Abstract
Objective:
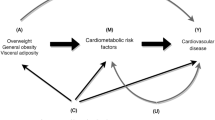
To investigate the effects of three weight loss interventions on cardiometabolic risk factors, including blood pressure, lipids, glucose and markers of insulin resistance and inflammation. We also examined whether categories of incremental weight change conferred greater improvements on these parameters.
Methods:
This 2-year trial was conducted in a primary care setting and included 390 obese participants who were randomly assigned to one of three interventions: (1) Usual Care (quarterly primary care provider (PCP) visits that included education about weight management); (2) Brief Lifestyle Counseling (quarterly PCP visits plus monthly behavioral counseling provided by a trained auxiliary health-care provider); or (3) Enhanced Brief Lifestyle Counseling (the same care as described for the previous intervention, plus weight loss medications or meal replacements). The primary outcome was change in cardiometabolic risk factors among groups.
Results:
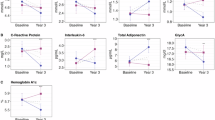
At month 24, participants in Enhanced Brief Lifestyle Counseling lost significantly more weight than those in Usual Care (4.6 vs 1.7 kg), with no other significant differences between groups. Enhanced Brief Lifestyle Counseling produced significantly greater improvements in high-density lipoprotein (HDL) cholesterol and triglyceride levels at one or more assessments, compared with the other two interventions. Markers of insulin resistance also improved significantly more in this group throughout the 2 years. Collapsing across the three groups, greater weight loss was associated with greater improvements in triglycerides, HDL cholesterol and markers of insulin resistance and inflammation at month 24, but was not significantly associated with reductions in blood pressure, total cholesterol and low-density lipoprotein cholesterol at any time.
Conclusions:
Enhanced Brief Lifestyle Counseling, which produced the largest weight loss, was generally associated with the greatest improvements in cardiovascular risk factors. These findings suggest that an intensive weight loss intervention, delivered in a primary care setting, can help obese individuals improve some cardiometabolic risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Goldstein DJ . Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord 1992; 16: 397–415.
Van Gaal LF, Mertens IL, Ballaux D . What is the relationship between risk factor reduction and degree of weight loss? Eur Heart J Suppl 2005; 7: L21–L26.
Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011; 34: 1481–1486.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Appel LJ, Champagne CM, Harsha HW, Cooper LS, Obarzanek E, Elmer PJ et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003; 289: 2083–2093.
Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008; 299: 1139–1148.
Tate DF, Jackvony EH, Wing RR . Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003; 289: 1833–1836.
Tsai AG, Wadden TA, Rogers MA, Day SC, Moore RH, Islam BJ . A primary care intervention for weight loss: results of a randomized controlled study. Obesity 2010; 18: 1614–1618.
Ockene IS, Hebert JR, Ockene JK, Saperia GM, Stanek E, Nicolosi R et al. Effect of a physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). Arch Intern Med 1999; 159: 725–731.
Martin PD, Dutton GR, Rhode PC, Horswell RL, Ryan DH, Brantley PJ . Weight loss maintenance following a primary care intervention for low-income minority women. Obesity 2008; 16: 2462–2467.
Ashley JM, St Jeor ST, Schrage JP, Perumean-Chaney SE, Gilbertson MC, McCall NL et al. Weight control in the physician’s office. Arch Intern Med 2001; 161: 1599–1604.
Yeh HC, Clark JM, Emmons KE, Moore RH, Bennett GG, Warner ET et al. Independent but coordinated trials: insights from the Practice-based Opportunities for Weight Reduction Trials Collaborative Research Group. Clin Trials 2010; 7: 322–332.
Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med 2011; 365: 1969–1979.
Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011; 365: 1959–1968.
Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med 2012; 172: 565–574.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002; 106: 3143–3421.
Borushek A . The CalorieKing Calorie, Fat and Carbohydrate Counter 8th edn. Family Health: Conta Mesa, CA, USA, 2008.
National Heart, Lung, and Blood Institute. Aim for a Healthy Weight. National Institutes of Health: Bethesda, MD, USA, 2005. NIH publication no. 05-5213.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med 2005; 353: 2111–2120.
Vetter ML, Wadden TA, Vinnard C, Moore RH, Khan Z, Volger S et al. Gender differences in relationship between symptoms of depression and high-sensitivity CRP. Int J Obes 2013; 37: S38–S43.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Acknowledgements
This research was supported by grants U01-HL087072 from the National Heart, Lung and Blood Institute and K24-DK065018 from the National Institutes of Diabetes and Digestive and Kidney Disease. We thank Amos Odeleye for his assistance with statistical analysis.
This article is published as part of a supplement, sponsored by the Center for Weight and Eating Disorders—University of Pennsylvania.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
TAW serves on the advisory boards of Novo Nordisk and Orexigen Therapeutics, which are developing weight loss medications, as well as of Alere and the Cardiometabolic Support Network, which provide behavioral weight loss programs. TAW has also served as a consultant for Boehringer Ingelheim, and has received grant support from the National Institutes of Health (NIH/NIDDK and NIH/NHLBI). DBS discloses relationships with the following companies: Allergan, BariMD, BaroNova, Enteromedics and Galderma. DBS has also received grant support from the National Institutes of Health (NIH). The remaining authors declare no conflict of interest.
Appendix
Appendix
POWER-UP Research Group: Investigators and Research Coordinators
Academic investigators at the Perelman School of Medicine at the University of Pennsylvania were Thomas A Wadden, PhD (principal investigator), David B Sarwer, PhD (co-principal investigator), Robert I Berkowitz, MD, Jesse Chittams, MS, Lisa Diewald, MS, RD, Shiriki Kumanyika, PhD, Renee Moore, PhD, Kathryn Schmitz, PhD, Adam G Tsai, MD, MSCE, Marion Vetter, MD, RD and Sheri Volger, MS, RD.
Research coordinators at the University of Pennsylvania were Caroline H Moran, BA, Jeffrey Derbas, BS, Megan Dougherty, BS, Zahra Khan, BA, Jeffrey Lavenberg, MA, Eva Panigrahi, MA, Joanna Evans, BA, Ilana Schriftman, BA, Dana Tioxon, Victoria Webb, BA and Catherine Williams-Smith, BS.
POWER-UP Research Group: Participating Sites and Clinical Investigators
PennCare–Bala Cynwyd Medical Associates: Ronald Barg, MD, Nelima Kute, MD, David Lush, MD, Celeste Mruk, MD, Charles Orellana, MD and Gail Rudnitsky, MD (primary care providers); Angela Monroe (lifestyle coach); Lisa Anderson (practice administrator).
PennCare—Internal Medicine Associates of Delaware County: David E Eberly, MD, Albert H Fink Jr, MD, Kathleen Malone, CRNP, Peter B Nonack, MD, Daniel Soffer, MD, John N Thurman, MD and Marc J Wertheimer, MD (primary care providers); Barbara Jean Shovlin, Lanisha Johnson (lifestyle coaches); Jill Esrey (practice administrator).
PennCare—Internal Medicine Mayfair: Jeffrey Heit, MD, Barbara C Joebstl, MD and Oana Vlad, MD (primary care providers); Rose Schneider, Tammi Brandley (lifestyle coaches); Linda Jelinski (practice administrator).
Penn Presbyterian Medical Associates: Joel Griska, MD, Karen J Nichols, MD, Edward G Reis, MD, James W Shepard, MD and Doris Davis-Whitely, PA (primary care providers); Dana Tioxon (lifestyle coach); Charin Sturgis (practice administrator).
PennCare—University City Family Medicine: Katherine Fleming, CRNP, Dana B Greenblatt, MD, Lisa Schaffer, DO, Tamara Welch, MD and Melissa Rosato, MD (primary care providers); Eugonda Butts, Marta Ortiz, Marysa Nieves and Alethea White (lifestyle coach); Cassandra Bullard (practice administrator).
PennCare–West Chester Family Practice: Jennifer DiMedio, CRNP, Melanie Ice, DO, Brandt Loev, DO, John S Potts, DO and Christine Tressel, DO (primary care providers); Iris Perez, Penny Rancy and Dianne Rittenhouse (lifestyle coaches); Joanne Colligan (practice administrator).
Rights and permissions
About this article
Cite this article
Vetter, M., Wadden, T., Chittams, J. et al. Effect of lifestyle intervention on cardiometabolic risk factors: results of the POWER-UP trial. Int J Obes 37 (Suppl 1), S19–S24 (2013). https://doi.org/10.1038/ijo.2013.92
Published:
Issue date:
DOI: https://doi.org/10.1038/ijo.2013.92
Keywords
This article is cited by
-
Maternal BMI changes from the prepregnancy to postpartum period are associated with postpartum cardiometabolic risk factors: a longitudinal study
Archives of Gynecology and Obstetrics (2023)
-
Long-term effects (> 24 months) of multiple lifestyle intervention on major cardiovascular risk factors among high-risk subjects: a meta-analysis
BMC Cardiovascular Disorders (2021)
-
Effectiveness of a community-based intervention for weight loss on cardiometabolic risk factors among overweight and obese women in a low socio-economic urban community: findings of the MyBFF@home
BMC Women's Health (2018)
-
Effects of Different Weight Loss Approaches on CVD Risk
Current Atherosclerosis Reports (2018)
-
Associations between weight change and biomarkers of cardiometabolic risk in South Asians: secondary analyses of the PODOSA trial
International Journal of Obesity (2016)