Abstract
Many human genetic associations with resistance to malaria have been reported, but few have been reliably replicated. We collected data on 11,890 cases of severe malaria due to Plasmodium falciparum and 17,441 controls from 12 locations in Africa, Asia and Oceania. We tested 55 SNPs in 27 loci previously reported to associate with severe malaria. There was evidence of association at P < 1 × 10−4 with the HBB, ABO, ATP2B4, G6PD and CD40LG loci, but previously reported associations at 22 other loci did not replicate in the multicenter analysis. The large sample size made it possible to identify authentic genetic effects that are heterogeneous across populations or phenotypes, with a striking example being the main African form of G6PD deficiency, which reduced the risk of cerebral malaria but increased the risk of severe malarial anemia. The finding that G6PD deficiency has opposing effects on different fatal complications of P. falciparum infection indicates that the evolutionary origins of this common human genetic disorder are more complex than previously supposed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Haldane, J.B.S. Disease and evolution. Ric. Sci. Suppl. A 19, 68–76 (1949).
Allison, A.C. Protection afforded by sickle-cell trait against subtertian malarial infection. BMJ 1, 290–294 (1954).
Allison, A.C. Genetic factors in resistance to malaria. Ann. NY Acad. Sci. 91, 710–729 (1961).
Bienzle, U., Ayeni, O., Lucas, A.O. & Luzzatto, L. Glucose-6-phosphate dehydrogenase and malaria. Greater resistance of females heterozygous for enzyme deficiency and of males with non-deficient variant. Lancet 1, 107–110 (1972).
Ruwende, C. et al. Natural selection of hemi- and heterozygotes for G6PD deficiency in Africa by resistance to severe malaria. Nature 376, 246–249 (1995).
Tishkoff, S.A. et al. Haplotype diversity and linkage disequilibrium at human G6PD: recent origin of alleles that confer malarial resistance. Science 293, 455–462 (2001).
Kwiatkowski, D.P. How malaria has affected the human genome and what human genetics can teach us about malaria. Am. J. Hum. Genet. 77, 171–192 (2005).
Verra, F., Mangano, V.D. & Modiano, D. Genetics of susceptibility to Plasmodium falciparum: from classical malaria resistance genes towards genome-wide association studies. Parasite Immunol. 31, 234–253 (2009).
Hedrick, P.W. Population genetics of malaria resistance in humans. Heredity (Edinb.) 107, 283–304 (2011).
Malaria Genomic Epidemiology Network. A global network for investigating the genomic epidemiology of malaria. Nature 456, 732–737 (2008).
World Health Organization. Severe falciparum malaria. Trans. R. Soc. Trop. Med. Hyg. 94 (suppl. 1), S1–S90 (2000).
World Health Organization. Guidelines for the Treatment of Malaria 2nd edn. (World Health Organization, Geneva, 2010).
Marsh, K. et al. Indicators of life-threatening malaria in African children. N. Engl. J. Med. 332, 1399–1404 (1995).
Taylor, T. et al. Standardized data collection for multi-center clinical studies of severe malaria in African children: establishing the SMAC network. Trans. R. Soc. Trop. Med. Hyg. 100, 615–622 (2006).
Jallow, M. et al. Clinical features of severe malaria associated with death: a 13-year observational study in The Gambia. PLoS ONE 7, e45645 (2012).
Chokshi, D.A. et al. Valid consent for genomic epidemiology in developing countries. PLoS Med. 4, e95 (2007).
Parker, M. et al. Ethical data release in genome-wide association studies in developing countries. PLoS Med. 6, e1000143 (2009).
Snow, R.W. et al. Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. Lancet 349, 1650–1654 (1997).
Reyburn, H. et al. Association of transmission intensity and age with clinical manifestations and case fatality of severe Plasmodium falciparum malaria. J. Am. Med. Assoc. 293, 1461–1470 (2005).
Yamamoto, F., Clausen, H., White, T., Marken, J. & Hakomori, S. Molecular genetic basis of the histo-blood group ABO system. Nature 345, 229–233 (1990).
Ogasawara, K. et al. Molecular genetic analysis of variant phenotypes of the ABO blood group system. Blood 88, 2732–2737 (1996).
Fry, A.E. et al. Common variation in the ABO glycosyltransferase is associated with susceptibility to severe Plasmodium falciparum malaria. Hum. Mol. Genet. 17, 567–576 (2008).
Cappellini, M.D. & Fiorelli, G. Glucose-6-phosphate dehydrogenase deficiency. Lancet 371, 64–74 (2008).
Hirono, A. & Beutler, E. Molecular cloning and nucleotide sequence of cDNA for human glucose-6-phosphate dehydrogenase variant A. Proc. Natl. Acad. Sci. USA 85, 3951–3954 (1988).
Clark, T.G. et al. Allelic heterogeneity of G6PD deficiency in West Africa and severe malaria susceptibility. Eur. J. Hum. Genet. 17, 1080–1085 (2009).
Timmann, C. et al. Genome-wide association study indicates two novel resistance loci for severe malaria. Nature 489, 443–446 (2012).
Sabeti, P. et al. CD40L association with protection from severe malaria. Genes Immun. 3, 286–291 (2002).
Hirschhorn, J.N., Lohmueller, K., Byrne, E. & Hirschhorn, K. A comprehensive review of genetic association studies. Genet. Med. 4, 45–61 (2002).
Williams, T.N. et al. Negative epistasis between the malaria-protective effects of α+-thalassemia and the sickle cell trait. Nat. Genet. 37, 1253–1257 (2005).
Atkinson, S.H. et al. Epistasis between the haptoglobin common variant and α+thalassemia influences risk of severe malaria in Kenyan children. Blood 123, 2008–2016 (2014).
Steinberg, M.H., Eaton, J.W., Berger, E., Coleman, M.B. & Oelshlegel, F.J. Erythrocyte calcium abnormalities and the clinical severity of sickling disorders. Br. J. Haematol. 40, 533–539 (1978).
Band, G. et al. Imputation-based meta-analysis of severe malaria in three African populations. PLoS Genet. 9, e1003509 (2013).
Fairhurst, R.M. et al. Abnormal display of PfEMP-1 on erythrocytes carrying haemoglobin C may protect against malaria. Nature 435, 1117–1121 (2005).
Bunn, H.F. The triumph of good over evil: protection by the sickle gene against malaria. Blood 121, 20–25 (2013).
Cserti, C.M. & Dzik, W.H. The ABO blood group system and Plasmodium falciparum malaria. Blood 110, 2250–2258 (2007).
Rowe, J.A. et al. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc. Natl. Acad. Sci. USA 104, 17471–17476 (2007).
Teo, Y.Y., Small, K.S. & Kwiatkowski, D.P. Methodological challenges of genome-wide association analysis in Africa. Nat. Rev. Genet. 11, 149–160 (2010).
Teo, Y.Y. et al. Genome-wide comparisons of variation in linkage disequilibrium. Genome Res. 19, 1849–1860 (2009).
Luzzatto, L. G6PD deficiency and malaria selection. Heredity 108, 456 (2012).
Menendez, C., Fleming, A.F. & Alonso, P.L. Malaria-related anaemia. Parasitol. Today 16, 469–476 (2000).
Weatherall, D.J. & Kwiatkowski, D. Hematologic disorders of children in developing countries. Pediatr. Clin. North Am. 49, 1149–1164 (2002).
Calis, J.C. et al. Severe anemia in Malawian children. N. Engl. J. Med. 358, 888–899 (2008).
Howes, R.E., Battle, K.E., Satyagraha, A.W., Baird, J.K. & Hay, S.I. G6PD deficiency: global distribution, genetic variants and primaquine therapy. Adv. Parasitol. 81, 133–201 (2013).
Price, R.N. et al. Vivax malaria: neglected and not benign. Am. J. Trop. Med. Hyg. 77, 79–87 (2007).
Louicharoen, C. et al. Positively selected G6PD-Mahidol mutation reduces Plasmodium vivax density in Southeast Asians. Science 326, 1546–1549 (2009).
Guerra, C.A. et al. The international limits and population at risk of Plasmodium vivax transmission in 2009. PLoS Negl. Trop. Dis. 4, e774 (2010).
Liu, W. et al. African origin of the malaria parasite Plasmodium vivax. Nat. Commun. 5, 3346 (2014).
Miller, L.H., Mason, S.J., Clyde, D.F. & McGinniss, M.H. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N. Engl. J. Med. 295, 302–304 (1976).
Hamblin, M.T., Thompson, E.E. & Di Rienzo, A. Complex signatures of natural selection at the Duffy blood group locus. Am. J. Hum. Genet. 70, 369–383 (2002).
Apinjoh, T.O. et al. Association of cytokine and Toll-like receptor gene polymorphisms with severe malaria in three regions of Cameroon. PLoS ONE 8, e81071 (2013).
Manjurano, A. et al. Candidate human genetic polymorphisms and severe malaria in a Tanzanian population. PLoS ONE 7, e47463 (2012).
Dunstan, S.J. et al. Variation in human genes encoding adhesion and proinflammatory molecules are associated with severe malaria in the Vietnamese. Genes Immun. 13, 503–508 (2012).
Toure, O. et al. Candidate polymorphisms and severe malaria in a Malian population. PLoS ONE 7, e43987 (2012).
Vallone, P.M., Decker, A.E. & Butler, J.M. Allele frequencies for 70 autosomal SNP loci with U.S. Caucasian, African-American, and Hispanic samples. Forensic Sci. Int. 149, 279–286 (2005).
Clayton, D. Testing for association on the X chromosome. Biostatistics 9, 593–600 (2008).
Cordell, H.J. Detecting gene-gene interactions that underlie human diseases. Nat. Rev. Genet. 10, 392–404 (2009).
Acknowledgements
The MalariaGEN Project is supported by the Wellcome Trust (WT077383/Z/05/Z) and the Bill and Melinda Gates Foundation through The Foundation for the National Institutes of Health (FNIH, USA) (566) as part of the Grand Challenges in Global Health Initiative. The Resource Centre for Genomic Epidemiology of Malaria is supported by the Wellcome Trust (090770/Z/09/Z). This research was supported by the UK Medical Research Council (G0600718 and G0600230) and by the Wellcome Trust Biomedical Ethics Enhancement Award (087285) and Strategic Award (096527). D.P.K. receives support from the UK Medical Research Council (G19/9). C.C.A.S. was supported by a Wellcome Trust Career Development Fellowship (097364/Z/11/Z). The Wellcome Trust also provides core awards to the Wellcome Trust Centre for Human Genetics (090532/Z/09/Z) and the Wellcome Trust Sanger Institute (098051/Z/05/Z). The Malaria Research and Training Center–Bandiagara Malaria Project (MRTC-BMP) in Mali group is supported by an Interagency Committee on Disability Research (ICDR) grant from the National Institute of Allergy and Infectious Diseases/US National Institutes of Health (NIAID/NIH) to the University of Maryland and the University of Bamako (USTTB) and by the Mali-NIAID/NIH International Centers for Excellence in Research (ICER) at USTTB. Contributions from Nigeria to CP1 were supported financially by a grant within the BioMalPar European Network of Excellence (LSHP-CT-2004-503578). E.A. received partial funding from the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement 242095-EVIMalaR and the Central African Network for Tuberculosis, HIV/AIDS and Malaria (CANTAM) funded by the European and Developing Countries Clinical Trials Partnership (EDCTP). T.N.W. is funded by Senior Fellowship awards from the Wellcome Trust (076934/Z/05/Z and 091758/Z/10/Z) and through the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement 242095-EVIMalaR. The Kenya Medical Research Institute (KEMRI)–Wellcome Trust Programme is funded through core support from the Wellcome Trust. This paper is published with the permission of the director of KEMRI. C.M.N. is supported through a strategic award to the KEMRI–Wellcome Trust Programme from the Wellcome Trust (084538). The Joint Malaria Programme, Kilimanjaro Christian Medical Centre in Tanzania received funding from a UK MRC grant (G9901439). We would like to thank all the Vietnamese individuals who agreed to provide samples for this study. We acknowledge the work of the clinical staff from the Hospital of Tropical Diseases, HCMC and Phuoc Long and Dong Xoai District Hospitals in Binh Phuoc province, Vietnam, who initially diagnosed and studied the individuals with severe malaria. We would like to thank N.T. Hieu and his staff from Hung Vuong Obstetric Hospital for the collection of the cord blood controls. The clinical component of this study was funded through the Wellcome Trust Major Overseas Program in Vietnam (089276/Z/09/Z). L.M. was supported through Basser (Royal Australasian College of Physicians) and National Health and Medical Research Council (NHMRC) scholarships. M.L. was supported through a Fogarty Foundation Scholarship. T.M.E.D. was supported through an NHMRC practitioner fellowship.
Author information
Authors and Affiliations
Consortia
Contributions
All senior authors from each partner site have approved the final manuscript and their site authorship, acknowledgments and full contributors list. Writing group: G.M.C., D.P.K., S.M., K.A.R. and C.C.A.S. Project management: E.A., T. Agbenyega, S.A., A.A., O.A., K.A.B., D.J.C., V.C., T.M.E.D., O.D., C.D., S.J.D., J.F., T.T.H., K.J.J., H.K., A.K., S.K., K.A.K., D.P.K., K.M., P.M., D.M., M.M., I.M., A. Niangaly, N.P., M. Pinder, B.P., H.R., E.R., K.A.R., P.S., S.B.S., G.S., S.S., T.T., M.A.T., T.N.W. and M.D.W. Sample clinical data collection and management: S.A., A.A., L.N.A.-E., O.A., T. Apinjoh, K.A.B., E.C.B., G.M.C., D.J.C., S.J.D., A.E., J.E., K.F., A. Ghansah, L.H., M.J., D.K., H.K., A.K., S.K., M.L., A. Macharia, V.D.M., A. Manjurano, L.M., P.M., S.M., R.M., A. Niangaly, C.M.N., A. Ndi, V.N., S.O., N.P., N.H.P., M. Pinder, B.P., N.T.N.Q., H.R., K.A.R., M.S., G.S., F.S.-J., S.S., T.T., C.Q.T., M.A.T., O.T., S. Usen, S. Uyoga and A.V. Sample processing, genotyping and management: A.A., L.N.A.-E., O.A., T. Apinjoh, E.C.B., R.C., A.E., A. Ghansah, A. Green, L.H., C.H., M.J., A.E.J., D.K., H.K., M.L., A. Macharia, V.D.M., A. Manjurano, L.M., S.M., R.M., A. Niangaly, C.M.N., A. Ndi, V.N., S.O., N.H.P., N.T.N.Q., K.A.R., K.R., F.S.-J., C.Q.T., O.T., S. Uyoga and A.V. Analysis: G.B., T.G.C., G.M.C., D.P.K., S.Q.L., S.M., M. Pirinen, K.A.R., N.S. and C.C.A.S. Full details on contribution are given in the supplementary material.
Corresponding authors
Ethics declarations
Competing interests
The author declare no competing financial interests.
Integrated supplementary information
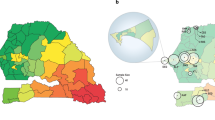
Supplementary Figure 1 Map of the locations of the MalariaGEN Partner Study sites involved in this project.
1. UK Resource Centre, Oxford University and Wellcome Trust Sanger Institute. 2. The Gambia, MRC Laboratories, Banjul. 3. Mali, University of Bamako, Bamako. 4. Burkina Faso, Centre National de Recherche et de Formation sur le Paludisme, Ouagadougou. 5. Ghana (Navrongo), Navrongo Memorial Institute for Medical Research with Navrongo Health Research Centre. 6. Ghana (Kumasi), Kwame Nkrumah University of Science and Technology. 7. Nigeria, University of Ibadan.8. Cameroon, University of Buea. 9. Kenya, KEMRI–Wellcome Research Programme, Kilifi. 10. Tanzania, Joint Malaria Programme, Kilimanjaro Christian Medical Centre, Moshi. 11. Malawi, Blantyre Malaria Project with Malawi-Liverpool–Wellcome Programme. 12. Vietnam, Oxford University Clinical Research Unit, Ho Chi Minh City. 13. Papua New Guinea, Papua New Guinea Institute for Medical Research, Madang. See also Supplementary Tables 1 and 2.
Supplementary Figure 2 Chromosomal map of the genes included in Supplementary Tables 5–7.
All genes are referenced to GRCh37, dbSNP137 and Ensembl build 73.
Supplementary Figure 3 Distribution of P values from multiple-association analyses at 55 SNPs having a prior association with severe malaria.
–log10 P values from combined analyses across the 12 contributing Consortial Project 1 study sites for severe malaria and the subtypes cerebral malaria and severe malarial anemia under additive, recessive, dominant and heterozygote advantage models. Results are shown for all individuals combined for (a) 0 < –log10 (P) ≤ 10 and (b) 10 < –log10 (P) < 250; results are shown in two panels for optimal viewing. The vertical dashed line indicates a P-value threshold of 1 × 10–3.
Supplementary Figure 4 Forest plots for interaction between ATP2B4 and HbC for association with severe malaria.
Odds ratios and 95% confidence intervals are shown for the interaction between ATP2B4 (rs10900585) and HbC (rs33930165) for association with severe malaria in all individuals combined across West African sites (Burkina Faso, The Gambia, Ghana, Mali, Cameroon and Nigeria). Results are adjusted for sex and ancestry. The baseline genotype is GG/GG, representing double ancestral homozygotes. OR = 1, indicating no effect, is highlighted by the gray horizontal dashed line.
Supplementary Figure 5 Genetic heterogeneity of the severe malaria subtypes cerebral malaria and severe malarial anemia within and across African populations for all loci.
Bar plots show the posterior probability on each of nine models of association where effects on the two subtypes are fixed, independent or correlated within a population combined with being fixed, independent or correlated across all the populations, as indicated by the different colors; the remainder of the posterior probability is on the null model where there is no effect on any of the subtypes. Before seeing the data, the null model is assumed to have 80% probability; the remaining 20% is divided equally among the other models. Approximate Bayes factors (ABFs), calculated as the ratio of the marginal likelihoods of a given model and the null model, are used to compare the evidence between models. (See the Online Methods for details and the specification of priors.) The dashed line at posterior probability = 20% indicates where the combined posterior probability of the non-null models is greater than their combined prior probability.
Supplementary Figure 6 Performance of sample collection across the set of 65 core SNPs (not including ATP2B4) successfully genotyped for all samples.
Samples have been ranked in order of pass rate from high to low (x axis) and plotted against their pass rate (y axis). A total of 33,138 samples were assayed, with 32,349 samples achieving a pass rate of ≥90% (98% of the sample received).
Supplementary Figure 7 Hardy-Weinberg equilibrium analysis of genotype data by SNP and country/ancestry.
A P value for Hardy-Weinberg equilibrium was calculated for each SNP and country/ancestry, discarding ancestry groups where the chromosome with the minor allele count fell below five (Forensic Sci. Int. 149, 279–286, 2005). X-chromosome SNPs used female genotypes only. At each SNP, the Hardy-Weinberg equilibrium P values calculated for each country/ancestry were transformed to unsigned log values and ranked from high to low. Each line corresponds to a single SNP and shows the transformed P values plotted as a function of their rank. The vertical dashed line at rank 5 represents the threshold for the number of ancestry groups failing the Hardy-Weinberg equilibrium test at a significance level of 1 × 10–4, a conservative threshold to allow for multiple tests (represented by the dashed horizontal line). Lines crossing into the top right of the area defined by the two dashed lines therefore represent SNPs that failed more than five tests and therefore were removed from further analysis. Using these cutoffs, the TNF c.-376G>A (rs1800750) SNP, indicated by the red line, was removed from further analysis owing to an excess of heterozygotes.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7, Supplementary Tables 1–25 and Supplementary Note. (PDF 6228 kb)
Rights and permissions
About this article
Cite this article
Malaria Genomic Epidemiology Network. Reappraisal of known malaria resistance loci in a large multicenter study. Nat Genet 46, 1197–1204 (2014). https://doi.org/10.1038/ng.3107
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ng.3107
This article is cited by
-
ApoE: A new piece to the severe malaria puzzle
Pediatric Research (2024)
-
Genetic variations in human ATP2B4 gene alter Plasmodium falciparum in vitro growth in RBCs from Gambian adults
Malaria Journal (2023)
-
ATP2B4 regulatory genetic variants are associated with mild malaria
Malaria Journal (2023)
-
Factors affecting haemoglobin dynamics in African children with acute uncomplicated Plasmodium falciparum malaria treated with single low-dose primaquine or placebo
BMC Medicine (2023)
-
Risk score prediction model based on single nucleotide polymorphism for predicting malaria: a machine learning approach
BMC Bioinformatics (2022)