Abstract
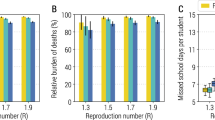
The threat posed by the highly pathogenic H5N1 influenza virus requires public health authorities to prepare for a human pandemic. Although pre-pandemic vaccines and antiviral drugs might significantly reduce illness rates1,2, their stockpiling is too expensive to be practical for many countries. Consequently, alternative control strategies, based on non-pharmaceutical interventions, are a potentially attractive policy option. School closure is the measure most often considered. The high social and economic costs of closing schools for months make it an expensive and therefore controversial policy, and the current absence of quantitative data on the role of schools during influenza epidemics means there is little consensus on the probable effectiveness of school closure in reducing the impact of a pandemic. Here, from the joint analysis of surveillance data and holiday timing in France, we quantify the role of schools in influenza epidemics and predict the effect of school closure during a pandemic. We show that holidays lead to a 20–29% reduction in the rate at which influenza is transmitted to children, but that they have no detectable effect on the contact patterns of adults. Holidays prevent 16–18% of seasonal influenza cases (18–21% in children). By extrapolation, we find that prolonged school closure during a pandemic might reduce the cumulative number of cases by 13–17% (18–23% in children) and peak attack rates by up to 39–45% (47–52% in children). The impact of school closure would be reduced if it proved difficult to maintain low contact rates among children for a prolonged period.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ferguson, N. M. et al. Strategies for mitigating an influenza pandemic. Nature 442, 448–452 (2006)
Germann, T. C., Kadau, K., Longini, I. M. & Macken, C. A. Mitigation strategies for pandemic influenza in the United States. Proc. Natl Acad. Sci. USA 103, 5935–5940 (2006)
Bell, D. M. Non-pharmaceutical interventions for pandemic influenza, national and community measures. Emerg. Infect. Dis. 12, 88–94 (2006)
Heymann, A., Chodick, G., Reichman, B., Kokia, E. & Laufer, J. Influence of school closure on the incidence of viral respiratory diseases among children and on health care utilization. Pediatr. Infect. Dis. J. 23, 675–677 (2004)
Valleron, A. J., Flahault, A. & Boelle, P. Y. Do school holidays have an impact on influenza epidemics, then on mortality? Presentation at International Conference on Options for the Control of Influenza V (Okinawa, 7–11 October 2003); 〈http://www.u707.jussieu.fr/valleron/dia/dia2003/okinawa.pdf〉
Glass, R., Glass, L., Beyeler, W. & Min, H. Targeted social distancing design for pandemic influenza. Emerg. Infect. Dis. 12, 1671–1681 (2006)
Valleron, A. J. et al. A computer network for the surveillance of communicable diseases: the French experiment. Am. J. Public Health 76, 1289–1292 (1986)
Flahault, A. et al. Virtual surveillance of communicable diseases: a 20-year experience in France. Stat. Methods Med. Res. 15, 413–421 (2006)
Longini, I. M., Koopman, J. S., Haber, M. & Cotsonis, G. A. Statistical inference for infectious diseases. Risk-specific household and community transmission parameters. Am. J. Epidemiol. 128, 845–859 (1988)
Cauchemez, S., Carrat, F., Viboud, C., Valleron, A. J. & Boelle, P. Y. A. Bayesian MCMC approach to study transmission of influenza: application to household longitudinal data. Stat. Med. 23, 3469–3487 (2004)
Denoeud, L. et al. Predicting pneumonia and influenza mortality from morbidity data. PLoS One 2, e464 (2007)
Glezen, W. P. et al. Age distribution of patients with medically-attended illnesses caused by sequential variants of influenza A/H1N1: comparison to age-specific infection rates, 1978–1989. Am. J. Epidemiol. 133, 296–304 (1991)
Monto, A. S. & Sullivan, K. M. Acute respiratory illness in the community. Frequency of illness and the agents involved. Epidemiol. Infect. 110, 145–160 (1993)
Olson, D. R. et al. Monitoring the impact of influenza by age: emergency department fever and respiratory complaint surveillance in New York City. PLoS Med. 4, e247 (2007)
Bootsma, M. C. J. & Ferguson, N. M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc. Natl Acad. Sci. USA 104, 7588–7593 (2007)
Hatchett, R. J., Mecher, C. E. & Lipsitch, M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl Acad. Sci. USA 104, 7582–7587 (2007)
Markel, H. et al. Nonpharmaceutical interventions implemented by US cities during the 1918–1919 influenza pandemic. J. Am. Med. Assoc. 298, 644–654 (2007)
Finkenstadt, B. F., Morton, A. & Rand, D. A. Modelling antigenic drift in weekly flu incidence. Stat. Med. 24, 3447–3461 (2005)
Xia, Y., Gog, J. R. & Grenfell, B. Semiparametric estimation of the duration of immunity from infectious disease time series: influenza as a case-study. J. R. Stat. Soc. Ser. C 54, 659–672 (2005)
Doucet, A., de Freitas, N. & Gordon, N. Sequential Monte Carlo Methods in Practice (Springer, New York, 2001)
Liu, J. S. Monte Carlo Strategies in Scientific Computing (Springer, New York, 2001)
Gilks, W. R., Richardson, S. & Spiegelhalter, D. J. Markov Chain Monte Carlo in Practice (Chapman and Hall, London, 1996)
Acknowledgements
We thank the MRC, European Union FP6 SARSTRANS and INFTRANS projects, RCUK, and the NIGMS MIDAS initiative for research funding. We thank F. Carrat for comments.
Author Contributions S.C. developed the transmission model and conceived and implemented the inference framework used, did the analysis and drafted and revised the text. All other authors edited or commented on the text. A.-J.V., P.-Y.B. and A.F. identified, collated and processed the surveillance and holiday data. P.-Y.B. also provided input on the statistical framework. N.M.F. conceived the study (building on earlier work by A.-J.V. and A.F. examining the correlation between holidays and seasonal influenza incidence), provided input on the statistical framework, model design and assumptions and gave other technical advice.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary information
The file contains extensive Supplementary Notes illustrated with Supplementary Figures and Tables and additional references. (PDF 615 kb)
Rights and permissions
About this article
Cite this article
Cauchemez, S., Valleron, AJ., Boëlle, PY. et al. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature 452, 750–754 (2008). https://doi.org/10.1038/nature06732
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1038/nature06732
This article is cited by
-
Impact of non-pharmaceutical interventions during COVID-19 on future influenza trends in Mainland China
BMC Infectious Diseases (2023)
-
Transmission dynamics of seasonal influenza in a remote island population
Scientific Reports (2023)
-
Changes in school feeding operations during the COVID-19 pandemic: evidence from 139 countries
Food Security (2023)
-
The Effects of Climatological Factors on Global Influenza Across Temperate and Tropical Regions
Mobile Networks and Applications (2023)
-
A sharp decrease in reported non-COVID-19 notifiable infectious diseases during the first wave of the COVID-19 epidemic in the Rotterdam region, the Netherlands: a descriptive study
BMC Infectious Diseases (2022)