Abstract
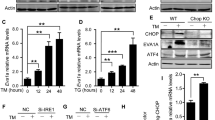
The mechanisms that regulate hematopoietic stem cell (HSC) regeneration after myelosuppressive injury are not well understood. We identified epidermal growth factor (EGF) to be highly enriched in the bone marrow serum of mice bearing deletion of Bak and Bax in TIE2-expressing cells in Tie2Cre; Bak1−/−; Baxflox/– mice. These mice showed radioprotection of the HSC pool and 100% survival after a lethal dose of total-body irradiation (TBI). Bone marrow HSCs from wild-type mice expressed functional EGF receptor (EGFR), and systemic administration of EGF promoted the recovery of the HSC pool in vivo and improved the survival of mice after TBI. Conversely, administration of erlotinib, an EGFR antagonist, decreased both HSC regeneration and the survival of mice after TBI. Mice with EGFR deficiency in VAV-expressing hematopoietic cells also had delayed recovery of bone marrow stem and progenitor cells after TBI. Mechanistically, EGF reduced radiation-induced apoptosis of HSCs and mediated this effect through repression of the proapoptotic protein PUMA. Our findings show that EGFR signaling regulates HSC regeneration after myelosuppressive injury.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Kiel, M.J., Yilmaz, O.H., Iwashita, T., Terhorst, C. & Morrison, S.J. SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell 121, 1109–1121 (2005).
Chute, J.P., Muramoto, G.G., Fung, J. & Oxford, C. Soluble factors elaborated by human brain endothelial cells induce the concomitant expansion of purified human BM CD34+CD38− cells and SCID-repopulating cells. Blood 105, 576–583 (2005).
Himburg, H.A. et al. Pleiotrophin regulates the expansion and regeneration of hematopoietic stem cells. Nat. Med. 16, 475–482 (2010).
Salter, A.B. et al. Endothelial progenitor cell infusion induces hematopoietic stem cell reconstitution in vivo. Blood 113, 2104–2107 (2009).
Butler, J.M. et al. Endothelial cells are essential for the self-renewal and repopulation of Notch-dependent hematopoietic stem cells. Cell Stem Cell 6, 251–264 (2010).
Hooper, A.T. et al. Engraftment and reconstitution of hematopoiesis is dependent on VEGFR2-mediated regeneration of sinusoidal endothelial cells. Cell Stem Cell 4, 263–274 (2009).
Montfort, M.J., Olivares, C.R., Mulcahy, J.M. & Fleming, W.H. Adult blood vessels restore host hematopoiesis following lethal irradiation. Exp. Hematol. 30, 950–956 (2002).
Ding, L., Saunders, T.L., Enikolopov, G. & Morrison, S.J. Endothelial and perivascular cells maintain haematopoietic stem cells. Nature 481, 457–462 (2012).
Chute, J.P. et al. Ex vivo culture with human brain endothelial cells increases the SCID-repopulating capacity of adult human bone marrow. Blood 100, 4433–4439 (2002).
Chute, J.P., Fung, J., Muramoto, G. & Erwin, R. Ex vivo culture rescues hematopoietic stem cells with long-term repopulating capacity following harvest from lethally irradiated mice. Exp. Hematol. 32, 308–317 (2004).
Muramoto, G.G., Chen, B., Cui, X., Chao, N.J. & Chute, J.P. Vascular endothelial cells produce soluble factors that mediate the recovery of human hematopoietic stem cells after radiation injury. Biol. Blood Marrow Transplant. 12, 530–540 (2006).
Chute, J.P. et al. Transplantation of vascular endothelial cells mediates the hematopoietic recovery and survival of lethally irradiated mice. Blood 109, 2365–2372 (2007).
Kirsch, D.G. et al. p53 controls radiation-induced gastrointestinal syndrome in mice independent of apoptosis. Science 327, 593–596 (2010).
Doan, P.L. et al. Tie2+ bone marrow endothelial cells regulate hematopoietic stem cell regeneration following radiation injury. Stem Cells published online, doi:10.1002/stem.1275 (6 November 2012).
Yoder, M.C. et al. Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood 109, 1801–1809 (2007).
Guo, S. et al. MicroRNA miR-125a controls hematopoietic stem cell number. Proc. Natl. Acad. Sci. USA 107, 14229–14234 (2010).
Boehrer, S. et al. Erlotinib exhibits antineoplastic off-target effects in AML and MDS: a preclinical study. Blood 111, 2170–2180 (2008).
Boehrer, S. et al. Erlotinib antagonizes constitutive activation of SRC family kinases and mTOR in acute myeloid leukemia. Cell Cycle 10, 3168–3175 (2011).
Sordella, R., Bell, D.W., Haber, D.A. & Settleman, J. Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science 305, 1163–1167 (2004).
Yang, W. et al. Nuclear PKM2 regulates β-catenin transactivation upon EGFR activation. Nature 480, 118–122 (2011).
Minder, P., Bayha, E., Becker-Pauly, C. & Sterchi, E.E. Meprinalpha transactivates the epidermal growth factor receptor (EGFR) via ligand shedding, thereby enhancing colorectal cancer cell proliferation and migration. J. Biol. Chem. 287, 35201–35211 (2012).
Cao, C. et al. Gα(i1) and Gα(i3) are required for epidermal growth factor–mediated activation of the Akt-mTORC1 pathway. Sci. Signal. 2, ra17 (2009).
Kriegs, M. et al. The epidermal growth factor receptor modulates DNA double-strand break repair by regulating non-homologous end-joining. DNA Repair (Amst.) 9, 889–897 (2010).
Shao, L. et al. Deletion of proapoptotic Puma selectively protects hematopoietic stem and progenitor cells against high-dose radiation. Blood 115, 4707–4714 (2010).
Yu, H. et al. Deletion of Puma protects hematopoietic stem cells and confers long-term survival in response to high-dose gamma-irradiation. Blood 115, 3472–3480 (2010).
Appelbaum, F.R. Hematopoietic-cell transplantation at 50. N. Engl. J. Med. 357, 1472–1475 (2007).
Chen, B.J. et al. Growth hormone mitigates against lethal irradiation and enhances hematologic and immune recovery in mice and nonhuman primates. PLoS ONE 5, e11056 (2010).
Waselenko, J.K. et al. Medical management of the acute radiation syndrome: recommendations of the Strategic National Stockpile Radiation Working Group. Ann. Intern. Med. 140, 1037–1051 (2004).
Liang, Y., Van Zant, G. & Szilvassy, S.J. Effects of aging on the homing and engraftment of murine hematopoietic stem and progenitor cells. Blood 106, 1479–1487 (2005).
Norddahl, G.L. et al. Accumulating mitochondrial DNA mutations drive premature hematopoietic aging phenotypes distinct from physiological stem cell aging. Cell Stem Cell 8, 499–510 (2011).
Elledge, S.J. Cell cycle checkpoints: preventing an identity crisis. Science 274, 1664–1672 (1996).
Levine, A.J. p53, the cellular gatekeeper for growth and division. Cell 88, 323–331 (1997).
Strasser, A., Harris, A.W., Jacks, T. & Cory, S. DNA damage can induce apoptosis in proliferating lymphoid cells via p53-independent mechanisms inhibitable by Bcl-2. Cell 79, 329–339 (1994).
Quelle, F.W. et al. Cytokine rescue of p53-dependent apoptosis and cell cycle arrest is mediated by distinct Jak kinase signaling pathways. Genes Dev. 12, 1099–1107 (1998).
Hérodin, F., Bourin, P., Mayol, J.F., Lataillade, J.J. & Drouet, M. Short-term injection of antiapoptotic cytokine combinations soon after lethal gamma-irradiation promotes survival. Blood 101, 2609–2616 (2003).
Zsebo, K.M. et al. Radioprotection of mice by recombinant rat stem cell factor. Proc. Natl. Acad. Sci. USA 89, 9464–9468 (1992).
Sinclair, W.K. Cyclic x-ray responses in mammalian cells in vitro. Radiat. Res. 33, 620–643 (1968).
Na Nakorn, T., Traver, D., Weissman, I.L. & Akashi, K. Myeloerythroid-restricted progenitors are sufficient to confer radioprotection and provide the majority of day 8 CFU-S. J. Clin. Invest. 109, 1579–1585 (2002).
Bill, H.M. et al. Epidermal growth factor receptor-dependent regulation of integrin-mediated signaling and cell cycle entry in epithelial cells. Mol. Cell Biol. 24, 8586–8599 (2004).
Ekert, P.G. et al. Cell death provoked by loss of interleukin-3 signaling is independent of Bad, Bim, and PI3 kinase, but depends in part on Puma. Blood 108, 1461–1468 (2006).
Jeffers, J.R. et al. Puma is an essential mediator of p53-dependent and -independent apoptotic pathways. Cancer Cell 4, 321–328 (2003).
Coloff, J.L. et al. Akt requires glucose metabolism to suppress puma expression and prevent apoptosis of leukemic T cells. J. Biol. Chem. 286, 5921–5933 (2011).
Leibowitz, B.J. et al. Uncoupling p53 functions in radiation-induced intestinal damage via PUMA and p21. Mol. Cancer Res. 9, 616–625 (2011).
Prigent, S.A. & Gullick, W.J. Identification of c-erbB-3 binding sites for phosphatidylinositol 3′-kinase and SHC using an EGF receptor/c-erbB-3 chimera. EMBO J. 13, 2831–2841 (1994).
Dittmann, K. et al. Radiation-induced epidermal growth factor receptor nuclear import is linked to activation of DNA-dependent protein kinase. J. Biol. Chem. 280, 31182–31189 (2005).
Rodemann, H.P., Dittmann, K. & Toulany, M. Radiation-induced EGFR-signaling and control of DNA-damage repair. Int. J. Radiat. Biol. 83, 781–791 (2007).
Cardó-Vila, M. et al. From combinatorial peptide selection to drug prototype (II): targeting the epidermal growth factor receptor pathway. Proc. Natl. Acad. Sci. USA 107, 5118–5123 (2010).
Ji, H. et al. The impact of human EGFR kinase domain mutations on lung tumorigenesis and in vivo sensitivity to EGFR-targeted therapies. Cancer Cell 9, 485–495 (2006).
Aguirre, A., Rubio, M.E. & Gallo, V. Notch and EGFR pathway interaction regulates neural stem cell number and self-renewal. Nature 467, 323–327 (2010).
Natarajan, A., Wagner, B. & Sibilia, M. The EGF receptor is required for efficient liver regeneration. Proc. Natl. Acad. Sci. USA 104, 17081–17086 (2007).
Shih, C.C. et al. Identification of a candidate human neurohematopoietic stem-cell population. Blood 98, 2412–2422 (2001).
Pain, B. et al. EGF-R as a hemopoietic growth factor receptor: the c-erbB product is present in chicken erythrocytic progenitors and controls their self-renewal. Cell 65, 37–46 (1991).
von Rüden, T. & Wagner, E.F. Expression of functional human EGF receptor on murine bone marrow cells. EMBO J. 7, 2749–2756 (1988).
Takahashi, T. et al. A potential molecular approach to ex vivo hematopoietic expansion with recombinant epidermal growth factor receptor–expressing adenovirus vector. Blood 91, 4509–4515 (1998).
Ryan, M.A. et al. Pharmacological inhibition of EGFR signaling enhances G-CSF–induced hematopoietic stem cell mobilization. Nat. Med. 16, 1141–1146 (2010).
Chan, G., Nogalski, M.T. & Yurochko, A.D. Activation of EGFR on monocytes is required for human cytomegalovirus entry and mediates cellular motility. Proc. Natl. Acad. Sci. USA 106, 22369–22374 (2009).
Dooley, D.C. et al. Basic fibroblast growth factor and epidermal growth factor downmodulate the growth of hematopoietic cells in long-term stromal cultures. J. Cell Physiol. 165, 386–397 (1995).
Zhang, C.C. & Lodish, H.F. Murine hematopoietic stem cells change their surface phenotype during ex vivo expansion. Blood 105, 4314–4320 (2005).
Hashimoto, M. et al. Fibroblast growth factor 1 regulates signaling via the glycogen synthase kinase-3β pathway. Implications for neuroprotection. J. Biol. Chem. 277, 32985–32991 (2002).
Shen, H. et al. An acute negative bystander effect of gamma-irradiated recipients on transplanted hematopoietic stem cells. Blood 119, 3629–3637 (2012).
Lee, T.C. & Threadgill, D.W. Generation and validation of mice carrying a conditional allele of the epidermal growth factor receptor. Genesis 47, 85–92 (2009).
Georgiades, P. et al. VavCre transgenic mice: a tool for mutagenesis in hematopoietic and endothelial lineages. Genesis 34, 251–256 (2002).
de Boer, J. et al. Transgenic mice with hematopoietic and lymphoid specific expression of Cre. Eur. J. Immunol. 33, 314–325 (2003).
Jacks, T. et al. Tumor spectrum analysis in p53-mutant mice. Curr. Biol. 4, 1–7 (1994).
Villunger, A. et al. p53- and drug-induced apoptotic responses mediated by BH3-only proteins puma and noxa. Science 302, 1036–1038 (2003).
Till, J.E. & McCulloch, E. A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat. Res. 14, 213–222 (1961).
Jordan, C.T., Yamasaki, G. & Minamoto, D. High-resolution cell cycle analysis of defined phenotypic subsets within primitive human hematopoietic cell populations. Exp. Hematol. 24, 1347–1355 (1996).
Chute, J.P. et al. Preincubation with endothelial cell monolayers increases gene transfer efficiency into human bone marrow CD34+CD38− progenitor cells. Hum. Gene Ther. 11, 2515–2528 (2000).
Bungartz, G., Land, H., Scadden, D.T. & Emerson, S.G. NF-Y is necessary for hematopoietic stem cell (HSC) proliferation and survival. Blood 119, 1380–1389 (2012).
Lehr, H.A., Mankoff, D.A., Corwin, D., Santeusanio, G. & Gown, A.M. Application of photoshop-based image analysis to quantification of hormone receptor expression in breast cancer. J. Histochem. Cytochem. 45, 1559–1565 (1997).
Lehr, H.A., van der Loos, C.M., Teeling, P. & Gown, A.M. Complete chromogen separation and analysis in double immunohistochemical stains using Photoshop-based image analysis. J. Histochem. Cytochem. 47, 119–126 (1999).
Acknowledgements
This work was supported in part by National Heart, Lung and Blood Institute grant HL-086998-01 (J.P.C.), National Institute of Allergy and Infectious Diseases (NIAID) grant AI-067798-06 (J.P.C.) and a pilot project from the NIAID Centers for Medical Countermeasures grant AI-067798-01 (D.G.K.). P.L.D. was supported by US National Institutes of Health training grant T32 HL0070757-33, the Barton Haynes Award and a Duke Cancer Center Seed Grant (Duke University).
Author information
Authors and Affiliations
Contributions
P.L.D. performed experiments, analyzed data and wrote the paper. H.A.H., K.H. and J.L.R. performed experiments and analyzed data. E.F., M.Q., J.R.H. and D.D. performed experiments. J.M.S. provided reagents. N.J.C. analyzed data and wrote the paper. D.G.K. designed experiments, analyzed data and wrote the paper. J.P.C. conceived of the study, designed experiments, analyzed the data and wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–3 (PDF 225 kb)
Rights and permissions
About this article
Cite this article
Doan, P., Himburg, H., Helms, K. et al. Epidermal growth factor regulates hematopoietic regeneration after radiation injury. Nat Med 19, 295–304 (2013). https://doi.org/10.1038/nm.3070
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/nm.3070
This article is cited by
-
Adipose-derived mesenchymal stem cells cultured in serum-free medium attenuate acute contrast-induced nephropathy by exerting anti-apoptotic effects
Stem Cell Research & Therapy (2023)
-
Impact of aging on gene expression response to x-ray irradiation using mouse blood
Scientific Reports (2021)
-
Neuropilin 1 regulates bone marrow vascular regeneration and hematopoietic reconstitution
Nature Communications (2021)
-
Vascular Regulation of Hematopoietic Stem Cell Homeostasis, Regeneration, and Aging
Current Stem Cell Reports (2021)
-
Dental Pulp Stem Cell-Derived Extracellular Vesicles Mitigate Haematopoietic Damage after Radiation
Stem Cell Reviews and Reports (2021)