Abstract
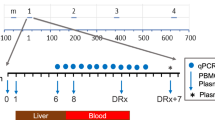
Malaria, caused by the protozoan Plasmodium, is a devastating mosquito-borne disease with the potential to affect nearly half the world's population1. Despite mounting substantial T and B cell responses, humans fail to efficiently control blood-stage malaria or develop sterilizing immunity to reinfections2. Although forkhead box P3 (FOXP3)+CD4+ regulatory T (Treg) cells form a part of these responses3,4,5, their influence remains disputed and their mode of action is unknown. Here we show that Treg cells expand in both humans and mice in blood-stage malaria and interfere with conventional T helper cell responses and follicular T helper (TFH)–B cell interactions in germinal centers. Mechanistically, Treg cells function in a critical temporal window to impede protective immunity through cytotoxic-T-lymphocyte-associated protein-4 (CTLA-4). Targeting Treg cells or CTLA-4 in this precise window accelerated parasite clearance and generated species-transcending immunity to blood-stage malaria in mice. Our study uncovers a critical mechanism of immunosuppression associated with blood-stage malaria that delays parasite clearance and prevents development of potent adaptive immunity to reinfection. These data also reveal a temporally discrete and potentially therapeutically amenable functional role for Treg cells and CTLA-4 in limiting antimalarial immunity.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
World Health Organization. World Malaria Report 2014 (World Health Organization, 2014).
Tran, T.M. et al. An intensive longitudinal cohort study of Malian children and adults reveals no evidence of acquired immunity to Plasmodium falciparum infection. Clin. Infect. Dis. 57, 40–47 (2013).
Ho, M. et al. Antigen-specific immunosuppression in human malaria due to Plasmodium falciparum. J. Infect. Dis. 153, 763–771 (1986).
Crompton, P.D. et al. Malaria immunity in man and mosquito: insights into unsolved mysteries of a deadly infectious disease. Annu. Rev. Immunol. 32, 157–187 (2014).
Van Braeckel-Budimir, N., Kurup, S.P. & Harty, J.T. Regulatory issues in immunity to liver and blood-stage malaria. Curr. Opin. Immunol. 42, 91–97 (2016).
Perez-Mazliah, D. & Langhorne, J. CD4 T-cell subsets in malaria: TH1/TH2 revisited. Front. Immunol. 5, 671 (2015).
Butler, N.S. et al. Therapeutic blockade of PD-L1 and LAG-3 rapidly clears established blood-stage Plasmodium infection. Nat. Immunol. 13, 188–195 (2011).
Finney, O.C., Riley, E.M. & Walther, M. Regulatory T cells in malaria—friend or foe? Trends Immunol. 31, 63–70 (2010).
Hansen, D.S. & Schofield, L. Natural regulatory T cells in malaria: host or parasite allies? PLoS Pathog. 6, e1000771 (2010).
Hisaeda, H. et al. Escape of malaria parasites from host immunity requires CD4+CD25+ regulatory T cells. Nat. Med. 10, 29–30 (2004).
Amante, F.H. et al. A role for natural regulatory T cells in the pathogenesis of experimental cerebral malaria. Am. J. Pathol. 171, 548–559 (2007).
Randall, L.M. et al. Common strategies to prevent and modulate experimental cerebral malaria in mouse strains with different susceptibilities. Infect. Immun. 76, 3312–3320 (2008).
Nie, C.Q. et al. CD4+CD25+ regulatory T cells suppress CD4+ T-cell function and inhibit the development of Plasmodium berghei–specific TH1 responses involved in cerebral malaria pathogenesis. Infect. Immun. 75, 2275–2282 (2007).
Cambos, M., Bélanger, B., Jacques, A., Roulet, A. & Scorza, T. Natural regulatory (CD4+CD25+FOXP+) T cells control the production of pro-inflammatory cytokines during Plasmodium chabaudi adami infection and do not contribute to immune evasion. Int. J. Parasitol. 38, 229–238 (2008).
Couper, K.N. et al. IL-10 from CD4+CD25−Foxp3−CD127− adaptive regulatory T cells modulates parasite clearance and pathology during malaria infection. PLoS Pathog. 4, e1000004 (2008).
Abel, S. et al. Strong impact of CD4+Foxp3+ regulatory T cells and limited effect of T cell–derived IL-10 on pathogen clearance during Plasmodium yoelii infection. J. Immunol. 188, 5467–5477 (2012).
Haque, A. et al. CD4+ natural regulatory T cells prevent experimental cerebral malaria via CTLA-4 when expanded in vivo. PLoS Pathog. 6, e1001221 (2010).
Linterman, M.A. et al. Foxp3+ follicular regulatory T cells control the germinal center response. Nat. Med. 17, 975–982 (2011).
Aloulou, M. et al. Follicular regulatory T cells can be specific for the immunizing antigen and derive from naive T cells. Nat. Commun. 7, 10579 (2016).
Setiady, Y.Y., Coccia, J.A. & Park, P.U. In vivo depletion of CD4+FOXP3+ Treg cells by the PC61 anti-CD25 monoclonal antibody is mediated by FcγRIII+ phagocytes. Eur. J. Immunol. 40, 780–786 (2010).
Penaloza-MacMaster, P. et al. Interplay between regulatory T cells and PD-1 in modulating T cell exhaustion and viral control during chronic LCMV infection. J. Exp. Med. 211, 1905–1918 (2014).
Boyman, O. & Sprent, J. The role of interleukin-2 during homeostasis and activation of the immune system. Nat. Rev. Immunol. 12, 180–190 (2012).
Schmidt, A., Oberle, N. & Krammer, P.H. Molecular mechanisms of Treg-mediated T cell suppression. Front. Immunol. 3, 51 (2012).
Sebastian, M. et al. Helios controls a limited subset of regulatory T cell functions. J. Immunol. 196, 144–155 (2016).
Kim, H.J. et al. Stable inhibitory activity of regulatory T cells requires the transcription factor Helios. Science 350, 334–339 (2015).
Wei, Y., Feng, J., Hou, Z., Wang, X.M. & Yu, D. Flow cytometric analysis of circulating follicular helper T (TFH) and follicular regulatory T (TFR) populations in human blood. Methods Mol. Biol. 1291, 199–207 (2015).
Maceiras, A.R. & Graca, L. Identification of Foxp3+ T follicular regulatory (TFR) cells by flow cytometry. Methods Mol. Biol. 1291, 143–150 (2015).
Boyle, M.J. et al. Human antibodies fix complement to inhibit Plasmodiumfalciparum invasion of erythrocytes and are associated with protection against malaria. Immunity 42, 580–590 (2015).
Cohen, S., McGREGOR, I.A. & Carrington, S. γ-globulin and acquired immunity to human malaria. Nature 192, 733–737 (1961).
Sage, P.T. et al. The coinhibitory receptor CTLA-4 controls B cell responses by modulating T follicular helper, T follicular regulatory, and T regulatory cells. Immunity 41, 1026–1039 (2014).
Yadav, M., Stephan, S. & Bluestone, J.A. Peripherally induced Tregs—role in immune homeostasis and autoimmunity. Front. Immunol. 4, 232 (2013).
Walker, L.S. & Sansom, D.M. The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nat. Rev. Immunol. 11, 852–863 (2011).
Yusuf, I. et al. Germinal center B cell depletion diminishes CD4+ follicular T helper cells in autoimmune mice. PLoS One 9, e102791 (2014).
Hannani, D. et al. Anticancer immunotherapy by CTLA-4 blockade: obligatory contribution of IL-2 receptors and negative prognostic impact of soluble CD25. Cell Res. 25, 208–224 (2015).
Ahlborg, N., Ling, I.T., Howard, W., Holder, A.A. & Riley, E.M. Protective immune responses to the 42-kilodalton (kDa) region of Plasmodium yoelii merozoite surface protein 1 are induced by the C-terminal 19-kDa region but not by the adjacent 33-kDa region. Infect. Immun. 70, 820–825 (2002).
Hafalla, J.C. et al. The CTLA-4 and PD-1/PD-L1 inhibitory pathways independently regulate host resistance to Plasmodium-induced acute immune pathology. PLoS Pathog. 8, e1002504 (2012).
Zander, R.A. et al. PD-1 co-inhibitory and OX40 co-stimulatory crosstalk regulates helper T cell differentiation and anti-Plasmodium humoral immunity. Cell Host Microbe 17, 628–641 (2015).
McKenzie, F.E. & Bossert, W.H. Multispecies Plasmodium infections of humans. J. Parasitol. 85, 12–18 (1999).
Topalian, S.L., Drake, C.G. & Pardoll, D.M. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 27, 450–461 (2015).
Korman, A.J., Peggs, K.S. & Allison, J.P. Checkpoint blockade in cancer immunotherapy. Adv. Immunol. 90, 297–339 (2006).
Wang, Y. et al. Th2 lymphoproliferative disorder of LatY136F mutant mice unfolds independently of TCR–MHC engagement and is insensitive to the action of Foxp3+ regulatory T cells. J. Immunol. 180, 1565–1575 (2008).
Liu, X. et al. Bcl6 expression specifies the T follicular helper cell program in vivo. J. Exp. Med. 209, 1841–1852 (2012).
Brundage, R.A. et al. Expression and phosphorylation of the Listeria monocytogenes ActA protein in mammalian cells. Proc. Natl. Acad. Sci. USA 90, 11890–11894 (1993).
Obeng-Adjei, N. et al. Circulating Th1-cell-type Tfh cells that exhibit impaired B cell help are preferentially activated during acute malaria in children. Cell Rep. 13, 425–439 (2015).
Villarino, N.F. et al. Composition of the gut microbiota modulates the severity of malaria. Proc. Natl. Acad. Sci. USA 113, 2235–2240 (2016).
Kim, M.T., Kurup, S.P., Starbeck-Miller, G.R. & Harty, J.T. Manipulating memory CD8 T cell numbers by timed enhancement of IL-2 signals. J. Immunol. 197, 1754–1761 (2016).
Qureshi, O.S. et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science 332, 600–603 (2011).
Fulton, R.B., Meyerholz, D.K. & Varga, S.M. Foxp3+ CD4 regulatory T cells limit pulmonary immunopathology by modulating the CD8 T cell response during respiratory syncytial virus infection. J. Immunol. 185, 2382–2392 (2010).
Acknowledgements
We thank L. Epping and S. Hartwig for assistance; S. Varga (University of Iowa, PC61.5 antibody), T. Waldschmidt (University of Iowa, MR-1 antibody), and D.A.A. Vignali (University of Pittsburgh, hybridoma clone C9B7W) for reagents; S. Perlman and V. Badovinac for constructive comments; the University of Iowa Central Microscopy Research Facility; and the New York University Insectary Core Facility. Support for these studies was provided by grants from the National Institute of Allergy and Infectious Disease of the National Institutes of Health (NIAID/NIH) (AI42767, AI85515, AI95178, and AI100527 to J.T.H.). Support for the laboratory of N.S.B. was provided by grants from NIAID/NIH (AI125446 and AI127481) and the National Institute of General Medical Science of the NIH (GM103447). The Malian study and the analysis of human samples were funded by the Division of Intramural Research, NIAID/NIH.
Author information
Authors and Affiliations
Contributions
S.P.K., N.O.-A., S.M.A., and N.S.B. designed, performed, analyzed, and interpreted experiments. S.P.K., N.S.B., P.D.C., and J.T.H. wrote the paper. B.T., O.K.D., and P.D.C. supervised the human studies and designed, analyzed, and interpreted experiments. J.T.H. supervised the project and designed and interpreted experiments.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Figures and Table
Supplementary Figures 1–14 and Supplementary Table 1 (PDF 2025 kb)
Rights and permissions
About this article
Cite this article
Kurup, S., Obeng-Adjei, N., Anthony, S. et al. Regulatory T cells impede acute and long-term immunity to blood-stage malaria through CTLA-4. Nat Med 23, 1220–1225 (2017). https://doi.org/10.1038/nm.4395
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/nm.4395
This article is cited by
-
Immunomodulatory effects of Eimeria maxima surface antigen (EmSAG) as an IFN-γ inhibitory molecule on peripheral blood mononuclear cells (PBMCs) and T cell subsets in chickens
Veterinary Research (2025)
-
High PD-1 and CTLA-4 expression correlates with host immune suppression in patients and a mouse model infected with Echinococcus multilocularis
Parasites & Vectors (2024)
-
Gene expression analyses reveal differences in children’s response to malaria according to their age
Nature Communications (2024)
-
The impact of Plasmodium-driven immunoregulatory networks on immunity to malaria
Nature Reviews Immunology (2024)
-
Gut Bacteroides act in a microbial consortium to cause susceptibility to severe malaria
Nature Communications (2023)