuracy of the Edinburgh Red Eye Diagnostic Algorithm. Eye (Lond) 2015; 29: 619–624.
Goudie C, Khan A, Lowe C, Wright M . The Accuracy of the Edinburgh Visual Loss Diagnostic Algorithm. Eye (Lond) 2015; 29: 1483–1488.
Komaroff AL . Algorithms and the ‘Art’ of Medicine. Am J Public Health 1982; 72 (1): 10–12.
Welch S, Eckstein M . Ophthalmology teaching in medical schools: a survey in the UK. Br J Ophthalmol 2011; 95: 748–749.
Borooah S, Wright M, Dhillon B . Ophthalmology Pocket Tutor. JP Medical Ltd: London, 2012.
Shaw J . When Muscles Falter: Update on Myasthenia Gravis [Internet]. American Academy of Ophthalmology; July 2006 [cited April 2015]. Available from http://www.aao.org/eyenet/article/when-muscles-falter-update-on-myasthenia-gravis.
Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D et al. Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation. Health Technol Assess 2006; 10: iii–iv xi–259.
Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S et al. Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis. Health Technol Assess 2006; 10: 1–168 iii–iv.
Ranjan D, Loewenstein D, Greig M, Acevedo A, Potter E, Appel J et al. Reliability and validity of an algorithm for the diagnosis of normal cognition, mild cognitive impairment, and dementia: implications for multicentre research studies. Am J Geriatr Psychiatry 2010; 18 (4): 363–370.
Christensen-Szalanski JJ, Diehr PH, Wood RW, Tompkins RK . Phased trial of a proven algorithm at a new primary care clinic. Am J Public Health 1982; 72 (1): 16–21.
Tamhankar MA, Kim JH, Ying G-S, Volpe NJ . Adult hypertropia: a guide to diagnostic evaluation based on review of 300 patients. Eye 2011; 25: 91–96.
Sowka JW, Kabat AG . Double trouble: how to diagnose diplopia. Rev Optom 2000; 137 (7): 53–58.
Trobe JD . The Rule of the Pupil Revisited: For Pupil-Involved Third Nerve Palsy and Aneurysm is the “Gold Standard” really a Catheter Angiogram in 2009? North American Neuro-Ophthalmology Society Annual Meeting Syllabus. University of Michigan: Ann Arbor, MI, USA, 2009, pp 107–110.
Marais W, Barret S . An overview of the third, fourth and sixth cranial nerve palsies. CME 2013; 31 (4): 147–152.
Tilikete C, Vighetto A . When is diplopia strongly suggestive of a vascular event? Expert Rev Ophthalmol 2009; 4 (4): 357–461.
Richard BW, Jones BR, Younge BR . Causes and Prognosis in 4278 cases of paralysis of the oculomotor, trochlear and abducens cranial nerves. Am J Ophthalmol 1992; 113: 489–496.
Morris RJ . Double vision as a presenting symptom on an ophthalmic casualty department. Eye 1991; 5: 124–129.
O’Colmain U, Gilmour C, MacEwan CJ . Acute-onset diplopia. Acta Ophthalmol 2014; 92: 382–386.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MW has received minimal royalties from the sales of ‘Ophthalmology Pocket Tutor’ where the algorithm has been published. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Butler, L., Yap, T. & Wright, M. The accuracy of the Edinburgh diplopia diagnostic algorithm. Eye 30, 812–816 (2016). https://doi.org/10.1038/eye.2016.44
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2016.44
This article is cited by
-
Peek Community Eye Health - mHealth system to increase access and efficiency of eye health services in Trans Nzoia County, Kenya: study protocol for a cluster randomised controlled trial
Trials (2019)
-
The Edinburgh diagnostic algorithms: a freely available validated resource for non-ophthalmologists
Eye (2016)