Abstract
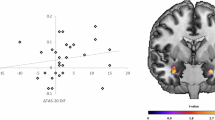
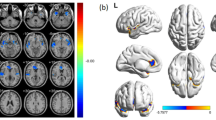
Serotonin reuptake inhibitors and cognitive-behavior therapy (CBT) are considered first-line treatments for obsessive-compulsive disorder (OCD). However, little is known about their modulatory effects on regional brain morphology in OCD patients. We sought to document structural brain abnormalities in treatment-naive OCD patients and to determine the effects of pharmacological and cognitive-behavioral treatments on regional brain volumes. Treatment-naive patients with OCD (n=38) underwent structural magnetic resonance imaging scan before and after a 12-week randomized clinical trial with either fluoxetine or group CBT. Matched-healthy controls (n=36) were also scanned at baseline. Voxel-based morphometry was used to compare regional gray matter (GM) volumes of regions of interest (ROIs) placed in the orbitofrontal, anterior cingulate and temporolimbic cortices, striatum, and thalamus. Treatment-naive OCD patients presented smaller GM volume in the left putamen, bilateral medial orbitofrontal, and left anterior cingulate cortices than did controls (p<0.05, corrected for multiple comparisons). After treatment with either fluoxetine or CBT (n=26), GM volume abnormalities in the left putamen were no longer detectable relative to controls. ROI-based within-group comparisons revealed that GM volume in the left putamen significantly increased (p<0.012) in fluoxetine-treated patients (n=13), whereas no significant GM volume changes were observed in CBT-treated patients (n=13). This study supports the involvement of orbitofronto/cingulo-striatal loops in the pathophysiology of OCD and suggests that fluoxetine and CBT may have distinct neurobiological mechanisms of action.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ashburner J, Friston KJ (2005). Unified segmentation. Neuroimage 26: 839–851.
Atmaca M, Yildirim H, Ozdemir H, Ozler S, Kara B, Ozler Z et al (2008). Hippocampus and amygdalar volumes in patients with refractory obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 32: 1283–1286.
Baxter Jr LR, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC et al (1992). Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry 49: 681–689.
Beck AT, Epstein N, Brown G, Steer RA (1988). An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56: 893–897.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961). An inventory for measuring depression. Arch Gen Psychiatry 4: 561–571.
Belotto-Silva C, Diniz JB, Malavazzia DM, Valério C, Fossaluza V, Sonia Borcato S et al (2011). Group cognitive-behavioral therapy versus selective serotonin reuptake inhibitors for obsessive-compulsive disorder: a practical clinical trial. J Anxiety Disord (in press).
Benazon NR, Moore GJ, Rosenberg DR (2003). Neurochemical analyses in pediatric obsessive-compulsive disorder in patients treated with cognitive-behavioral therapy. J Am Acad Child Adolesc Psychiatry 42: 1279–1285.
Benkelfat C, Nordahl TE, Semple WE, King AC, Murphy DL, Cohen RM (1990). Local cerebral glucose metabolic rates in obsessive-compulsive disorder. Patients treated with clomipramine. Arch Gen Psychiatry 47: 840–848.
Blier P, Bouchard C (1994). Modulation of 5-HT release in the guinea-pig brain following long-term administration of antidepressant drugs. Br J Pharmacol 113: 485–495.
Bloom FE, Kupfer DJ (1995). Psychopharmacology: The Fourth Generation of Progress. Raven Press: New York. 2002p.pp.
Brett M, Johnsrude IS, Owen AM (2002). The problem of functional localization in the human brain. Nat Rev Neurosci 3: 243–249.
Burgos-Robles A, Vidal-Gonzalez I, Santini E, Quirk GJ (2007). Consolidation of fear extinction requires NMDA receptor-dependent bursting in the ventromedial prefrontal cortex. Neuron 53: 871–880.
Busatto GF, Zamignani DR, Buchpiguel CA, Garrido GE, Glabus MF, Rocha ET et al (2000). A voxel-based investigation of regional cerebral blood flow abnormalities in obsessive-compulsive disorder using single photon emission computed tomography (SPECT). Psychiatry Res 99: 15–27.
Cardinal RN, Parkinson JA, Hall J, Everitt BJ (2002). Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neurosci Biobehav Rev 26: 321–352.
Cardoner N, Soriano-Mas C, Pujol J, Alonso P, Harrison BJ, Deus J et al (2007). Brain structural correlates of depressive comorbidity in obsessive-compulsive disorder. Neuroimage 38: 413–421.
Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ (2005). The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev 29: 399–419.
Chamberlain SR, Menzies L, Hampshire A, Suckling J, Fineberg NA, del Campo N et al (2008). Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science 321: 421–422.
Cordioli A, Heldt E, Bochi D, Margis M, de Sousa M, Tonello J et al (2002). Cognitive-behavioral group therapy in the treatment of obsessive-compulsive disorder: an open clinical trial. Revista Brasileira de Psiquiatria 24: 113–120.
Cuadra MB, Cammoun L, Butz T, Cuisenaire O, Thiran JP (2005). Comparison and validation of tissue modelization and statistical classification methods in T1-weighted MR brain images. IEEE Trans Med Imaging 24: 1548–1565.
Czeh B, Muller-Keuker JI, Rygula R, Abumaria N, Hiemke C, Domenici E et al (2007). Chronic social stress inhibits cell proliferation in the adult medial prefrontal cortex: hemispheric asymmetry and reversal by fluoxetine treatment. Neuropsychopharmacology 32: 1490–1503.
Davis M, Myers KM (2002). The role of glutamate and gamma-aminobutyric acid in fear extinction: clinical implications for exposure therapy. Biol Psychiatry 52: 998–1007.
Derryberry D, Tucker DM (1992). Neural mechanisms of emotion. J Consult Clin Psychol 60: 329–338.
Diniz JB, Shavitt RG, Pereira CA, Hounie AG, Pimentel I, Koran LM et al (2010). Quetiapine versus clomipramine in the augmentation of selective serotonin reuptake inhibitors for the treatment of obsessive-compulsive disorder: a randomized, open-label trial. J Psychopharmacol 24: 297–307.
Eddy KT, Dutra L, Bradley R, Westen D (2004). A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clin Psychol Rev 24: 1011–1030.
el Mansari M, Bouchard C, Blier P (1995). Alteration of serotonin release in the guinea pig orbito-frontal cortex by selective serotonin reuptake inhibitors. Relevance to treatment of obsessive-compulsive disorder. Neuropsychopharmacology 13: 117–127.
Ferreira LK, Busatto GF (2010). Heterogeneity of coordinate-based meta-analyses of neuroimaging data: an example from studies in OCD. Br J Psychiatry 197: 76–77; author reply 77.
Fossaluza V, Diniz JB, Pereira Bde B, Miguel EC, Pereira CA (2009). Sequential allocation to balance prognostic factors in a psychiatric clinical trial. Clinics (Sao Paulo) 64: 511–518.
Friston K, Holmes A, Worsley K, Poline J, Frith C, Frackowiak R (1994). Statistic parametric maps in functional imaging: a general linear approach. Hum Brain Mapp 2: 189–210.
Gilbert AR, Moore GJ, Keshavan MS, Paulson LA, Narula V, Mac Master FP et al (2000). Decrease in thalamic volumes of pediatric patients with obsessive-compulsive disorder who are taking paroxetine. Arch Gen Psychiatry 57: 449–456.
Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S et al (2004). Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry 61: 34–41.
Good CD, Johnsrude IS, Ashburner J, Henson RN, Friston KJ, Frackowiak RS (2001). A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage 14 (1 Pt 1): 21–36.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 46: 1006–1011.
Greenberg BD, Rauch SL, Haber SN (2010). Invasive circuitry-based neurotherapeutics: stereotactic ablation and deep brain stimulation for OCD. Neuropsychopharmacology 35: 317–336.
Greist JH, Jefferson JW, Kobak KA, Katzelnick DJ, Serlin RC (1995). Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder. A meta-analysis. Arch Gen Psychiatry 52: 53–60.
Guy W (1976). Clinical Global Impression (CGI). In: ECDEU Assessment Manual for Psychopharmacology, Revised edn. US Department of Health, Education, and Welfare: Rockville, MD, USA [S.l].
Haber SN (2003). The primate basal ganglia: parallel and integrative networks. J Chem Neuroanat 26: 317–330.
Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, Lopez-Sola M, Hernandez-Ribas R et al (2009). Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch Gen Psychiatry 66: 1189–1200.
Hoexter MQ, Shavitt RG, D’Alcante CC, Cecconi JP, Diniz JB, Belotto-Silva C et al (2009). The drug-naive OCD patients imaging genetics, cognitive and treatment response study: methods and sample description. Rev Bras Psiquiatr 31: 349–353.
Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T et al (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res 191: 36–43.
Insel TR (1992). Toward a neuroanatomy of obsessive-compulsive disorder. Arch Gen Psychiatry 49: 739–744.
Kodama M, Fujioka T, Duman RS (2004). Chronic olanzapine or fluoxetine administration increases cell proliferation in hippocampus and prefrontal cortex of adult rat. Biol Psychiatry 56: 570–580.
Lacerda AL, Dalgalarrondo P, Caetano D, Camargo EE, Etchebehere EC, Soares JC (2003). Elevated thalamic and prefrontal regional cerebral blood flow in obsessive-compulsive disorder: a SPECT study. Psychiatry Res 123: 125–134.
Lazaro L, Bargallo N, Castro-Fornieles J, Falcon C, Andres S, Calvo R et al (2009). Brain changes in children and adolescents with obsessive-compulsive disorder before and after treatment: a voxel-based morphometric MRI study. Psychiatry Res 172: 140–146.
Lyoo IK, Dager SR, Kim JE, Yoon SJ, Friedman SD, Dunner DL et al (2010). Lithium-induced gray matter volume increase as a neural correlate of treatment response in bipolar disorder: a longitudinal brain imaging study. Neuropsychopharmacology 35: 1743–1750.
MacMaster FP, O’Neill J, Rosenberg DR (2008). Brain imaging in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 47: 1262–1272.
Mazziotta JC, Toga AW, Evans A, Fox P, Lancaster J (1995). A probabilistic atlas of the human brain: theory and rationale for its development. The International Consortium for Brain Mapping (ICBM). Neuroimage 2: 89–101.
First MB, Spitzer RL, Gibbon M, Williams JB (1997). Structured Clinical Interview for DSM-IV Axis I Disorders: Clinical Version (SCID CV). American Psychiatric Press: Washington, DC.
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET (2008). Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev 32: 525–549.
Miguel EC, Ferrao YA, Rosario MC, Mathis MA, Torres AR, Fontenelle LF et al (2008). The Brazilian research consortium on obsessive-compulsive spectrum disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr 30: 185–196.
Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL (2005). Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA 102: 10706–10711.
Milad MR, Wright CI, Orr SP, Pitman RK, Quirk GJ, Rauch SL (2007). Recall of fear extinction in humans activates the ventromedial prefrontal cortex and hippocampus in concert. Biol Psychiatry 62: 446–454.
Perani D, Colombo C, Bressi S, Bonfanti A, Grassi F, Scarone S et al (1995). [18F]FDG PET study in obsessive-compulsive disorder. A clinical/metabolic correlation study after treatment. Br J Psychiatry 166: 244–250.
Phelps EA, Delgado MR, Nearing KI, LeDoux JE (2004). Extinction learning in humans: role of the amygdala and vmPFC. Neuron 43: 897–905.
Phillips ML, Drevets WC, Rauch SL, Lane R (2003). Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biol Psychiatry 54: 504–514.
Pujol J, Soriano-Mas C, Alonso P, Cardoner N, Menchon JM, Deus J et al (2004). Mapping structural brain alterations in obsessive-compulsive disorder. Arch Gen Psychiatry 61: 720–730.
Radua J, Mataix-Cols D (2009). Voxel-wise meta-analysis of grey matter changes in obsessive-compulsive disorder. Br J Psychiatry 195: 393–402.
Radua J, van den Heuvel OA, Surguladze S, Mataix-Cols D (2010). Meta-analytical comparison of voxel-based morphometry studies in obsessive-compulsive disorder vs other anxiety disorders. Arch Gen Psychiatry 67: 701–711.
Rauch SL (2000). Neuroimaging research and the neurobiology of obsessive-compulsive disorder: where do we go from here? Biol Psychiatry 47: 168–170.
Rauch SL, Jenike MA, Alpert NM, Baer L, Breiter HC, Savage CR et al (1994). Regional cerebral blood flow measured during symptom provocation in obsessive-compulsive disorder using oxygen 15-labeled carbon dioxide and positron emission tomography. Arch Gen Psychiatry 51: 62–70.
Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D et al (2006). The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry 11: 495–504.
Rosenberg DR, Benazon NR, Gilbert A, Sullivan A, Moore GJ (2000). Thalamic volume in pediatric obsessive-compulsive disorder patients before and after cognitive behavioral therapy. Biol Psychiatry 48: 294–300.
Rotge JY, Langbour N, Guehl D, Bioulac B, Jaafari N, Allard M et al (2010). Gray matter alterations in obsessive-compulsive disorder: an anatomic likelihood estimation meta-analysis. Neuropsychopharmacology 35: 686–691.
Saxena S, Brody AL, Ho ML, Alborzian S, Ho MK, Maidment KM et al (2001). Cerebral metabolism in major depression and obsessive-compulsive disorder occurring separately and concurrently. Biol Psychiatry 50: 159–170.
Saxena S, Brody AL, Ho ML, Alborzian S, Maidment KM, Zohrabi N et al (2002). Differential cerebral metabolic changes with paroxetine treatment of obsessive-compulsive disorder vs major depression. Arch Gen Psychiatry 59: 250–261.
Saxena S, Gorbis E, O’Neill J, Baker SK, Mandelkern MA, Maidment KM et al (2009). Rapid effects of brief intensive cognitive-behavioral therapy on brain glucose metabolism in obsessive-compulsive disorder. Mol Psychiatry 14: 197–205.
Saxena S, Rauch SL (2000). Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am 23: 563–586.
Schwartz JM, Stoessel PW, Baxter Jr LR, Martin KM, Phelps ME (1996). Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorder. Arch Gen Psychiatry 53: 109–113.
Sotres-Bayon F, Cain CK, LeDoux JE (2006). Brain mechanisms of fear extinction: historical perspectives on the contribution of prefrontal cortex. Biol Psychiatry 60: 329–336.
Soumier A, Banasr M, Goff LK, Daszuta A (2009). Region- and phase-dependent effects of 5-HT(1A) and 5-HT(2C) receptor activation on adult neurogenesis. Eur Neuropsychopharmacol 20: 336–345.
Sousa MB, Isolan LR, Oliveira RR, Manfro GG, Cordioli AV (2006). A randomized clinical trial of cognitive-behavioral group therapy and sertraline in the treatment of obsessive-compulsive disorder. J Clin Psychiatry 67: 1133–1139.
Swedo SE, Pietrini P, Leonard HL, Schapiro MB, Rettew DC, Goldberger EL et al (1992). Cerebral glucose metabolism in childhood-onset obsessive-compulsive disorder. Revisualization during pharmacotherapy. Arch Gen Psychiatry 49: 690–694.
Szeszko PR, Christian C, Macmaster F, Lencz T, Mirza Y, Taormina SP et al (2008). Gray matter structural alterations in psychotropic drug-naive pediatric obsessive-compulsive disorder: an optimized voxel-based morphometry study. Am J Psychiatry 165: 1299–1307.
Szeszko PR, MacMillan S, McMeniman M, Lorch E, Madden R, Ivey J et al (2004). Amygdala volume reductions in pediatric patients with obsessive-compulsive disorder treated with paroxetine: preliminary findings. Neuropsychopharmacology 29: 826–832.
Szeszko PR, Robinson D, Alvir JM, Bilder RM, Lencz T, Ashtari M et al (1999). Orbital frontal and amygdala volume reductions in obsessive-compulsive disorder. Arch Gen Psychiatry 56: 913–919.
Talairach J, Tornoux P (1988). Co-planar Stereotaxic Atlas of the Human Brain. New York: Thieme Medical Publishers.
Tucker DM, Luu P, Pribram KH (1995). Social and emotional self-regulation. Ann NY Acad Sci 769: 213–239.
Valente Jr AA, Miguel EC, Castro CC, Amaro Jr E, Duran FL, Buchpiguel CA et al (2005). Regional gray matter abnormalities in obsessive-compulsive disorder: a voxel-based morphometry study. Biol Psychiatry 58: 479–487.
van den Heuvel OA, Remijnse PL, Mataix-Cols D, Vrenken H, Groenewegen HJ, Uylings HB et al (2009). The major symptom dimensions of obsessive-compulsive disorder are mediated by partially distinct neural systems. Brain 132 (Pt 4): 853–868.
Vikas A, Avasthi A, Sharan P (2009). Psychological impact of obsessive compulsive disorder on patients and their caregivers: a comparative study with depressive disorder. Int J Soc Psychiatry 57: 45–56.
Volpato Cordioli A, Heldt E, Braga Bochi D, Margis R, Basso de Sousa M, Fonseca Tonello J et al (2003). Cognitive-behavioral group therapy in obsessive-compulsive disorder: a randomized clinical trial. Psychother Psychosom 72: 211–216.
Acknowledgements
We thank Dr Cristina Belotto-Silva, Ms Sonia Borcatto, Dr Ana Gabriela Hounie, Ms Marines Alves Joaquim, Ms Ana Carolina Ferreira Rosa, and Ms Luciana Cristina Santos whose help was critical to the conduction of this project. We also thank Ms Dianne M Hezel for helpful comments on the manuscript. This study received financial support in the form of grants provided by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, Foundation for the Support of Research in the State of São Paulo) to Dr Miguel (2005/55628-8) and from FAPESP scholarships to Dr Shavitt (06/61459-7), to Dr Diniz (06/50273-0), to Dr Lopes (2008/10257-0), and to Ms D’Alcante (06/58286-3). Dr Hoexter is supported by a PhD scholarship from FAPESP (2005/04206-6) and by a doctorate ‘sandwich’ scholarship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Agency for Support and Evaluation of Graduate Education) (4375/08-4). This work was presented in part at the 48th Annual Meeting of the American College of Neuropsychopharmacology, 6–10 December 2009, Hollywood, Florida, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Hoexter, Dr Duran, Ms D’Alcante, Dr Shavitt, Dr Lopes, Dr Diniz, Mr Batistuzzo, and Dr Busatto have declared no conflict of interest. Dr Dougherty has acted as a consultant for Medtronic, Eli Lilly, Brand Ideas, McNeil, and Reed Elsevier, and has received research funding from Medtronic, Eli Lilly, McNeil, and Cyberonics. Dr Deckersbach's research has been funded by NIMH, NARSAD, TSA, OCF, and Tufts University. He has received honoraria, consultation fees, and/or royalties from the MGH Psychiatry Academy, BrainCells, Systems Research and Applications Corporation, Boston University, the Catalan Agency for Health Technology Assessment and Research, the National Association of Social Workers Massachusetts, the Massachusetts Medical Society, Tufts University, NIDA, German Research Foundation/Federal Ministry for Education and Research, and Oxford University Press. He has also participated in research funded by NIH, NIA, AHRQ, Janssen Pharmaceuticals, The Forest Research Institute, Shire Development, Medtronic, Cyberonics, and Northstar. Dr Bressan has received honoraria and/or consultations fees from Novartis, Eli Lilly, Janssen, and AstraZeneca. Dr Miguel has received lecture fees from Lundbeck and Solvay.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hoexter, M., de Souza Duran, F., D'Alcante, C. et al. Gray Matter Volumes in Obsessive-Compulsive Disorder Before and After Fluoxetine or Cognitive-Behavior Therapy: A Randomized Clinical Trial. Neuropsychopharmacol 37, 734–745 (2012). https://doi.org/10.1038/npp.2011.250
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2011.250
Keywords
This article is cited by
-
Volumetric MRI Findings in Mild Traumatic Brain Injury (mTBI) and Neuropsychological Outcome
Neuropsychology Review (2023)
-
Brief internet-delivered cognitive-behavioural intervention for children and adolescents with symptoms of anxiety and depression during the COVID-19 pandemic: a randomised controlled trial protocol
Trials (2022)
-
Structural neuroimaging biomarkers for obsessive-compulsive disorder in the ENIGMA-OCD consortium: medication matters
Translational Psychiatry (2020)
-
Layer-specific reduced neuronal density in the orbitofrontal cortex of older adults with obsessive–compulsive disorder
Brain Structure and Function (2019)
-
Cortical Thickness and Subcortical Gray Matter Volume in Pediatric Anxiety Disorders
Neuropsychopharmacology (2017)