Abstract
Purpose
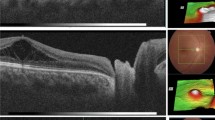
To evaluate surgical intervention with pars plana vitrectomy (PPV) for correction of optic disc pit maculopathy (ODP-M).
Patients and methods
Retrospective chart review from 13 centres of 51 eyes of 50 patients with ODP-M who underwent PPV between 2002–2014. Anatomic and final best-corrected visual acuity (BCVA) outcomes were evaluated for all cases with different adjuvant techniques.
Results
There were 23 males and 27 females with median age 25.5 (6–68) years. Preoperative median foveal thickness was 694.5 (331–1384) μm and improved to 252.5 (153–1405) μm. Median BCVA improved from 20/200 (20/20000 to 20/40) to 20/40 (20/2000 to 20/20) with 20/40 or better in 31 eyes. Complete retinal reattachment was achieved in 44 eyes (86.3%) at 7.1 (5.9) months. The good surgical outcomes were achieved in different adjuvant groups. Median follow-up was 24 (6 to 120) months.
Conclusions
These results confirm the long-term effectiveness of PPV for ODP-M. Prospective studies are needed to determine the effectiveness of any adjuvant technique in improving the success of PPV for ODP-M.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Apple DJ, Rabb MF, Walsh PM . Congenital anomalies of the optic disc. Surv Ophthalmol 1998; 27: 3–41.
Postel EA, Pulido JS, McNamara JA, Johnson MW . The etiology and treatment of macular detachment associated with optic nerve pits and related anomalies. Trans Am Ophthalmolol Soc 1998; 96: 73–93.
Gass JDM . Serous detachment of the macula secondary to congenital pit of the optic nerve head. Am J Ophthalmol 1969; 67: 821–841.
Jain N, Johnson MW . Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol 2014; 158: 423–435.
Gowdar JP, Rajesh B, Giridhar A, Gopalakrishnan M, Hussain R, Thachil T . An insight into the pathogenesis of optic disc pit-associated maculopathy with enhanced depth imaging. JAMA Ophthalmol 2015; 133: 466–469.
Georgalas I, Ladas I, Georgopoulos G, Petrou P . Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol 2011; 249: 1113–1122.
Garcia-Arumi J, Guraya BC, Espax AB, Castillo VM, Ramsay LS, Motta RM . Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefe’s Arch Clin Exp Ophthalmol 2004; 242: 819–826.
Cox MS, Witherspoon CD, Morris RE, Flynn HW . Evolving techniques in the treatment of macular detachment caused by optic nerve pits. Ophthalmology 1988; 95: 889–896.
Moisseiev E, Moisseiev J, Loewenstein A . Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. Int J Retin Vitr 2015; 1: 1–9.
Avci R, Yilmaz S, Inan UU, Kaderli B, Kurt M, Yalcinbayir O et al. Long-term outcomes of pars plana vitrectomy without internal limiting membrane peeling for optic disc pit maculopathy. Eye 2013; 27: 1359–1367.
Abouammoh MA, Alsulaiman SM, Gupta VS, Mousa A, Hirakata A, Berrocal MH et alKing Khaled Eye Specialist Hospital International Collaborative Retina Study Group. Pars plana vitrectomy with juxtapapillary laser photocoagulation versus vitrectomy without juxtapapillary laser photocoagulation for the treatment of optic disc pit maculopathy: the results of the KKESH International Collaborative Retina Study Group. Br J Ophthalmol 2016; 100: 478–483.
Hirakata A, Inoue M, Hiraoka T, McCuen BW 2nd . Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology 2012; 119: 810–818.
Steel DH, Williamson TH, Laidlaw DA, Sharma P, Matthews C, Rees J et al. Extent and location of intraretinal and subretinal fluid as prognostic factors for the outcome of patients with optic disk pit maculopathy. Retina 2016; 36: 110–118.
Rayat JS, Rudnisky CJ, Waite C, Huang P, Sheidow TG, Kherani A et al. Long-Term outcomes for optic disk pit maculopathy after vitrectomy. Retina 2015; 35: 2011–2017.
Hirakata A, Okada AA, Hida T . Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology 2005; 112: 1430–1435.
Shukla D, Kalliath J, Tandon M, Vijayakumar B . Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina 2012; 32: 1337–1342.
Gandorfer A, Kampik A . Role of vitreoretinal interface in the pathogenesis and therapy of macular disease associated with optic pits. Ophthalmologe 2000; 974: 276–279.
Rizzo S, Belting C, Genovesi-Ebert F, Di Bartolo E, Cresti F, Cinelli L et al. Optic disc pit maculopathy: the value of small-gauge vitrectomy, peeling, laser treatment, and gas tamponade. Eur J Ophthalmol 2012; 22: 620–625.
Lincoff H, Yannuzzi L, Singerman L, Kreissig I, Fisher Y . Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol 1993; 111: 1071–1079.
Johnson TM, Johnson MW . Pathogenic implications of subretinal gas migration through pits and atypical colobomas of the optic nerve. Arch Ophthalmol 2004; 122: 1793–1800.
Teke MY, Citirik M . 23 Gauge vitrectomy, endolaser, and gas tamponade versus vitrectomy alone for serous macular detachment associated with optic disc pit. Am J Ophthalmol 2015; 160: 779–785.
Gregory-Roberts EM, Mateo C, Corcóstegui B, Schiff WM, Chang LK, Quiroz-Mercado H et al. Optic disk pit morphology and retinal detachment: optical coherence tomography with intraoperative correlation. Retina 2013; 33: 363–370.
Matsumoto H, Yamanaka I, Hisatomi T, Enaida H, Ueno A, Hata Y et al. Triamcinolone acetonide-assisted pars plana vitrectomy improves residual posterior vitreous hyaloid removal: ultrastructural analysis of the inner limiting membrane. Retina 2007; 27: 174–179.
Coca MN, Tofigh S, Elkeeb A, Godley BF . Optic disc pit maculopathy recurring in the absence of vitreous gel. JAMA Ophthalmol 2014; 132: 1375–1376.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented in part as a free paper in EURETINA meeting in Hamburg, 2013, at Turkish-Israel Joint Meeting in EURETINA meeting in Hamburg, 2013 and presented in part as a scientific poster at the 31st Annual Meeting of American Society of Retinal Specialists, 24–28 August 2013, Toronto, ON, Canada.
Rights and permissions
About this article
Cite this article
Avci, R., Kapran, Z., Ozdek, Ş. et al. Multicenter study of pars plana vitrectomy for optic disc pit maculopathy: MACPIT study. Eye 31, 1266–1273 (2017). https://doi.org/10.1038/eye.2017.142
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.142
This article is cited by
-
Comparison of subretinal aflibercept vs ranibizumab vs bevacizumab in the context of PPV, pneumatic displacement with subretinal air and subretinal tPA in naïve submacular haemorrhage secondary to nAMD. “The Submarine Study”
Eye (2024)
-
The outcomes of intravitreal C3F8 gas tamponade combined with laser photocoagulation treatment for optic disc pit maculopathy
International Ophthalmology (2022)
-
Sulphur hexafluoride (SF6) intravitreal injection combined with argon laser photocoagulation for treatment of optic disc pit maculopathy
Eye (2021)
-
Surgical outcomes in patients with optic disc pit maculopathy: does peeling the ILM lead to better outcomes?
International Ophthalmology (2020)
-
Makulaveränderungen bei Grubenpapille – „Optic disc pit maculopathy“ (ODP-M)
Der Ophthalmologe (2019)