Abstract
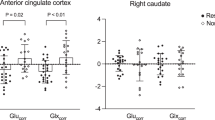
Many patients with schizophrenia show a limited symptomatic response to treatment with dopaminergic antipsychotics. This may reflect the additional involvement of non-dopaminergic neurochemical dysfunction in the pathophysiology of the disorder. We tested the hypothesis that brain glutamate levels would differ between patients with first-episode psychosis who were symptomatic compared with those with minimal symptoms following antipsychotic treatment. Proton magnetic resonance spectroscopy (1H-MRS) spectra were acquired at 3 Tesla in the anterior cingulate cortex and left thalamus in 15 patients with first-episode psychosis in symptomatic remission, and 17 patients with first-episode psychosis who were still symptomatic following at least one course of antipsychotic treatment. Metabolite levels were estimated in ratio to creatine (Cr) using LCModel. Levels of glutamate/Cr in the anterior cingulate cortex were significantly higher in patients who were still symptomatic than in those in remission (T(30)=3.02; P=0.005). Across the entire sample, higher levels of glutamate/Cr in the anterior cingulate cortex were associated with a greater severity of negative symptoms (r=0.42; P=0.017) and a lower level of global functioning (r=−0.47; P=0.007). These findings suggest that clinical status following antipsychotic treatment in schizophrenia is linked to glutamate dysfunction. Treatment with compounds acting on the glutamatergic system might therefore be beneficial in patients who respond poorly to dopaminergic antipsychotics.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Andreasen NC, Carpenter Jr WT, Kane JM, Lasser RA, Marder SR, Weinberger DR (2005). Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 162: 441–449.
Aoyama N, Theberge J, Drost DJ, Manchanda R, Northcott S, Neufeld RW et al. (2011). Grey matter and social functioning correlates of glutamatergic metabolite loss in schizophrenia. Br J Psychiatry 198: 448–456.
Borgwardt SJ, McGuire PK, Aston J, Berger G, Dazzan P, Gschwandtner U et al. (2007). Structural brain abnormalities in individuals with an at-risk mental state who later develop psychosis. Br J Psychiatry Suppl 51: s69–s75.
Bustillo JR, Chen H, Gasparovic C, Mullins P, Caprihan A, Qualls C et al. (2011). Glutamate as a marker of cognitive function in schizophrenia: a proton spectroscopic imaging study at 4 Tesla. Biol Psychiatry 69: 19–27.
Bustillo JR, Rowland LM, Mullins P, Jung R, Chen H, Qualls C et al. (2010). (1)H-MRS at 4 Tesla in minimally treated early schizophrenia. Mol Psychiatry 15: 629–636.
Dazzan P, Soulsby B, Mechelli A, Wood SJ, Velakoulis D, Phillips LJ et al. (2011). Volumetric abnormalities predating the onset of schizophrenia and affective psychoses: an MRI study in subjects at ultrahigh risk of psychosis. Schizophr Bull; e-pub ahead of print 25 April 2011.
de la Fuente-Sandoval C, Leon-Ortiz P, Favila R, Stephano S, Mamo D, Ramirez-Bermudez J et al. (2011). Higher levels of glutamate in the associative-striatum of subjects with prodromal symptoms of schizophrenia and patients with first-episode psychosis. Neuropsychopharmacology 36: 1781–1791.
Egerton A, Fusar-Poli P, Stone JM (2012). Glutamate and psychosis risk. Curr Pharm Des 18: 466–478.
Fornito A, Yung AR, Wood SJ, Phillips LJ, Nelson B, Cotton S et al. (2008). Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol Psychiatry 64: 758–765.
Fusar-Poli P, Radua J, McGuire P, Borgwardt S (2011). Neuroanatomical maps of psychosis onset: voxel-wise meta-analysis of antipsychotic-naive VBM studies. Schizophr Bull; e-pub ahead of print 10 November 2011.
Gallinat J, Kunz D, Lang UE, Neu P, Kassim N, Kienast T et al. (2007). Association between cerebral glutamate and human behaviour: the sensation seeking personality trait. Neuroimage 34: 671–678.
Hall RC (1995). Global assessment of functioning. A modified scale. Psychosomatics 36: 267–275.
Hancu I (2009). Optimized glutamate detection at 3T. J Magn Reson Imaging 30: 1155–1162.
Javitt DC (2004). Glutamate as a therapeutic target in psychiatric disorders. Mol Psychiatry 9: 984–997.
Javitt DC, Duncan L, Balla A, Sershen H (2005). Inhibition of system A-mediated glycine transport in cortical synaptosomes by therapeutic concentrations of clozapine: implications for mechanisms of action. Mol Psychiatry 10: 275–287.
Jessen F, Fingerhut N, Sprinkart AM, Kuhn KU, Petrovsky N, Maier W et al. (2011). N-acetylaspartylglutamate (NAAG) and N-acetylaspartate (NAA) in patients with schizophrenia. Schizophr Bull; e-pub ahead of print 12 September 2011.
Kanowski M, Kaufmann J, Braun J, Bernarding J, Tempelmann C (2004). Quantitation of simulated short echo time 1H human brain spectra by LCModel and AMARES. Magn Reson Med 51: 904–912.
Kapur S, Zipursky R, Jones C, Remington G, Houle S (2000). Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry 157: 514–520.
Karch S, Pogarell O, Mulert C (2012). Functional magnetic resonance imaging and treatment strategies in schizophrenia. Curr Pharm Biotechnol 13: 1622–1629.
Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276.
Marsman A, van den Heuvel MP, Klomp DW, Kahn RS, Luijten PR, Hulshoff Pol HE (2011). Glutamate in schizophrenia: a focused review and meta-analysis of 1H-MRS studies. Schizophr Bull; e-pub ahead of print 11 July 2011.
McLoughlin GA, Ma D, Tsang TM, Jones DN, Cilia J, Hill MD et al. (2009). Analyzing the effects of psychotropic drugs on metabolite profiles in rat brain using 1H NMR spectroscopy. J Proteome Res 8: 1943–1952.
Pan JW, Mason GF, Pohost GM, Hetherington HP (1996). Spectroscopic imaging of human brain glutamate by water-suppressed J-refocused coherence transfer at 4.1 T. Magn Reson Med 36: 7–12.
Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ et al. (2003). Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet 361: 281–288.
Pilowsky LS, Costa DC, Ell PJ, Murray RM, Verhoeff NP, Kerwin RW (1993). Antipsychotic medication, D2 dopamine receptor blockade and clinical response: a 123I IBZM SPET (single photon emission tomography) study. Psychol Med 23: 791–797.
Pouwels PJ, Frahm J (1998). Regional metabolite concentrations in human brain as determined by quantitative localized proton MRS. Magn Reson Med 39: 53–60.
Provencher SW (1993). Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med 30: 672–679.
Reid MA, Stoeckel LE, White DM, Avsar KB, Bolding MS, Akella NS et al. (2011). Assessments of function and biochemistry of the anterior cingulate cortex in schizophrenia. Biol Psychiatry 68: 625–633.
Rothlisberger M, Riecher-Rossler A, Aston J, Fusar-Poli P, Radu EW, Borgwardt S (2012). Cingulate volume abnormalities in emerging psychosis. Curr Pharm Des 18: 495–504.
Shirayama Y, Obata T, Matsuzawa D, Nonaka H, Kanazawa Y, Yoshitome E et al. (2010). Specific metabolites in the medial prefrontal cortex are associated with the neurocognitive deficits in schizophrenia: a preliminary study. Neuroimage 49: 2783–2790.
Snitz BE, MacDonald III A, Cohen JD, Cho RY, Becker T, Carter CS (2005). Lateral and medial hypofrontality in first-episode schizophrenia: functional activity in a medication-naive state and effects of short-term atypical antipsychotic treatment. Am J Psychiatry 162: 2322–2329.
Stone JM, Day F, Tsagaraki H, Valli I, McLean MA, Lythgoe DJ et al. (2009). Glutamate dysfunction in people with prodromal symptoms of psychosis: relationship to gray matter volume. Biol Psychiatry 66: 533–539.
Stone JM, Morrison PD, Pilowsky LS (2007). Glutamate and dopamine dysregulation in schizophrenia--a synthesis and selective review. J Psychopharmacol 21: 440–452.
Stone JM, Raffin M, Morrison P, McGuire PK (2010). Review: the biological basis of antipsychotic response in schizophrenia. J Psychopharmacol 24: 953–964.
Tayoshi S, Sumitani S, Taniguchi K, Shibuya-Tayoshi S, Numata S, Iga J et al. (2009). Metabolite changes and gender differences in schizophrenia using 3-Tesla proton magnetic resonance spectroscopy (1H-MRS). Schizophr Res 108: 69–77.
Theberge J, Al-Semaan Y, Williamson PC, Menon RS, Neufeld RW, Rajakumar N et al. (2003). Glutamate and glutamine in the anterior cingulate and thalamus of medicated patients with chronic schizophrenia and healthy comparison subjects measured with 4.0-T proton MRS. Am J Psychiatry 160: 2231–2233.
Theberge J, Bartha R, Drost DJ, Menon RS, Malla A, Takhar J et al. (2002). Glutamate and glutamine measured with 4.0 T proton MRS in never-treated patients with schizophrenia and healthy volunteers. Am J Psychiatry 159: 1944–1946.
Theberge J, Williamson KE, Aoyama N, Drost DJ, Manchanda R, Malla AK et al. (2007). Longitudinal grey-matter and glutamatergic losses in first-episode schizophrenia. Br J Psychiatry 191: 325–334.
Tibbo P, Hanstock C, Valiakalayil A, Allen P (2004). 3-T proton MRS investigation of glutamate and glutamine in adolescents at high genetic risk for schizophrenia. Am J Psychiatry 161: 1116–1118.
Van Elst LT, Valerius G, Buchert M, Thiel T, Rusch N, Bubl E et al. (2005). Increased prefrontal and hippocampal glutamate concentration in schizophrenia: evidence from a magnetic resonance spectroscopy study. Biol Psychiatry 58: 724–730.
Wood SJ, Yucel M, Wellard RM, Harrison BJ, Clarke K, Fornito A et al. (2007). Evidence for neuronal dysfunction in the anterior cingulate of patients with schizophrenia: a proton magnetic resonance spectroscopy study at 3 T. Schizophr Res 94: 328–331.
Acknowledgements
This work was supported by the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry, King's College London. We thank the study participants and the radiography team at the Centre for Neuroimaging Sciences, Institute of Psychiatry, King's College London.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
GJB received honoraria for teaching from General Electric during the course of this work. In the past 3 years, JS has received a non-restricted academic fellowship from GlaxoSmithKline, and honoraria from Roche, AstraZeneca, Behrenberg Bank, and Pfizer. The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Egerton, A., Brugger, S., Raffin, M. et al. Anterior Cingulate Glutamate Levels Related to Clinical Status Following Treatment in First-Episode Schizophrenia. Neuropsychopharmacol 37, 2515–2521 (2012). https://doi.org/10.1038/npp.2012.113
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2012.113
Keywords
This article is cited by
-
Association between increased anterior cingulate glutamate and psychotic-like experiences, but not autistic traits in healthy volunteers
Scientific Reports (2023)
-
Association of default-mode network neurotransmitters and inter-network functional connectivity in first episode psychosis
Neuropsychopharmacology (2023)
-
Glutamatergic basis of antipsychotic response in first-episode psychosis: a dual voxel study of the anterior cingulate cortex
Neuropsychopharmacology (2023)
-
Anterior cingulate glutamate metabolites as a predictor of antipsychotic response in first episode psychosis: data from the STRATA collaboration
Neuropsychopharmacology (2023)
-
Variability and magnitude of brain glutamate levels in schizophrenia: a meta and mega-analysis
Molecular Psychiatry (2023)