Abstract
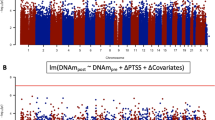
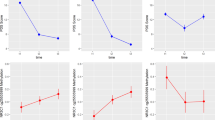
Genomic variation in the SKA2 gene has recently been identified as a promising suicide biomarker. In light of its role in glucocorticoid receptor transactivation, we investigated whether SKA2 DNA methylation influences cortisol stress reactivity and is involved in the development of post-traumatic stress disorder (PTSD). Increased SKA2 methylation was significantly associated with lower cortisol stress reactivity in 85 healthy individuals exposed to the Trier Social Stress Test (B=−173.40, t=−2.324, p-value=0.023). Next, we observed that longitudinal decreases in SKA2 methylation after deployment were associated with the emergence of post-deployment PTSD symptoms in a Dutch military cohort (N=93; B=−0.054, t=−3.706, p-value=3.66 × 10−4). In contrast, exposure to traumatic stress during deployment by itself resulted in longitudinal increases in SKA2 methylation (B=0.037, t=4.173, p-value=6.98 × 10−5). Using pre-deployment SKA2 methylation levels and childhood trauma exposure, we found that the previously published suicide prediction rule significantly predicted post-deployment PTSD symptoms (AUC=0.66, 95% CI: 0.53–0.79) with an optimal sensitivity of 0.81 and specificity of 0.91. Permutation analysis using random methylation loci supported these findings. Together, these data establish the importance of SKA2 for cortisol stress responsivity and the development of PTSD and provide further evidence that SKA2 is a promising biomarker for stress-related disorders including PTSD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T et al (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 27: 169–190.
Boks MP, Schipper M, Schubart CD, Sommer IE, Kahn RS, Ophoff RA (2007). Investigating gene environment interaction in complex diseases: increasing power by selective sampling for environmental exposure. Int J Epidemiol 36: 1363–1369.
Boks MP, van Mierlo HC, Rutten BP, Radstake TR, de Wit L, Geuze E et al (2015). Longitudinal changes of telomere length and epigenetic age related to traumatic stress and post-traumatic stress disorder. Psychoneuroendocrinology 51: 506–512.
Bremner JD, Bolus R, Mayer EA (2007). Psychometric properties of the Early Trauma Inventory-Self Report. J Nerv Ment Dis 195: 211–218.
Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF et al (2007). Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry 62: 1080–1087.
De Kloet CS, Vermetten E, Geuze E, Kavelaars A, Heijnen CJ, Westenberg HG (2006). Assessment of HPA-axis function in posttraumatic stress disorder: pharmacological and non-pharmacological challenge tests, a review. J Psychiatr Res 40: 550–567.
Derogatis LR, Lipman RS, Covi L (1973). SCL-90: an outpatient psychiatric rating scale–preliminary report. Psychopharmacol Bull 9: 13–28.
Guintivano J, Brown T, Newcomer A, Jones M, Cox O, Maher BS et al (2014). Identification and replication of a combined epigenetic and genetic biomarker predicting suicide and suicidal behaviors. Am J Psychiatry 171: 1287–1296.
Heim C, Newport DJ, Miller AH, Nemeroff CB (2000). Long-term neuroendocrine effects of childhood maltreatment. JAMA 284: 2321.
Houtepen LC, Boks MP, Kahn RS, Joels M, Vinkers CH (2015). Antipsychotic use is associated with a blunted cortisol stress response: a study in euthymic bipolar disorder patients and their unaffected siblings. Eur Neuropsychopharmacol 25: 77–84.
Hovens JE, Ramsen I, van der Ploeg HM (2000) Selfreport Measure For PTSD Symptoms: SIP Manual. Swets & Zeitlinger: Leiden, The Netherlands.
Hovens JE, Bramsen I, van der Ploeg HM (2002). Self-rating inventory for posttraumatic stress disorder: review of the psychometric properties of a new brief Dutch screening instrument. Percept Mot Skills 94: 996–1008.
Jaffe AE, Irizarry RA (2014). Accounting for cellular heterogeneity is critical in epigenome-wide association studies. Genome Biol 15: R31.
Keane TM, Caddell JM, Taylor KL (1988). Mississippi scale for combat-related posttraumatic stress disorder: three studies in reliability and validity. J Consult Clin Psychol 56: 85–90.
Klengel T, Mehta D, Anacker C, Rex-Haffner M, Pruessner JC, Pariante CM et al (2013). Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions. Nat Neurosci 16: 33–41.
Lovallo WR, Farag NH, Sorocco KH, Cohoon AJ, Vincent AS (2012). Lifetime adversity leads to blunted stress axis reactivity: studies from the Oklahoma Family Health Patterns Project. Biol Psychiatry 71: 344–349.
Malan-Muller S, Seedat S, Hemmings SM (2014). Understanding posttraumatic stress disorder: insights from the methylome. Genes Brain Behav 13: 52–68.
Mehta D, Binder EB (2012). Gene x environment vulnerability factors for PTSD: the HPA-axis. Neuropharmacology 62: 654–662.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 28: 916–931.
Reijnen A, Rademaker AR, Vermetten E, Geuze E (2015). Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry 30: 341–346.
Rice L, Waters CE, Eccles J, Garside H, Sommer P, Kay P et al (2008). Identification and functional analysis of SKA2 interaction with the glucocorticoid receptor. J Endocrinol 198: 499–509.
Sandweiss DA, Slymen DJ, Leardmann CA, Smith B, White MR, Boyko EJ et al (2011). Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Arch Gen Psychiatry 68: 496–504.
Schoenbaum M, Kessler RC, Gilman SE, Colpe LJ, Heeringa SG, Stein MB et al (2014). Predictors of suicide and accident death in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry 71: 493–503.
Schubeler D (2015). Function and information content of DNA methylation. Nature 517: 321–326.
Sundin J, Fear NT, Iversen A, Rona RJ, Wessely S (2010). PTSD after deployment to Iraq: conflicting rates, conflicting claims. Psychol Med 40: 367–382.
Thombs BD, Bernstein DP, Lobbestael J, Arntz A (2009). A validation study of the Dutch Childhood Trauma Questionnaire-Short Form: factor structure, reliability, and known-groups validity. Child Abuse Negl 33: 518–523.
Van Zuiden M, Geuze E, Maas M, Vermetten E, Heijnen CJ, Kavelaars A (2009). Deployment-related severe fatigue with depressive symptoms is associated with increased glucocorticoid binding to peripheral blood mononuclear cells. Brain Behav Immun 23: 1132–1139.
Van Zuiden M, Geuze E, Willemen HL, Vermetten E, Maas M, Heijnen CJ et al (2011). Pre-existing high glucocorticoid receptor number predicting development of posttraumatic stress symptoms after military deployment. Am J Psychiatry 168: 89–96.
Vinkers CH, Zorn JV, Cornelisse S, Koot S, Houtepen LC, Olivier B et al (2013). Time-dependent changes in altruistic punishment following stress. Psychoneuroendocrinology 38: 1467–1475.
Vinkers CH, Kalafateli AL, Rutten BP, Kas MJ, Kaminsky Z, Turner JD et al (2015a). Traumatic stress and human DNA methylation: a critical review. Epigenomics 7: 593–608.
Vinkers CH, Joëls M, Milaneschi Y, Gerritsen L, Kahn RS, Penninx BW et al (2015b). Mineralocorticoid receptor haplotypes sex-dependently moderate depression susceptibility following childhood maltreatment. Psychoneuroendocrinology 54: 90–102.
Witteveen AB, Van der Ploeg E, Bramsen I, Huizink AC, Slottje P, Smid T et al (2006). Dimensionality of the posttraumatic stress response among police officers and fire fighters: an evaluation of two self-report scales. Psychiatry Res 141: 213–228.
Yehuda R, Giller EL, Southwick SM, Lowy MT, Mason JW (1991). Hypothalamic-pituitary-adrenal dysfunction in posttraumatic stress disorder. Biol Psychiatry 30: 1031–1048.
Zovkic IB, Meadows JP, Kaas GA, Sweatt JD (2013). Interindividual Variability in Stress Susceptibility: A Role for Epigenetic Mechanisms in PTSD. Front Psychiatry 4: 60.
Acknowledgements
The data collection was funded by the Dutch Ministry of Defence. Methylation analyses were funded by the VENI Award fellowship from the Netherlands Organisation for Scientific Research (NWO, grant number 916.11.086) to BPFR. Funders had no role in design and reporting of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Boks, M., Rutten, B., Geuze, E. et al. SKA2 Methylation is Involved in Cortisol Stress Reactivity and Predicts the Development of Post-Traumatic Stress Disorder (PTSD) After Military Deployment. Neuropsychopharmacol 41, 1350–1356 (2016). https://doi.org/10.1038/npp.2015.286
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2015.286
This article is cited by
-
Decreased mononuclear cell NR3C1 SKA2 and FKPB5 expression levels among adult survivors of suicide bombing terror attacks in childhood are associated with the development of PTSD
Molecular Psychiatry (2023)
-
Biomarker Response to Mindfulness Intervention in Veterans Diagnosed with Post-traumatic Stress Disorder
Mindfulness (2022)
-
A systematic review of childhood maltreatment and DNA methylation: candidate gene and epigenome-wide approaches
Translational Psychiatry (2021)
-
Resting mononuclear cell NR3C1 and SKA2 expression levels predict blunted cortisol reactivity to combat training stress among elite army cadets exposed to childhood adversity
Molecular Psychiatry (2021)
-
Longitudinal epigenome-wide association studies of three male military cohorts reveal multiple CpG sites associated with post-traumatic stress disorder
Clinical Epigenetics (2020)