Abstract
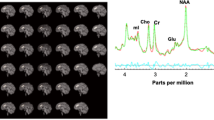
Smoking withdrawal negatively impacts inhibitory control, and these effects are greater for smokers with preexisting attention problems, such as attention deficit/hyperactivity disorder (ADHD). The current study preliminarily evaluated changes in inhibitory control-related behavior and brain activation during smoking withdrawal among smokers with ADHD. Moreover, we investigated the role of catecholamine transmission in these changes by examining the effects of 40 mg methylphenidate (MPH) administration. Adult daily smokers with (n=17) and without (n=20) ADHD completed fMRI scanning under each of three conditions: (a) smoking as usual+placebo; (b) 24 h smoking abstinence+placebo and (c) 24 h smoking abstinence+MPH. Scan order was randomized and counterbalanced. Participants completed a modified Go/No-Go task to assess both sustained and transient inhibitory control. Voxelwise analysis of task-related BOLD signal revealed a significant group-by-abstinence interaction in occipital/parietal cortex during sustained inhibition, with greater abstinence-induced decreases in activation observed among ADHD smokers compared with non-ADHD smokers. Changes in behavioral performance during abstinence were associated with changes in activation in regions of occipital and parietal cortex and bilateral insula during sustained inhibition in both groups. MPH administration improved behavioral performance and increased sustained inhibitory control-related activation for both groups. During transient inhibition, MPH increased prefrontal activation for both groups and increased striatal activation only among ADHD smokers. These preliminary findings suggest that abstinence-induced changes in catecholamine transmission in visual attention areas (eg, occipital and superior parietal cortex) may be associated with inhibitory control deficits and contribute to smoking vulnerability among individuals with ADHD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Addicott MA, Sweitzer MM, Froeliger B, Rose JE, McClernon FJ (2015). Increased functional connectivity in an insula-based network is associated with improved smoking cessation outcomes. Neuropsychopharmacology 40: 2648–2656.
Ahrendts J, Rusch N, Wilke M, Philipsen A, Eickhoff SB, Glauche V et al (2011). Visual cortex abnormalities in adults with ADHD: a structural MRI study. World J Biol Psychiatry 12: 260–270.
Ashare RL, Falcone M, Lerman C (2014). Cognitive function during nicotine withdrawal: Implications for nicotine dependence treatment. Neuropharmacology 76 (Pt B): 581–591.
Ashare RL, Hawk LW Jr. (2012). Effects of smoking abstinence on impulsive behavior among smokers high and low in ADHD-like symptoms. Psychopharmacology 219: 537–547.
Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 121: 65–94.
Bennett IJ, Motes MA, Rao NK, Rypma B (2012). White matter tract integrity predicts visual search performance in young and older adults. Neurobiol Aging 33: 433 e421–433.e431.
Berridge CW, Devilbiss DM, Andrzejewski ME, Arnsten AF, Kelley AE, Schmeichel B et al (2006). Methylphenidate preferentially increases catecholamine neurotransmission within the prefrontal cortex at low doses that enhance cognitive function. Biol Psychiatry 60: 1111–1120.
Castellanos FX, Proal E (2012). Large-scale brain systems in ADHD: beyond the prefrontal-striatal model. Trends Cogn Sci 16: 17–26.
Chikazoe J, Jimura K, Asari T, Yamashita K, Morimoto H, Hirose S et al (2009). Functional dissociation in right inferior frontal cortex during performance of go/no-go task. Cereb Cortex 19: 146–152.
Cocchi L, Bramati IE, Zalesky A, Furukawa E, Fontenelle LF, Moll J et al (2012). Altered functional brain connectivity in a non-clinical sample of young adults with attention-deficit/hyperactivity disorder. J Neurosci 32: 17753–17761.
Congdon E, Mumford JA, Cohen JR, Galvan A, Aron AR, Xue G et al (2010). Engagement of large-scale networks is related to individual differences in inhibitory control. Neuroimage 53: 653–663.
Covey LS, Hu MC, Weissman J, Croghan I, Adler L, Winhusen T (2011). Divergence by ADHD subtype in smoking cessation response to OROS-methylphenidate. Nicotine Tob Res 13: 1003–1008.
Cubillo A, Halari R, Smith A, Taylor E, Rubia K (2012). A review of fronto-striatal and fronto-cortical brain abnormalities in children and adults with Attention Deficit Hyperactivity Disorder (ADHD) and new evidence for dysfunction in adults with ADHD during motivation and attention. Cortex 48: 194–215.
Dillo W, Goke A, Prox-Vagedes V, Szycik GR, Roy M, Donnerstag F et al (2010). Neuronal correlates of ADHD in adults with evidence for compensation strategies—a functional MRI study with a Go/No-Go paradigm. Ger Med Sci 8: Doc09.
Engert V, Pruessner JC (2008). Dopaminergic and noradrenergic contributions to functionality in ADHD: the role of methylphenidate. Curr Neuropharmacol 6: 322–328.
Froeliger B, McConnell PA, Bell S, Sweitzer M, Kozink RV, Eichberg C et al (2017). Association between baseline corticothalamic-mediated inhibitory control and smoking relapse vulnerability. JAMA Psychiatry 74: 379–386.
Ghahremani DG, Lee B, Robertson CL, Tabibnia G, Morgan AT, De Shetler N et al (2012). Striatal dopamine D(2)/D(3) receptors mediate response inhibition and related activity in frontostriatal neural circuitry in humans. J Neurosci 32: 7316–7324.
Greenberg AS, Verstynen T, Chiu YC, Yantis S, Schneider W, Behrmann M (2012). Visuotopic cortical connectivity underlying attention revealed with white-matter tractography. J Neurosci 32: 2773–2782.
Hannestad J, Gallezot JD, Planeta-Wilson B, Lin SF, Williams WA, van Dyck CH et al (2010). Clinically relevant doses of methylphenidate significantly occupy norepinephrine transporters in humans in vivo. Biol Psychiatry 68: 854–860.
Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K (2013). Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects. JAMA Psychiatry 70: 185–198.
Humfleet GL, Prochaska JJ, Mengis M, Cullen J, Munoz R, Reus V et al (2005). Preliminary evidence of the association between the history of childhood attention-deficit/hyperactivity disorder and smoking treatment failure. Nicotine Tob Res 7: 453–460.
Janes AC, Pizzagalli DA, Richardt S, Frederick Bde B, Holmes AJ, Sousa J et al (2010). Neural substrates of attentional bias for smoking-related cues: an FMRI study. Neuropsychopharmacology 35: 2339–2345.
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O et al (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 163: 716–723.
Kollins SH, English JS, Itchon-Ramos N, Chrisman AK, Dew R, O'Brien B et al (2014). A pilot study of lis-dexamfetamine dimesylate (LDX/SPD489) to facilitate smoking cessation in nicotine-dependent adults with ADHD. J Atten Disord 18: 158–168.
Kollins SH, English JS, Roley ME, O'Brien B, Blair J, Lane SD et al (2013). Effects of smoking abstinence on smoking-reinforced responding, withdrawal, and cognition in adults with and without attention deficit hyperactivity disorder. Psychopharmacology 227: 19–30.
Kozink RV, Kollins SH, McClernon FJ (2010). Smoking withdrawal modulates right inferior frontal cortex but not presupplementary motor area activation during inhibitory control. Neuropsychopharmacology 35: 2600–2606.
McClernon FJ, Addicott MA, Sweitzer MM (2015). Smoking abstinence and neurocognition: implications for cessation and relapse. Curr Top Behav Neurosci 23: 193–227.
McClernon FJ, Kollins SH (2008a). ADHD and smoking: from genes to brain to behavior. Ann NY Acad Sci 1141: 131–147.
McClernon FJ, Kollins SH, Lutz AM, Fitzgerald DP, Murray DW, Redman C et al (2008b). Effects of smoking abstinence on adult smokers with and without attention deficit hyperactivity disorder: results of a preliminary study. Psychopharmacology 197: 95–105.
McClernon FJ, Van Voorhees EE, English J, Hallyburton M, Holdaway A, Kollins SH (2011). Smoking withdrawal symptoms are more severe among smokers with ADHD and independent of ADHD symptom change: results from a 12-day contingency-managed abstinence trial. Nicotine Tob Res 13: 784–792.
Milberger S, Biederman J, Faraone SV, Chen L, Jones J (1997). ADHD is associated with early initiation of cigarette smoking in children and adolescents. J Am Acad Child Adolesc Psychiatry 36: 37–44.
Molina BS, Pelham WE Jr. (2003). Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol 112: 497–507.
Muller CP, Huston JP (2007). Dopamine activity in the occipital and temporal cortices of rats: dissociating effects of sensory but not pharmacological stimulation. Synapse 61: 254–258.
Noudoost B, Moore T (2011). Control of visual cortical signals by prefrontal dopamine. Nature 474: 372–375.
Parks EL, Madden DJ (2013). Brain connectivity and visual attention. Brain Connect 3: 317–338.
Pironti VA, Lai MC, Muller U, Dodds CM, Suckling J, Bullmore ET et al (2014). Neuroanatomical abnormalities and cognitive impairments are shared by adults with attention-deficit/hyperactivity disorder and their unaffected first-degree relatives. Biol Psychiatry 76: 639–647.
Pomerleau OF, Downey KK, Stelson FW, Pomerleau CS (1995). Cigarette smoking in adult patients diagnosed with attention deficit hyperactivity disorder. J Subst Abuse 7: 373–378.
Powell J, Dawkins L, West R, Powell J, Pickering A (2010). Relapse to smoking during unaided cessation: clinical, cognitive and motivational predictors. Psychopharmacology 212: 537–549.
Proal E, Reiss PT, Klein RG, Mannuzza S, Gotimer K, Ramos-Olazagasti MA et al (2011). Brain gray matter deficits at 33-year follow-up in adults with attention-deficit/hyperactivity disorder established in childhood. Arch Gen Psychiatry 68: 1122–1134.
Shiffman SM, Jarvik ME (1976). Smoking withdrawal symptoms in two weeks of abstinence. Psychopharmacology 50: 35–39.
Simmonds DJ, Pekar JJ, Mostofsky SH (2008). Meta-analysis of Go/No-go tasks demonstrating that fMRI activation associated with response inhibition is task-dependent. Neuropsychologia 46: 224–232.
Vaidya CJ, Austin G, Kirkorian G, Ridlehuber HW, Desmond JE, Glover GH et al (1998). Selective effects of methylphenidate in attention deficit hyperactivity disorder: a functional magnetic resonance study. Proc Natl Acad Sci USA 95: 14494–14499.
Van Voorhees EE, Mitchell JT, McClernon FJ, Beckham JC, Kollins SH (2012). Sex, ADHD symptoms, and smoking outcomes: an integrative model. Med Hypotheses 78: 585–593.
Volkow ND, Wang GJ, Fowler JS, Ding YS (2005). Imaging the effects of methylphenidate on brain dopamine: new model on its therapeutic actions for attention-deficit/hyperactivity disorder. Biol Psychiatry 57: 1410–1415.
Volkow ND, Wang GJ, Kollins SH, Wigal TL, Newcorn JH, Telang F et al (2009). Evaluating dopamine reward pathway in ADHD: clinical implications. JAMA 302: 1084–1091.
Volkow ND, Wang GJ, Newcorn J, Telang F, Solanto MV, Fowler JS et al (2007). Depressed dopamine activity in caudate and preliminary evidence of limbic involvement in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 64: 932–940.
Watanabe J, Sugiura M, Sato K, Sato Y, Maeda Y, Matsue Y et al (2002). The human prefrontal and parietal association cortices are involved in NO-GO performances: an event-related fMRI study. Neuroimage 17: 1207–1216.
Willcutt EG (2012). The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9: 490–499.
Winhusen TM, Somoza EC, Brigham GS, Liu DS, Green CA, Covey LS et al (2010). Impact of attention-deficit/hyperactivity disorder (ADHD) treatment on smoking cessation intervention in ADHD smokers: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 71: 1680–1688.
Xue G, Aron AR, Poldrack RA (2008). Common neural substrates for inhibition of spoken and manual responses. Cereb Cortex 18: 1923–1932.
Zhang L, Dong Y, Doyon WM, Dani JA (2012). Withdrawal from chronic nicotine exposure alters dopamine signaling dynamics in the nucleus accumbens. Biol Psychiatry 71: 184–191.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Sweitzer, M., Kollins, S., Kozink, R. et al. ADHD, Smoking Withdrawal, and Inhibitory Control: Results of a Neuroimaging Study with Methylphenidate Challenge. Neuropsychopharmacol. 43, 851–858 (2018). https://doi.org/10.1038/npp.2017.248
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2017.248
This article is cited by
-
Attention-deficit/hyperactivity disorder and the explore/exploit trade-off
Neuropsychopharmacology (2021)
-
Does methylphenidate use affect sperm parameters in patients undergoing infertility investigation? A retrospective analysis of 9769 semen samples
Archives of Gynecology and Obstetrics (2021)
-
Subcortical structures and visual divergent thinking: a resting-state functional MRI analysis
Brain Structure and Function (2021)
-
Increased subjective and reinforcing effects of initial nicotine exposure in young adults with attention deficit hyperactivity disorder (ADHD) compared to matched peers: results from an experimental model of first-time tobacco use
Neuropsychopharmacology (2020)