Abstract
Background/objectives:
To address behaviours associated with childhood obesity, certain target values are recommended that should be met to improve children’s health. In the IDEFICS (Identification and prevention of Dietary- and lifestyle-induced health Effects in Children and infantS) study such lifestyle recommendations were conveyed as six key messages. Here, we investigate the adherence of European children to these messages.
Methods:
The IDEFICS intervention was based on the intervention mapping approach with the following six targets: increase water consumption (to replace sugar-containing beverages), increase fruit/vegetable consumption, reduce daily screen time, increase daily physical activity, improve the quality of family life and ensure adequate sleep duration. Internationally recommended target values were applied to determine the prevalence of children meeting these targets.
Results:
In a cohort of 18 745 children participating in the IDEFICS baseline survey or newly recruited during follow-up, data on the above lifestyle behaviours were collected for a varying number of 8302 to 17 212 children. Information on all six behaviours was available for 5140 children. Although 52.5% of the cohort was classified in the highest category of water consumption, only 8.8% met the target of an intake of fruits/vegetables five times a day. The prevalence of children adhering to the recommendation regarding total screen time—below 1 h for pre-school children and 2 h for school children—was 51.1%. The recommended amount of at least 60 min of moderate-to-vigorous physical activity per day was fulfilled by 15.2%. Family life of the child measured by various indicators was considered as satisfactory in 22.8%. Nocturnal sleep duration of 11 (10) hours or more in pre-school (school) children was achieved by 37.9%. In general, children in northern countries and younger children showed better adherence to the recommendations. Only 1.1% of the children adhered to at least five of these recommendations.
Conclusions:
Current adherence of children to lifestyle recommendations to prevent childhood obesity is low where observed differences with respect to country, age and gender call for targeted intervention.
Similar content being viewed by others
Introduction
In the last decade, a rapid growth of the prevalence of obesity was experienced worldwide, the importance of which can be best illustrated with the forecast that this phenomenon could reverse the increase in life expectancy having been observed in the past decades.1 Similar trends of obesity epidemic were also observed in the child population, which made it a worldwide public health crisis.2 Later consequences of childhood obesity put a significant burden on, both, the individual’s health and quality of life as well as on the health care system on a societal level.
Recently, the so-called obesity epidemic in children showed a flattening trend in several countries,3 probably due to preventive and intervention efforts. Even if long-term observation will reinforce this favourable trend, obesity will still remain a major public health concern for the next decades4 to be managed by targeted interventions.5
The IDEFICS (Identification and prevention of Dietary- and lifestyle-induced health Effects in Children and infantS) study was designed to (1) investigate the aetiology of childhood obesity, by assessing the contributing role of potential risk factors, that is, the effects of diet, lifestyle, psychosocial and genetic factors,6 and to describe their causal pathways. (2) The IDEFICS study also launched an intervention programme which was developed according to the intervention mapping protocol,7 a methodological framework for the elaboration of public health promotion programmes and community interventions. Relevant behaviours and their determinants were dissected and integrated into matrices for operational interventional actions,8 chosen on the basis of existing evidence and/or supporting theoretical models for behaviour change. Lifestyle behaviours known as most relevant lifestyle-related risk factors for obesity9 were selected as intervention targets: (1) diet, (2) physical activity and (3) stress. Each of these three areas was addressed by two so-called key messages:
-
1a. Enhancing daily consumption of water
-
1b. Enhancing daily consumption of fruits and vegetables
-
2a. Reducing TV viewing
-
2b. Enhancing daily physical activity
-
3a. Improving the quality of family life
-
3b. Ensuring adequate sleep duration.
The aim of this paper is to describe the adherence to the recommendations related to these six key messages in the study sample, that is, at baseline before the intervention started and in newly recruited children at follow-up, stratified by country, sex and age. In addition, we calculated a composite compliance score of these targeted lifestyle factors.
Subjects and methods
Study subjects
A cohort of 16 228 children aged 2–9 years was examined in a population-based baseline survey in eight European countries ranging from North to South and from East to West (Estonia, Sweden, Germany, Belgium, Hungary, Italy, Spain, Cyprus) from autumn 2007 to spring 2008. The study was not designed to provide a representative sample for each country. Rather, this baseline survey (T0) was the starting point of a prospective study with the largest European children’s cohort established to date.10 This cohort and additional 2517 children aged 2–10.9 years who were newly recruited during a second survey (T1) 2 years later comprise the study sample of the present analysis. Exactly the same survey modules were deployed at baseline (T0) and at follow-up (T1). The actual age of school enrolment varied in the survey countries, so the school-aged subgroup was defined according to the most frequent date, that is, being 6 years or older.
All children in the defined age group who resided in the defined regions and who attended the selected primary schools (grades 1 and 2), pre-schools or kindergartens were eligible for participation. Children were enroled via schools and kindergartens to facilitate equal enrolment of all social groups. In addition to the signed informed consent given by parents, each child was asked to give verbal assent immediately before examination. All examination modules were offered to each participant, except accelerometry where the number of available devices limited the participation. Participants were free to opt out for specific modules, which resulted in varying numbers of response.
Assessment of lifestyle behaviours and related recommendations
In the following, we briefly describe how each of the lifestyle behaviours was measured in the IDEFICS study.
Questionnaires provided information for the indicator variables of five from the six key messages. Children’s Eating Habits Questionnaire11 (CEHQ) was completed by parents, recording dietary habits and food frequency referring to the previous four weeks. Indicators for diet-related key messages, that is, the frequency of water consumption and fruit and vegetable consumption were obtained from CEQH. Water consumption was assessed as times per day. The fruit and/or vegetable consumption was derived by summarising the daily consumption of the following food types: fruits with or without added sugar, including freshly pressed smoothies (while excluding juices), and cooked or raw vegetables.
CEHQ was complemented by a computer-based 24-h dietary recall, including an interview where, among other questions, parents reported what time their child went to bed the previous day and what time he/she got up in the morning, from which the nocturnal sleep duration was calculated for the previous day.
Parents completed a self-completion set of questionnaires to assess gestational, socio-demographic and behavioural factors, being the source also for proxy-reported daily screen time of the child separately for weekdays and weekend days with the help of the question: how long does your child usually watch TV/video/DVD per day?
The parental core questionnaire included questions from the KINDL questionnaire designed to assess health-related quality of life in children and adolescents independently of the current health status.12 As it was assumed that high quality of life indicates more balanced family life, a health-related quality of life score was used as an indicator of the key message referring to improved quality of family life, though the score itself covers a broader range of information than the family life. This health-related quality of life score comprised four of the six original KINDL dimensions:13 emotional self-being, self-esteem, family relations and social contacts. The range of the score was 12–48, the higher values indicating better quality of life.14
To monitor the physical activity, children wore a uniaxial accelerometer (ActiGraph or ActiTrainer, ActiGraph, Pensacola, FL, USA) on a hip belt over at least three consecutive days including one weekend day.15 A minimum duration of 6 h monitoring time per day was required to achieve proper reliability,16 whereas the epoch of sampling was set on 15 s, where non-wear time was defined as at least 20 min of consecutive zeroes. The duration of moderate-to-vigorous physical activity (MVPA) was determined according to the cut-offs of Evenson17 (see Konstabel et al.;18 this issue).
Composite compliance score
Internationally recommended target values regarding the six lifestyle behaviours are based on a report on existing guidelines.19
As water consumption is subject to relevant seasonal and climate influences and water content of the diet can also contribute to hydration; we have not considered the international recommendation20 for this key message but used the highest category of intake frequency in CEHQ, that is, four or more times per day as the target to be met.
Regarding daily consumption of fruits and vegetables, the national recommended target values proved to be so diverse that we decided to use the recommendation from the WHO CINDI nutritional guidelines,21 that is, a daily intake of five or more portions of fruits and/or vegetables.
Among the various recommendations for sleep duration, we considered 11 h or more for pre-school children and 10 h or more for school children22 as target values.
The most generally accepted recommendation23 restricts TV viewing time to 1–2 h per day where the lower threshold applies to pre-school children, combining all screen-based activities.24
The evaluation of the original KINDL questionnaire does not provide an established target value in all the survey countries, so we decided to use the 85th percentile of the scale range (that is, 44 points) as threshold of an indicator for a good quality of life, which itself is considered as proxy for a balanced family life.
The recommended target value of MVPA for children ranges from 15 to 20 min in the Mediterranean countries, for example, Cyprus and Italy, to 90 min in Canada.25 The most widely accepted target value of 60 min MVPA26 was applied in our analysis.
On the basis of the internationally recommended target values described above, a compliance score was calculated adding up the number of those key messages for which the recommended target values were met. Hence, the values of the compliance score range from zero (no compliance at all) to six (fulfilling the recommendation for all six key messages). Achieving at least five points was considered as good compliance.
Quality management
All survey elements followed detailed standard operation procedures that were laid down in the general survey manual and finalised after the pre-test of all survey modules.
To check and improve the quality of data, the reliability of questionnaires was checked by re-administering the CEHQ and selected questions of the parental questionnaire in a convenience sample of study participants11 confirming an acceptable reproducibility even by more than 4 months between the first and second administration, without any systematic differences in reproducibility by sex and age. Food consumption assessed by the CEHQ was validated against selected nutrients measured in blood and urine,27 which revealed a significant positive correlation between reported intake and excretion. A methodological study was carried out to compare uniaxial and triaxial accelerometers in children and to validate them using doubly labelled water as the gold standard.28
Statistical analysis
On the basis of the above described variables and pre-defined cut-off points, we assessed country-specific means and s.d. and prevalences of compliance with each of the six key messages as well as country-specific distributions regarding the compliance score, stratified by pre-school/school and sex. All analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
The study population was already described in detail by Ahrens et al.29 The data were obtained from 8302 (physical activity) to 17 212 (screen time) children, according to the varying proportions of participation in the various modules. Information on all six behaviours was available for 5140 children (Figure 1). No noteworthy differences were found regarding the socio-demographic characteristics between the total sample and the various subpopulations according to the availability of data on the various key messages (Table 1).
Table 2 shows the sample size with respect to the key messages and summarises the observed behaviours. A positive trend with age can be observed for total screen time in the sense that older children spent more time in front of the TV or computer and for physical activity, whereas there is negative trend for fruit and vegetable intake, sleep time and the health-related quality of life score. In all countries, the total screen time was higher for boys than girls (in pre-school age: 1.53 vs 1.36 h per week; in school age 2.06 vs 1.76 h per week). Also, the mean daily duration of MVPA was higher for boys than for girls (in pre-school age: 38.2 vs 30.6 min; in school age 47.9 vs 36.2 min).
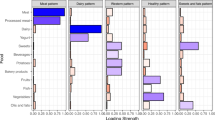
Table 3 demonstrates the compliance with the key messages. Overall, 52.5% of the children were in the highest category of water intake. The water consumption in southern countries was much higher than in central and northern European countries. Fruit and vegetable consumption was far below the recommended target value in all countries and age groups: the proportion of children who achieved the ‘5 a day’ recommendation was only 8.8%. Fruit and vegetable consumption were above average in Nordic countries and Cyprus. None of the diet-related key behaviours showed major differences by sex or age.
Total screen-based activities were below the recommended target value in 51.5% of all children with no major regional differences, girls having better compliance than boys (56.4% vs 46.6%). The recommended target value of MVPA was achieved in only 15.2% of the children, with threefold difference in the prevalence between countries (8.8% in Cyprus vs 25.7% in Sweden). The same order of magnitude in difference was observed according to sex: the proportion of children achieving the recommended target value of MVPA was higher among boys than among girls (in pre-school children 15.0% vs 4.5%; in school children 26.8% vs 10.5%).
Key messages promoting lifestyle changes to cope with stress indicate far better results in the northern region than in the southern region, especially among girls (see Table 3). In addition, we observed a negative trend with age for the health-related quality of life score.
The recommendation on sleep duration was fulfilled in 37.9% of our study sample. In both age groups and in all countries except Estonia, the prevalence of adherence to recommendation was better in girls.
Regarding the compliance score, the two extremes of the scale showed a sharp contrast: 0 and 1 points, that is, poor compliance, were observed for 37.6% in our study sample, whereas a good compliance with this set of lifestyle recommendations was observed in only 1.1% of the children. Figures 2 and 3 depict the distribution of the compliance score according to age, sex and country. The score showed a similar pattern as most of the key messages, that is, a better adherence of children to the six key messages in the northern countries and among younger age groups.
Discussion
The present paper investigated the adherence of European children to selected8,9,30 health behaviours known to be associated with childhood obesity and being essential for children's optimal and healthy development. The results demonstrate that surprisingly low proportions of these children meet the recommended target values of the investigated health behaviours (8.8–52.5%).
The consumption of sugar-sweetened beverages is an important contributor to childhood obesity31,32 confirmed even by longitudinal studies.33 In spite of this, there is no special recommendation regarding soft drink consumption. The WHO CINDI guideline simply proposes the limitation of sugary drinks. The review of Libuda and Kersting31 also underlined that the most reasonable preventive measure is replacing soft drinks by non-caloric beverages, for example, tap water and mineral water. In our study, half of the children showed a satisfactory water intake reflected by the highest category of intake frequency reported in the CEHQ. However, this also implies that almost half of the children do not drink enough water.
A low level of fruit and vegetable consumption among children is consistently reported. The position paper of the American Dietetic Association on Dietary Guidance for Healthy Children Ages 2 to 11 Years34 reported that 63 and 78% of children 2 to 9 years do not consume the recommended number of servings of fruits and vegetables. They found an average daily intake of two servings of fruits and 2.2 of vegetables. A recent review35 confirmed this observation, demonstrating low intakes of fruits and vegetables in most American, European and Australian studies, between 2 and 3 portions per day which are well below the recommended five portions. This target value of five portions should consider the age of the child, that is, the appropriate amount of fruits and vegetables depends on the energy needs, where for example, a young child should eat more than 200 g per day.21 In the Netherlands, more children complied with the World Health Organisation recommendation of 400 g fruits and vegetables per day (17.0%) in 2009 than in 2003 (11.8%, P=0.004).36 However, even the 2009 figures were lower than expected. Two German studies37 reported a fruit intake of 110 and 114 g in boys and girls, respectively, and a vegetable intake of 104 and 115 g; in total, 2.6–2.8 portions according to the WHO CINDI conversion. A British study38 revealed that the daily consumption of at least one portion of fruit and of vegetables in 9–10-year-old children was 56.8 and 49.9%, respectively. Results on the association of fruit and vegetable consumption and obesity are controversial in spite of their low energy density. Nevertheless, high fruit and vegetable consumption contributes to a well-balanced nutrient-containing diet. The data gained from the IDEFICS survey correspond to the results demonstrated by the studies discussed above. Fruit and vegetable consumption is very low in the participating European children, not even approaching the widely accepted internationally recommended target value of five times per day, where the proportion of adherers ranged from 2.5% in Belgium to 14.5% in Sweden, while in total 91.2% of the children have an intake lower than optimal. Fruit/vegetable intake does not differ substantially between age groups. It is worth mentioning that fruit/vegetable intake is relatively low even in the Mediterranean countries. On the basis of these data, we can state that plant food consumption should be highly promoted among European children.
Reviews concerning the relationship between TV time, sedentary time and obesity are equivocal;39 however, the majority of them confirm a positive association. Possible explanations are multifold,40 involving direct and indirect mechanisms contributing to the childhood obesity epidemic. Time spent on TV viewing potentially decreases the time spent in physical activity. Food proved to be the most frequently advertised product category on children's TV, the majority of these products being energy dense and nutrient poor.40 This facilitates adverse dietary patterns: energy-dense snack consumption, fast-food consumption, energy-dense drink intake, higher total energy intake and higher percentage energy from fat.41,42 Watching TV redirects attention from conscious eating and provides opportunity for unnoticed and unrestricted snacking.43 These arguments support the American Academy of Pediatrics Policy Statement suggesting that daily screen time should be restricted to 1–2 h, the lower limit applying for younger children.44 There is a positive trend with age for total screen time, but due to the duplication of permitted screen time, this does not cause an increase in non-compliance with the guidelines. The majority of studies reported a significant relationship between television viewing time and adverse dietary outcomes with as little as 1 h of daily television exposure.45 According to the present data the recommendation of<1 h of total screen time per day for pre-school children and<2 h per day for school children—not exclusively TV viewing—seems to be reasonable. These thresholds were reached by 51.5% of the IDEFICS population that was the second best compliance in the present study after compliance to water consumption.
Physical activity and sedentary behaviour are also considered important aetiological factors46 in childhood obesity. The beneficial effect of physical activity exceeds the simple prevention of overweight. It improves metabolic and mental health,47 besides, it is also positively associated with academic performance.48 There is a positive trend with age for compliance to physical activity recommendations in the IDEFICS population, but even school children’s physical activity levels are far below the recommended target value. The prevalence of spending more than 1 h per day in MVPA is overall very low, ranging from 6.8% in Italy to 25.7% in Sweden. Boys were more physically active than girls, which confirms previous findings49,50 where it is repeatedly stressed from an overall European perspective that girls are less likely to be suffciently physically active than boys.
Currently, there is a growing interest on how different aspects of family life affect children’s health. Although we did not explicitly measure, for instance, the stress level of the family, but various other indicators of the quality of family life instead, it is interesting to note that the stress level of the family can be an important contributor to childhood obesity,51, 52, 53 and the other way round, obesity may increase the stress level.54, 55, 56, 57, 58 Our cross-sectional study cannot identify causal relationships, though literature suggests that impaired mother–child relationship, reduced social support and parenting care may have a role in establishing adverse diet patterns. This puts in focus the relationships within the family confirming the results of our intervention mapping approach, which addressed stress management as one of the intervention targets for the IDEFICS study. The strengthening of a supportive family environment may have beneficial effects on stress coping and consequently on obesity. A negative trend with age was observed for the health-related quality of life score in the IDEFICS population, with lower values in the southern countries at all ages.
An increasing body of evidence suggests that shorter sleep duration is independently associated with weight gain, particularly in younger age groups.59 Investigation of sleep patterns in the IDEFICS study60 confirmed the association of sleep duration with obesity: a dose-dependant association between sleep duration and overweight was observed. A clear gradient in sleep duration could also be seen between regions: children from northern Europe sleep longer than children in southern Europe. Sleep duration has shown a decreasing trend in the past century, reflecting changing lifestyles.61 In our study, the age-specific recommendations were met by 7.5% of Estonian children up to 82.2% of Belgian children. On the basis of these results, we can conclude that striving for longer sleep duration among European children would be essential, and this should be promoted especially in the southern countries. Please note that we only recorded nocturnal sleep duration although sleep during the daytime might be relevant in Mediterranean countries where for instance napping after lunch is common, but this was not recorded in the IDEFICS study.
Several lifestyle factors are described as behavioural contributors to childhood obesity,30 which are often associated with each other. Regarding intervention targets, the literature typically deals separately with these factors. The advantage of combining the most important lifestyle factors in a compliance score may provide a more holistic view: complying with certain aspects of lifestyle recommendations can vary even within an individual, but these aspects can compensate each other, creating a final common effect on the outcome of obesity. The score can express the fulfilment of a comprehensive set of recommended behavioural factors, such as in the present study the compliance with the six key messages of the IDEFICS intervention. Our data revealed that an almost complete compliance (that is, five or six messages) with recommendations is rare among European youth: the range is 0 (Cyprus) to 2.8% (Germany) with 1.1% prevalence in the total IDEFICS population. The distribution of the compliance score was different between countries and compliance increased with age.
The strength of the present study is its large sample size with wide geographical coverage of Europe. The study was carefully planned and performed a standardised and quality-controlled data collection. One limitation of the present analysis may be that the children participating in the various modules were not a random sample of the overall study population. However, there were no apparent differences in the socio-demographic profile between the responders and non-responders to the various modules. Another limitation is the reliance on self-reports with respect to variables where an objective assessment or a direct measurement was not feasible in such a large population-based study. This was for instance the case for questions that were related to family life. Furthermore, the relationship of our key message to improve the quality of family life and the newly developed quality of life score has not been directly shown. But as the quality of life score used in this paper contains a module characterising the quality of family relations (taken from the original KINDL questionnaire), we are quite confident that its use is valid for indicating the key message with respect to an improved quality of family life.
Conclusion
The compliance of young children to health-behaviour recommendations was very low and should therefore be improved, preferably via those actors who can serve as a role model, mediator for the different lifestyle aspects or nutritional gatekeeper for the children. The present paper directs the attention to the gap between the present and the required situation. Further studies are needed to define evidence-based target values for a healthy development of children.
References
Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 2005; 352: 1138–1145.
Lobstein T, Baur L, Uauy R . Obesity in children and young people: a crisis in public health. Obes Rev 2004; 5 (Suppl 1): 4–104.
Olds T, Maher C, Zumin S, Peneau S, Lioret S, Castetbon K et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 2011; 6: 342–360.
The European health report 2005 Public health action for healthier children and populations. World Health Organization Regional Office for Europe, 2005.
Haynos AF, O'Donohue WT . Universal childhood and adolescent obesity prevention programs: review and critical analysis. Clin Psychol Rev 2012; 32: 383–399.
Ahrens W, Bammann K, de Henauw S, Halford J, Palou A, Pigeot I et al. Understanding and preventing childhood obesity and related disorders—IDEFICS: a European multilevel epidemiological approach. Nutr Metab Cardiovasc Dis 2006; 16: 302–308.
Verbestel V, De Henauw S, Maes L, Haerens L, Marild S, Eiben G et al. Using the intervention mapping protocol to develop a community-based intervention for the prevention of childhood obesity in a multi-centre European project: the IDEFICS intervention. Int J Behav Nutr Phys Act 2011; 8: 82.
De Henauw S, Verbestel V, Marild S, Barba G, Bammann K, Eiben G et al. The IDEFICS community-oriented intervention programme: a new model for childhood obesity prevention in Europe? Int J Obes (Lond) 2011; 35 (Suppl 1): S16–S23.
Brown T, Kelly S, Summerbell C . Prevention of obesity: a review of interventions. Obes Rev 2007; 8 (Suppl 1): 127–130.
Ahrens W, Bammann K, Siani A, Buchecker K, De Henauw S, Iacoviello L et al. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes (Lond) 2011; 35 (Suppl 1): S3–S15.
Lanfer A, Hebestreit A, Ahrens W, Krogh V, Sieri S, Lissner L et al. Reproducibility of food consumption frequencies derived from the Children's Eating Habits Questionnaire used in the IDEFICS study. Int J Obes (Lond) 2011; 35: S61–S68.
Ravens-Sieberer U, Bullinger M . KINDL-R. Fragebogen zur Erfassung der gesundheitsbezogenen Lebensqualität bei Kindern und Jugendlichen. Revidierte Form Manual, 2000. http://www.kindl.org/deutsch/manual/.
Pigeot I, Pohlabeln H, Gwozdz W . Stress coping and relaxation. 22nd Workshop of European Childhood Obesity Group: Palma de Mallorca, Spain, 17–19 October 2012.
Ravens-Sieberer U, Ellert U, Erhart M . [Health-related quality of life of children and adolescents in Germany. Norm data from the German Health Interview and Examination Survey (KiGGS)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007; 50: 810–818.
Ojiambo R, Konstabel K, Veidebaum T, Reilly J, Verbestel V, Huybrechts I et al. Validity of hip-mounted uniaxial accelerometry with heart-rate monitoring vs triaxial accelerometry in the assessment of free-living energy expenditure in young children: the IDEFICS Validation Study. J Appl Physiol 2012; 113: 1530–1536.
Ojiambo R, Cuthill R, Budd H, Konstabel K, Casajus JA, Gonzalez-Aguero A et al. Impact of methodological decisions on accelerometer outcome variables in young children. Int J Obes (Lond) 2011; 35 (Suppl 1): S98–S103.
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA . Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011; 43: 1360–1368.
Konstabel K, Veidebaum T, Verbestel V, Moreno LA, Bammann K, Tornaritis M et al. Objectively measured physical activity in European children: the IDEFICS study. Int J Obes (Lond) 2014; 38 (Suppl 2): S135–S143.
Beckmann SC, Reisch LA, Bendixen LC . IDEFICS Consortium. Report on existing guidelines. Deliverable 8.1, IDEFICS study, 2007. http://www.idefics.eu/Idefics/UserFiles/File/D8_1_ExistingGuidelines_Final.pdf (last access May 2014).
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific opinion on dietary reference values for water. EFSA Journal 2010; 8: 1459 (http://www.efsa.europa.eu/en/efsajournal/pub/1459.htm).
CINDI Dietary Guide. WHO Regional Office for Europe: Copenhagen, 2000. Available at http://www.euro.who.int/__data/assets/pdf_file/0010/119926/E70041.pdf.
Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS . Children's sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep 2013; 36: 527–534.
American Academy of Pediatrics. Committee on Public Education. American Academy of Pediatrics: Children, adolescents, and television. Pediatrics 2001; 107: 423–426.
Lissner L, Lanfer A, Gwozdz W, Olafsdottir S, Eiben G, Moreno LA et al. Television habits in relation to overweight, diet and taste preferences in European children: the IDEFICS study. Eur J Epidemiol 2012; 27: 705–715.
Global Recommendations on Physical Activity for Health. World Health Organization: Geneva, 2010. http://whqlibdoc.who.int/publications/2010/9789241599979_eng.pdf
Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B et al. Evidence based physical activity for school-age youth. J Pediatr 2005; 146: 732–737.
Huybrechts I, Bornhorst C, Pala V, Moreno LA, Barba G, Lissner L et al. Evaluation of the Children's Eating Habits Questionnaire used in the IDEFICS study by relating urinary calcium and potassium to milk consumption frequencies among European children. Int J Obes (Lond) 2011; 35 (Suppl 1): S69–S78.
Bammann K, Sioen I, Huybrechts I, Casajus JA, Vicente-Rodriguez G, Cuthill R et al. The IDEFICS validation study on field methods for assessing physical activity and body composition in children: design and data collection. Int J Obes (Lond) 2011; 35 (Suppl 1): S79–S87.
Ahrens W, Pigeot I, Pohlabeln H, De Henauw S, Lissner L, Molnár D et al. Prevalence of overweight and obesity in European children below the age of 10. Int J Obes (Lond) 2014; 38 (Suppl 2): S99–S107.
Sherry B . Food behaviors and other strategies to prevent and treat pediatric overweight. Int J Obes (Lond) 2005; 29 (Suppl 2): S116–S126.
Libuda L, Kersting M . Soft drinks and body weight development in childhood: is there a relationship? Curr Opin Clin Nutr Metab Care 2009; 12: 596–600.
Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Mihatsch W et al. Role of dietary factors and food habits in the development of childhood obesity: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2011; 52: 662–669.
Moreno LA, Rodriguez G . Dietary risk factors for development of childhood obesity. Curr Opin Clin Nutr Metab Care 2007; 10: 336–341.
Nicklas T, Johnson R . Position of the American Dietetic Association: Dietary guidance for healthy children ages 2 to 11 years. J Am Diet Assoc 2004; 104: 660–677.
Evans CE, Christian MS, Cleghorn CL, Greenwood DC, Cade JE . Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am J Clin Nutr 2012; 96: 889–901.
Fischer C, Brug J, Tak NI, Yngve A, te Velde SJ . Differences in fruit and vegetable intake and their determinants among 11-year-old schoolchildren between 2003 and 2009. Int J Behav Nutr Phys Act 2011; 8: 141.
Sausenthaler S, Standl M, Buyken A, Rzehak P, Koletzko S, Bauer CP et al. Regional and socio-economic differences in food, nutrient and supplement intake in school-age children in Germany: results from the GINIplus and the LISAplus studies. Public Health Nutr 2011; 14: 1724–1735.
van Sluijs EM, Skidmore PM, Mwanza K, Jones AP, Callaghan AM, Ekelund U et al. Physical activity and dietary behaviour in a population-based sample of British 10-year old children: the SPEEDY study (Sport, Physical activity and Eating behaviour: environmental Determinants in Young people). BMC Public Health 2008; 8: 388.
Chinapaw MJ, Proper KI, Brug J, van Mechelen W, Singh AS . Relationship between young peoples' sedentary behaviour and biomedical health indicators: a systematic review of prospective studies. Obes Rev 2011; 12: e621–e632.
Coon KA, Tucker KL . Television and children's consumption patterns. A review of the literature. Minerva Pediatr 2002; 54: 423–436.
Pearson N, Biddle SJ . Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med 2011; 41: 178–188.
Santaliestra-Pasias AM, Mouratidou T, Verbestel V, Huybrechts I, Gottrand F, Le Donne C et al. Food consumption and screen-based sedentary behaviors in European adolescents: the HELENA study. Arch Pediatr Adolesc Med 2012; 166: 1010–1020.
Boulos R, Vikre EK, Oppenheimer S, Chang H, Kanarek RB . ObesiTV: how television is influencing the obesity epidemic. Physiol Behav 2012; 107: 146–153.
From the American Academy of Pediatrics. Policy Statement. Children, Adolescents, and the Media. Council on communications and media. Pediatrics 2013; 132: 958–961.
Ford C, Ward D, White M . Television viewing associated with adverse dietary outcomes in children ages 2-6. Obes Rev 2012; 13: 1139–1147.
Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev 2010; 11: 695–708.
Janssen I, Leblanc AG . Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010; 7: 40.
Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ . Physical activity and performance at school: a systematic review of the literature including a methodological quality assessment. Arch Pediatr Adolesc Med 2012; 166: 49–55.
Ortlieb S, Schneider G, Koletzko S, Berdel D, von Berg A, Bauer CP et al. Physical activity and its correlates in children: a cross-sectional study (the GINIplus & LISAplus studies). BMC Public Health 2013; 13: 349.
Guinhouya BC, Samouda H, de Beaufort C . Level of physical activity among children and adolescents in Europe: a review of physical activity assessed objectively by accelerometry. Public Health 2013; 127: 301–311.
Koch FS, Sepa A, Ludvigsson J . Psychological stress and obesity. J Pediatr 2008; 153: 839–844.
Puder JJ, Munsch S . Psychological correlates of childhood obesity. Int J Obes (Lond) 2010; 34 (Suppl 2): S37–S43.
Gundersen C, Mahatmya D, Garasky S, Lohman B . Linking psychosocial stressors and childhood obesity. Obes Rev 2011; 12: e54–e63.
Cornette R . The emotional impact of obesity on children. Worldviews Evid Based Nurs 2008; 5: 136–141.
Atlantis E, Baker M . Obesity effects on depression: systematic review of epidemiological studies. Int J Obes (Lond) 2008; 32: 881–891.
Wardle J, Cooke L . The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab 2005; 19: 421–440.
Tsiros MD, Olds T, Buckley JD, Grimshaw P, Brennan L, Walkley J et al. Health-related quality of life in obese children and adolescents. Int J Obes (Lond) 2009; 33: 387–400.
Strauss RS, Pollack HA . Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003; 157: 746–752.
Patel SR, Hu FB . Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008; 16: 643–653.
Hense S, Pohlabeln H, De Henauw S, Eiben G, Molnar D, Moreno LA et al. Sleep duration and overweight in European children: is the association modified by geographic region?b Sleep 2011; 34: 885–890.
Matricciani L, Olds T, Petkov J . In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev 2012; 16: 203–211.
Acknowledgements
This work was done as a part of the IDEFICS study (www.idefics.eu). We gratefully acknowledge the financial support of the European Community within the Sixth RTD Framework Programme Contract No. 016181 (FOOD). We are grateful to the Volkswagen Foundation that financially supported the production of this supplement. We are grateful to all participating children and their families, to their teachers and communities supporting the recruitment and completion of the examinations and to the researchers and field workers of the IDEFICS study. The support and discussion with the Diet Panel and Guideline Panel of the IDFFICS Consortium was most helpful. LL has received grant support from VR, FORTE and FORMAS (research councils in Sweden).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The information in this document reflects the author's view and is provided as is. Additional data, for example, regarding sex differences, can be obtained from the author on request.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Kovács, E., Siani, A., Konstabel, K. et al. Adherence to the obesity-related lifestyle intervention targets in the IDEFICS study. Int J Obes 38 (Suppl 2), S144–S151 (2014). https://doi.org/10.1038/ijo.2014.145
Published:
Issue date:
DOI: https://doi.org/10.1038/ijo.2014.145
This article is cited by
-
Intervention effects of a school-based health promotion programme on children’s nutrition behaviour
Journal of Public Health (2023)
-
Development and evaluation study of FLY-Kids: a new lifestyle screening tool for young children
European Journal of Pediatrics (2023)
-
Supportive treatment of vascular dysfunction in pediatric subjects with obesity: the OBELIX study
Nutrition & Diabetes (2022)
-
Effects of nutrition intervention strategies in the primary prevention of overweight and obesity in school settings: a protocol for a systematic review and network meta-analysis
Systematic Reviews (2021)
-
Diagnosis, treatment and prevention of pediatric obesity: consensus position statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics
Italian Journal of Pediatrics (2018)