Abstract
Purpose
To evaluate a novel small-aperture supplementary implant that applies the principle of pinholes for management of irregular astigmatism, in postmortem human eyes.
Methods
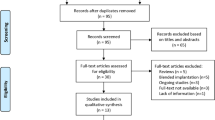
Pseudophakic human cadaver eyes were imaged by anterior segment optical coherence tomography (AS-OCT) to assess position of the in-the-bag intraocular lens (IOL). Eyes were prepared as per the Miyake-Apple technique. Two versions of the supplementary implant (open-loop and tripod designs) were then inserted into the sulcus of each eye. Evaluations under AS-OCT and from anterior and posterior views of the anterior segment were used to assess IOL fixation, centration, tilt, and interlenticular distance (ILD). This experimental study has been conducted in John A. Moran Eye Center, University of Utah.
Results
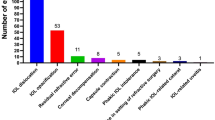
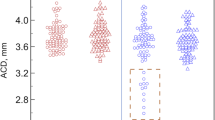
Nine eyes were selected, with various sizes, primary IOL materials/designs, and Soemmering’s ring formation. The open-loop model exhibited a mild degree of decentration and tilt in 2 eyes with zonular dehiscence. Mild decentration and tilt of the tripod were observed in 4 eyes; in 1 additional eye it was centered but mildly tilted. Three eyes with zonular dehiscence had one of the closed loops of the tripod located posteriorly to the ciliary processes. In all cases, an ILD was observed between the lenses (open loop: 0.65±0.13 mm; tripod: 0.41±0.12 mm).
Conclusions
It is important to take into account anatomical aspects related to ciliary sulcus fixation of supplementary IOLs. Both designs evaluated, exhibited appropriate centration and ILD. The open-loop design had less risk of tilt in association with haptics protruding posteriorly through areas of zonular weakness.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Fares U, Sarhan AR, Dua HS . Management of post-keratoplasty astigmatism. J Cataract Refract Surg 2012; 38 (11): 2029–2039.
Perlman EM . An analysis and interpretation of refractive errors after penetrating keratoplasty. Ophthalmology 1981; 88: 39–45.
Karabatsas CH, Cook SD, Sparrow JM . Proposed classification for topographic patterns seen after penetrating keratoplasty. Br J Ophthalmol 1999; 83 (4): 403–409.
Schraepen P, Vandorselaer T, Trau R, Tassignon MJ . LASIK and arcuate incisions for the treatment of post-penetrating keratoplasty anisometropia and/or astigmatism. Bull Soc Belge Ophtalmol 2004; 292: 19–25.
Buzard K, Febbraro JL, Fundingsland BR . Laser in situ keratomileusis for the correction of residual ametropia after penetrating keratoplasty. J Cataract Refract Surg 2004; 30 (5): 1006–1013.
Laíns I, Rosa AM, Guerra M, Tavares C, Lobo C, Silva MF, Quadrado MJ, Murta JN . Irregular astigmatism after corneal transplantation—efficacy and safety of topography-guided treatment. Cornea 2016; 35 (1): 30–36.
Kymionis GD, Yoo SH, Ide T, Culbertson WW . Femtosecond-assisted astigmatic keratotomy for post-keratoplasty irregular astigmatism. J Cataract Refract Surg 2009; 35 (1): 11–13.
Barnett M, Lien V, Li JY, Durbin-Johnson B, Mannis MJ . Use of Scleral Lenses and Miniscleral Lenses After Penetrating Keratoplasty. Eye Contact Lens 2016; 42 (3): 185–189.
Dexl AK, Jell G, Strohmaier C, Seyeddain O, Riha W, Rückl T, Bachernegg A, Grabner G . Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg 2015; 41 (3): 566–575.
Lindstrom RL, Macrae SM, Pepose JS, Hoopes PC Sr . Corneal inlays for presbyopia correction. Curr Opin Ophthalmol 2013; 24 (4): 281–287.
Trindade CLC, Trindade BLC . Novel pinhole intraocular implant for the treatment of irregular corneal astigmatism and severe light sensitivity after penetrating keratoplasty. J Cataract Refract Surg Online Case Reports 2015; 3: 4–7.
Kahraman G, Amon M . New supplementary intraocular lens for refractive enhancement in pseudophakic patients. J Cataract Refract Surg 2010; 36 (7): 1090–1094.
Falzon K, Stewart OG . Correction of undesirable pseudophakic refractive error with the Sulcoflex intraocular lens. J Refract Surg 2012; 28 (9): 614–619.
McIntyre JS, Werner L, Fuller SR, Kavoussi SC, Hill M, Mamalis N . Assessment of a single-piece hydrophilic acrylic IOL for piggyback sulcus fixation in pseudophakic cadaver eyes. J Cataract Refract Surg 2012; 38 (1): 155–162.
Reiter N, Werner L, Guan J, Li J, Tsaousis KT, Mamalis N, Srinivasan S . Assessment of a new hydrophilic acrylic supplementary IOL for sulcus fixation in pseudophakic cadaver eyes. Eye (Lond) 2017; 31 (5): 802–809.
Pereira FA, Werner L, Milverton EJ, Coroneo MT . Miyake-Apple posterior video analysis/photographic technique. J Cataract Refract Surg 2009; 35: 577–587.
Trindade CLC, Trindade FC, Trindade BC Tiny hero against the evil axis Video presented at the Annual Meeting of the American Society of Cataract and Refractive Surgery (ASCRS) 2017, CA, USA. Available at: http://ascrs2017.conferencefilms.com/abstractawards.wcs.
Kim WS, Park IK, Chun YS . Quantitative analysis of functional changes caused by pinhole glasses. Invest Ophthalmol Vis Sci 2014; 55 (10): 6679–6685.
Kanellopoulos AJ, Asimellis G, Georgiadou S . Digital pupillometry and centroid shift changes after cataract surgery. J Cataract Refract Surg 2015; 41 (2): 408–414.
Li L, Wang K, Yan Y, Song X, Liu Z . Research on calculation of the IOL tilt and decentration based on surface fitting. Comput Math Methods Med 2013; 2013: 572530.
Gomaa A, Lee RM, Liu CS . Polypseudophakia for cataract surgery: 10-year follow-up on safety and stability of two poly-methyl-methacrylate (PMMA) intraocular lenses within the capsular bag. Eye (Lond) 2011; 25 (8): 1090–1093.
Findl O, Menapace R, Rainer G, Georgopoulos M . Contact zone of piggyback acrylic intraocular lenses. J Cataract Refract Surg 1999; 25 (6): 860–862.
Findl O, Menapace R, Georgopoulos M, Kiss B, Petternel V, Rainer G . Morphological appearance and size of contact zones of piggyback intraocular lenses. J Cataract Refract Surg 2001; 27 (2): 219–223.
Hesse RJ . Refractive changes produced by capsule contraction after piggyback acrylic intraocular lens implantation. J Cataract Refract Surg 2002; 28 (12): 2229–2230.
Werner L, Apple DJ, Pandey SK, Solomon KD, Snyder ME, Brint SF, Gayton JL, Shugar JK, Trivedi RH, Izak AM . Analysis of elements of interlenticular opacification. Am J Ophthalmol 2002; 133 (3): 320–326.
Scharioth GB . New add-on intraocular lens for patients with age-related macular degeneration. J Cataract Refract Surg 2015; 41 (8): 1559–1563.
Acknowledgements
Michael Anderson, COA, Moran Eye Center assisted with the AS-OCT examination. Work supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology & Visual Sciences, University of Utah. Morcher GmbH provided the pinhole intraocular lenses used in this study. CLCT holds a patent of the implant and has a license contract with Morcher GmbH. The other authors have no financial or proprietary interest in any product mentioned in this paper. LW, MD, PhD, reports research grants from Abbott Medical Optics, grants and personal fees from Alcon, grants from Anew Optics, grants from Advanced Visual Sciences, grants from CIMA, grants from ClarVista, grants from DORC, grants from Hoya, grants from Medicontur, grants from Perfect Lens, grants from PhysIOL, grants and personal fees from PowerVision, grants from Sharklet, grants from Shifamed, grants from Sigilon, grants from Zeiss outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tsaousis, K., Werner, L., Trindade, C. et al. Assessment of a novel pinhole supplementary implant for sulcus fixation in pseudophakic cadaver eyes. Eye 32, 637–645 (2018). https://doi.org/10.1038/eye.2017.239
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.239