Abstract
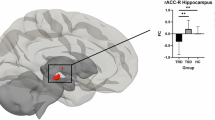
Major depressive disorder (MDD) is associated with structural and functional alterations in the prefrontal cortex (PFC) and anterior cingulate cortex (ACC). Enhanced ACC activity at rest (measured using various imaging methodologies) is found in treatment-responsive patients and is hypothesized to bolster treatment response by fostering adaptive rumination. However, whether structural changes influence functional coupling between fronto-cingulate regions and ACC regional homogeneity (ReHo) and whether these functional changes are related to levels of adaptive rumination and treatment response is still unclear. Cortical thickness and ReHo maps were calculated in 21 unmedicated depressed patients and 35 healthy controls. Regions with reduced cortical thickness defined the seeds for the subsequent functional connectivity (FC) analyses. Patients completed the Response Style Questionnaire, which provided a measure of adaptive rumination associated with better response to psychotherapy. Compared with controls, depressed patients showed thinning of the right anterior PFC, increased prefrontal connectivity with the supragenual ACC (suACC), and higher ReHo in the suACC. The suACC clusters of increased ReHo and FC spatially overlapped. In depressed patients, suACC ReHo scores positively correlated with PFC thickness and with FC strength. Moreover, stronger fronto-cingulate connectivity was related to higher levels of adaptive rumination. Greater suACC ReHo and connectivity with the right anterior PFC seem to foster adaptive forms of self-referential processing associated with better response to psychotherapy, whereas prefrontal thinning impairs the ability of depressed patients to engage the suACC during a major depressive episode. Bolstering the function of the suACC may represent a potential target for treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Alexopoulos GS, Hoptman MJ, Kanellopoulos D, Murphy CF, Lim KO, Gunning FM (2012). Functional connectivity in the cognitive control network and the default mode network in late-life depression. J Affect Disord 139: 56–65.
Amico F, Meisenzahl E, Koutsouleris N, Reiser M, Moller HJ, Frodl T (2011). Structural MRI correlates for vulnerability and resilience to major depressive disorder. J Psychiatry Neurosci 36: 15–22.
Ashburner J (2007). A fast diffeomorphic image registration algorithm. Neuroimage 38: 95–113.
Beck AT, Steer RA, Ball R, Ranieri W (1996). Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess 67: 588–597.
Bermpohl F, Walter M, Sajonz B, Lucke C, Hagele C, Sterzer P et al (2009). Attentional modulation of emotional stimulus processing in patients with major depression—alterations in prefrontal cortical regions. Neurosci Lett 463: 108–113.
Bora E, Fornito A, Pantelis C, Yucel M (2012). Gray matter abnormalities in major depressive disorder: a meta-analysis of voxel based morphometry studies. J Affect Disord 138: 9–18.
Buckner RL, Andrews-Hanna JR, Schacter DL (2008). The brain's default network: anatomy, function, and relevance to disease. Ann NY Acad Sci 1124: 1–38.
Burwell RA, Shirk SR (2007). Subtypes of rumination in adolescence: associations between brooding, reflection, depressive symptoms, and coping. J Clin Child Adolesc Psychol 36: 56–65.
Chao-Gan Y, Yu-Feng Z (2010). DPARSF: a MATLAB toolbox for ‘pipeline’ data analysis of resting-state fMRI. Front Syst Neurosci 4: 13.
Chen AC, Oathes DJ, Chang C, Bradley T, Zhou ZW, Williams LM et al (2013a). Causal interactions between fronto-parietal central executive and default-mode networks in humans. Proc Natl Acad Sci USA 110: 19944–19949.
Chen CH, Ridler K, Suckling J, Williams S, Fu CH, Merlo-Pich E et al (2007). Brain imaging correlates of depressive symptom severity and predictors of symptom improvement after antidepressant treatment. Biol Psychiatry 62: 407–414.
Chen J, Zhou C, Wu B, Wang Y, Li Q, Wei Y et al (2013b). Left versus right repetitive transcranial magnetic stimulation in treating major depression: a meta-analysis of randomised controlled trials. Psychiatry Res 210: 1260–1264.
Dale AM, Fischl B, Sereno MI (1999). Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage 9: 179–194.
Downar J, Daskalakis ZJ (2013). New targets for rTMS in depression: a review of convergent evidence. Brain Stimul 6: 231–240.
Fischl B, Dale AM (2000). Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA 97: 11050–11055.
Fischl B, Sereno MI, Dale AM (1999). Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage 9: 195–207.
Franz M, Lemke MR, Meyer T, Ulferts J, Puhl P, Snaith RP (1998). [German version of the Snaith-Hamilton-Pleasure Scale (SHAPS-D). Anhedonia in schizophrenic and depressive patients]. Fortschr Neurol Psychiatr 66: 407–413.
Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R (1996). Movement-related effects in fMRI time-series. Magn Reson Med 35: 346–355.
Friston KJ, Worsley KJ, Frackowiak RS, Mazziotta JC, Evans AC (1994). Assessing the significance of focal activations using their spatial extent. Hum Brain Mapp 1: 210–220.
Frodl T, Jager M, Born C, Ritter S, Kraft E, Zetzsche T et al (2008). Anterior cingulate cortex does not differ between patients with major depression and healthy controls, but relatively large anterior cingulate cortex predicts a good clinical course. Psychiatry Res 163: 76–83.
Hamilton JP, Furman DJ, Chang C, Thomason ME, Dennis E, Gotlib IH (2011). Default-mode and task-positive network activity in major depressive disorder: implications for adaptive and maladaptive rumination. Biol Psychiatry 70: 327–333.
Heller AS, Johnstone T, Peterson MJ, Kolden GG, Kalin NH, Davidson RJ (2013). Increased prefrontal cortex activity during negative emotion regulation as a predictor of depression symptom severity trajectory over 6 months. JAMA Psychiatry 70: 1181–1189.
Helmreich I, Wagner S, Mergl R, Allgaier AK, Hautzinger M, Henkel V et al (2011). The Inventory Of Depressive Symptomatology (IDS-C(28)) is more sensitive to changes in depressive symptomatology than the Hamilton Depression Rating Scale (HAMD(17)) in patients with mild major, minor or subsyndromal depression. Eur Arch Psychiatry Clin Neurosci 261: 357–367.
Henkel V, Seemuller F, Obermeier M, Adli M, Bauer M, Mundt C et al (2009). Does early improvement triggered by antidepressants predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord 115: 439–449.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR et al (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289: 3095–3105.
Koolschijn PC, van Haren NE, Lensvelt-Mulders GJ, Hulshoff Pol HE, Kahn RS (2009). Brain volume abnormalities in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Hum Brain Mapp 30: 3719–3735.
Krampen G (1994). Skalen zur Erfassung von Hoffnungslosigkeit (H-Skalen). Deutsche Bearbeitung und Weiterentwicklung der H-Skala von Aaron T Beck. Hogrefe: Göttingen, Germany.
Kuhn S, Gallinat J (2013). Resting-state brain activity in schizophrenia and major depression: a quantitative meta-analysis. Schizophr Bull 39: 358–365.
Kuhn S, Vanderhasselt MA, De Raedt R, Gallinat J (2012). Why ruminators won't stop: the structural and resting state correlates of rumination and its relation to depression. J Affect Disord 141: 352–360.
Kühner C, Huffziger S, Nolen-Hoeksema S (2007) Response Styles Questionnaire—Deutsche Version (RSQ-D). Hogrefe: Göttingen, Germany.
Lai CH (2013). Gray matter volume in major depressive disorder: a meta-analysis of voxel-based morphometry studies. Psychiatry Res 211: 37–46.
Lai CH, Wu YT (2012). Frontal regional homogeneity increased and temporal regional homogeneity decreased after remission of first-episode drug-naive major depressive disorder with panic disorder patients under duloxetine therapy for 6 weeks. J Affect Disord 136: 453–458.
Laux L, Glanzmann P, Schaffner P, Spielberger CD (1981) Das State-Trait-Angstinventar. Theoretische Grundlagen und Handanweisungen. Beltz Testgesellschaft: Weinheim, Germany.
Li M, Metzger CD, Li W, Safron A, van Tol MJ, Lord A et al (2014). Dissociation of glutamate and cortical thickness is restricted to regions subserving trait but not state markers in major depressive disorder. J Affect Disord 169: 91–100.
Liao W, Chen H, Feng Y, Mantini D, Gentili C, Pan Z et al (2010). Selective aberrant functional connectivity of resting state networks in social anxiety disorder. Neuroimage 52: 1549–1558.
Liu F, Guo W, Liu L, Long Z, Ma C, Xue Z et al (2013). Abnormal amplitude low-frequency oscillations in medication-naive, first-episode patients with major depressive disorder: a resting-state fMRI study. J Affect Disord 146: 401–406.
Logothetis NK, Murayama Y, Augath M, Steffen T, Werner J, Oeltermann A (2009). How not to study spontaneous activity. Neuroimage 45: 1080–1089.
Nejad AB, Fossati P, Lemogne C (2013). Self-referential processing, rumination, and cortical midline structures in major depression. Front Hum Neurosci 7: 666.
Northoff G, Duncan NW, Hayes DJ (2010). The brain and its resting state activity—experimental and methodological implications. Prog Neurobiol 92: 593–600.
Paus T, Castro-Alamancos MA, Petrides M (2001). Cortico-cortical connectivity of the human mid-dorsolateral frontal cortex and its modulation by repetitive transcranial magnetic stimulation. Eur J Neurosci 14: 1405–1411.
Peterson BS, Wang Z, Horga G, Warner V, Rutherford B, Klahr KW et al (2014). Discriminating risk and resilience endophenotypes from lifetime illness effects in familial major depressive disorder. JAMA Psychiatry 71: 136–148.
Peterson BS, Warner V, Bansal R, Zhu H, Hao X, Liu J et al (2009). Cortical thinning in persons at increased familial risk for major depression. Proc Natl Acad Sci USA 106: 6273–6278.
Pizzagalli DA (2011). Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology 36: 183–206.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL (2001). A default mode of brain function. Proc Natl Acad Sci USA 98: 676–682.
Rentzsch J, Adli M, Wiethoff K, Gomez-Carrillo de Castro A, Gallinat J (2014). Pretreatment anterior cingulate activity predicts antidepressant treatment response in major depressive episodes. Eur Arch Psychiatry Clin Neurosci 264: 213–223.
Salomons TV, Dunlop K, Kennedy SH, Flint A, Geraci J, Giacobbe P et al (2014). Resting-state cortico-thalamic-striatal connectivity predicts response to dorsomedial prefrontal rTMS in major depressive disorder. Neuropsychopharmacology 39: 488–498.
Siegle GJ, Carter CS, Thase ME (2006). Use of FMRI to predict recovery from unipolar depression with cognitive behavior therapy. Am J Psychiatry 163: 735–738.
Treynor W, Gonzalez R, Nolen-Hoeksema S (2003). Rumination Reconsidered: A Psychometric Analysis. Cogn Ther Res 27: 247–259.
Tu PC, Chen LF, Hsieh JC, Bai YM, Li CT, Su TP (2012). Regional cortical thinning in patients with major depressive disorder: a surface-based morphometry study. Psychiatry Res 202: 206–213.
Van Dijk KR, Sabuncu MR, Buckner RL (2012). The influence of head motion on intrinsic functional connectivity MRI. Neuroimage 59: 431–438.
van Eijndhoven P, van Wingen G, Katzenbauer M, Groen W, Tepest R, Fernandez G et al (2013). Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. Am J Psychiatry 170: 1477–1486.
van Tol MJ, Li M, Metzger CD, Hailla N, Horn DI, Li W et al (2013). Local cortical thinning links to resting-state disconnectivity in major depressive disorder. Psychol Med 1: 1–13.
van Tol MJ, van der Wee NJ, van den Heuvel OA, Nielen MM, Demenescu LR, Aleman A et al (2010). Regional brain volume in depression and anxiety disorders. Arch Gen Psychiatry 67: 1002–1011.
Wang L, Li K, Zhang Q, Zeng Y, Dai W, Su Y et al (2014). Short-term effects of escitalopram on regional brain function in first-episode drug-naive patients with major depressive disorder assessed by resting-state functional magnetic resonance imaging. Psychol Med 44: 1417–1426.
Wu QZ, Li DM, Kuang WH, Zhang TJ, Lui S, Huang XQ et al (2011). Abnormal regional spontaneous neural activity in treatment-refractory depression revealed by resting-state fMRI. Hum Brain Mapp 32: 1290–1299.
Yan CG, Cheung B, Kelly C, Colcombe S, Craddock RC, Di Martino A et al (2013). A comprehensive assessment of regional variation in the impact of head micromovements on functional connectomics. Neuroimage 76: 183–201.
Yao Z, Wang L, Lu Q, Liu H, Teng G (2009). Regional homogeneity in depression and its relationship with separate depressive symptom clusters: a resting-state fMRI study. J Affect Disord 115: 430–438.
Zuo XN, Di Martino A, Kelly C, Shehzad ZE, Gee DG, Klein DF et al (2010). The oscillating brain: complex and reliable. Neuroimage 49: 1432–1445.
Acknowledgements
We thank Dr Philip Stämpfli and Dr Esther Sydekum for their invaluable assistance in study procedures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Späti, J., Hänggi, J., Doerig, N. et al. Prefrontal Thinning Affects Functional Connectivity and Regional Homogeneity of the Anterior Cingulate Cortex in Depression. Neuropsychopharmacol 40, 1640–1648 (2015). https://doi.org/10.1038/npp.2015.8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2015.8
This article is cited by
-
Brain connectivity in major depressive disorder: a precision component of treatment modalities?
Translational Psychiatry (2023)
-
Decreased cortical thickness of left premotor cortex as a treatment predictor in major depressive disorder
Brain Imaging and Behavior (2021)
-
Meta-analysis of cortical thickness abnormalities in medication-free patients with major depressive disorder
Neuropsychopharmacology (2020)
-
Cortical thickness reductions associate with abnormal resting-state functional connectivity in non-neuropsychiatric systemic lupus erythematosus
Brain Imaging and Behavior (2018)