Abstract
Elevated blood pressure (BP) is probably the most-important modifiable risk factor for cardiovascular disease (CVD). BP influences the development of CVD, even if levels of BP are well below the usual cut-off point that defines the presence of arterial hypertension. Adequate measurement of BP is the most-important requirement for the diagnosis and treatment of patients with suspected hypertension. The use of methodologies such as ambulatory and home BP monitoring have become powerful tools for defining the 'real' BP of patients, discarding the white-coat effect, and discovering masked hypertension. Early intervention with life-style changes and antihypertensive drugs is required to obtain the best outcome for the patient. In this sense, early use of combination antihypertensive drug therapy is recommended. The treatment of resistant hypertension—the type of elevated BP that is most difficult to control—has clearly improved over the past decade. Further studies are required to define how antihypertensive therapy should be used in the earliest stages of hypertension and for the treatment of patients with a mild-to-moderate increase in global cardiovascular risk.
Key Points
-
Half of the burden of cardiovascular disease (CVD) in the general population is attributable to high blood pressure (BP); the threshold BP for the initiation of antihypertensive treatment is currently 140/90 mmHg
-
CVD and renal disease often develop in parallel in the cardiovascular continuum, and control of BP is required at all stages of this continuum to improve patient outcome
-
A BP goal of <130/80 mmHg could represent a risk for patients with coronary artery disease, but might be considered for patients with proteinuria or those at high risk of stroke
-
The prompt use of combination antihypertensive drug therapy facilitates initial BP control; patient compliance and treatment adherence improve BP control during therapy
-
Resistant hypertension continues to occur frequently, although BP control has improved with the use of aldosterone blockers and techniques such as renal denervation and baroreceptor stimulation
-
New studies, particularly of the early stages of arterial hypertension, are required and a more-frequent use ambulatory and home BP measurements is recommended
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, accounting for 30% of all deaths.1 Elevated blood pressure (BP) is probably the most-important modifiable risk factor for CVD. Findings from prospective cohort studies have established a graded positive association between BP and the risk of CVD, starting at 115 mmHg for systolic BP.2 Box 1 contains the various grades (or stages) of BP observed in the general population, as defined by the European Society of Hypertension (ESH)3 and in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. (JNC7).4 BP contributes to the development of cardiovascular and other diseases, even when BP levels are normal or high-normal (prehypertension), and the development of such diseases accelerates with increasing levels of BP.
The effectiveness of antihypertensive therapy was initially demonstrated in patients with systolic BP >160 mmHg, and the results of early prospective trials were reviewed by Collins et al. over two decades ago.5 Around the same time, the effectiveness of antihypertensive therapy in elderly patients (aged >60 years) was also demonstrated.6 The preventive capacity of life-style changes, such as switching to a healthy diet, has been studied in the Dietary Approaches to Stop Hypertension (DASH) trial7,8 and is established for variations of the Mediterranean diet, which has proven to reduce cardiovascular morbidity and mortality.9,10 Results of a meta-analysis from 2011 have also shown a significant reduction in cardiovascular events associated with a diminution in salt intake.11 A complete intervention, including life-style changes and antihypertensive drugs, is usually only considered in patients who present with hypertension (grade 1 or higher) and in a small percentage of individuals with high-normal BP, if they have established cardiovascular or renal disease. All other patients with prehypertension would normally only receive advice about physical activity and diet.3,4,12
In this Review, I discuss the progression of high-normal BP to overt hypertension and the associated burden of cardiovascular and renal disease. I also provide an update on the controversies and challenges involved in the treatment of patients with established arterial hypertension, such as the choice of appropriate threshold and goal BP levels, the adequate number of drugs to be used since the early stages of hypertension, and which type of combination therapy offers most advantages to the patient.
Hypertension and renal disease
Burden of disease and hypertension progression
About half of the global burden of CVD in 2001 was estimated to be attributed to high BP (defined by Lawes and colleagues as ≥115 mmHg systolic BP).1 Worldwide, 7.6 million premature deaths (about 13.5% of the global total), 54% of strokes, and 47% of cases of ischemic heart disease were caused by high BP in 2001. About half of this burden was carried by people with hypertension, the rest by patients with lower levels of BP (115–139 mmHg systolic BP).1
The progression of elevated BP to established arterial hypertension has been clearly shown in the Framingham study data.13 Findings from this seminal study have also demonstrated that the prevalence of cardiovascular morbidity and mortality is higher in individuals with normal BP than in those with optimal BP, and increases even more in patients with high-normal BP.14 With increasing age, BP progressively rises from normal BP levels to prehypertensive levels, before advancing to established arterial hypertension. The gradual progression of BP is also observed when patients are not (or insufficiently) treated, and results in the development of atherosclerosis and target organ damage (TOD), and shortens the time until symptomatic CVD or renal disease become evident.
Results of the Trial of Preventing Hypertension (TROPHY)15 and the Prevention of Hypertension with the Angiotensin-Converting-Enzyme Inhibitor Ramipril in Patients with High-Normal BP (PHARAO) study16 showed that pharmacological intervention with an angiotensin-receptor blocker or an angiotensin-converting-enzyme inhibitor is sufficient to prevent the progression of high-normal BP into established arterial hypertension, probably avoiding the subsequent increase in cardiovascular risk. Further studies are required to confirm these findings and to investigate whether such an early intervention is cost-effective and prevents cardiovascular morbidity and mortality. However, guidelines3,4,12 contemplate the use of antihypertensive drugs, in particular that of suppressors of the renin–angiotensin–aldosterone system (RAAS) in patients with high-normal BP and TOD. Combination antihypertensive therapy is also used in patients with clinically overt CVD or advanced renal disease who present with BP levels <140/90 mmHg.
The effect of antihypertensive treatment on the secondary prevention of cardiovascular events and all-cause mortality among persons without clinically defined hypertension (<140/90 mmHg) was evaluated in a meta-analysis published in 2011.17 The investigators acknowledge that antihypertensive drugs could be used for reasons other than their capacity to lower BP (because they might exert additional beneficial effects) and concluded that this type of treatment was associated with a decreased risk of stroke, congestive heart failure, composite CVD events, and all-cause mortality. Interestingly, cardiovascular mortality and the incidence of myocardial infarction were not significantly lower in patients who took antihypertensive medication with BP values <140/90 mmHg. Even so, the conclusion of the authors and an accompanying editorial was that that antihypertensive treatment was beneficial for patients with CVD and a BP <140/90 mmHg.18
The cardiorenal continuum
The concept of a 'cardiovascular continuum' has been developed by Eugene Braunwald and Victor Dzau over the past two decades.19,20,21 At present, it is more specifically known as the 'cardiorenal continuum', owing to the high prevalence of combined CVD and chronic kidney disease (Figure 1). This model can be divided into three main stages. In the first stage, only cardiovascular risk factors can be detected and no evidence of TOD is present. At this stage, adequate control of BP and of other associated modifiable cardiovascular risk factors (such as smoking, hyperlipidemia, metabolic syndrome, or diabetes mellitus) can prevent the development of diverse forms of TOD that are associated with increased cardiorenal morbidity and mortality. Manifestations of TOD that can be prevented by early intervention are microalbuminuria22,23 and left ventricular hypertrophy.24 Is the prevention of TOD sufficient to prevent future fatal and nonfatal cardiovascular events? The answer to this question is (and will probably remain) unknown, because studies that could provide the answer are highly unlikely to be performed owing to their long duration and high costs. However, the finding that any of four markers of TOD (microalbuminuria, pulse-wave velocity, left ventricular mass, and carotid plaques) can predict cardiovascular mortality independently of Systemic Coronary Risk Evaluation stratification is an argument in favor of the consideration of the prevention of TOD in daily clinical practice.25
In clinical practice, three different stages can be identified. In the first, only cardiovascular risk factors are detected. In the second stage, target-organ damage (mostly albuminuria, a low estimated glomerular filtration rate, or left ventricular hypertrophy) is discovered. The third stage is characterized by the presence of symptomatic target-organ damage or that of of established cardiovascular disease, renal disease, or both. Abbreviations: CKD, chronic kidney disease; ESRD, end-stage renal disease. Reprinted from Dzau, V. & Braunwald, E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am. Heart J. 121(4), 1244–1263 © 1991 with permission from Elsevier.
The second stage of the cardiorenal continuum is characterized by the presence of one or more of the diverse indicators of asymptomatic TOD (Box 2). Adequate control of BP and other risk factors can facilitate the regression of TOD. Preliminary data indicate that regression of albuminuria26,27 and of left ventricular hypertrophy28,29 are followed by a decrease in the number of cardiovascular events. By contrast, an increase in the urinary excretion of albumin predicts cardiovascular events or death.27 These data support the need to follow the evolution of the various forms of TOD in patients with hypertension.
The third and final stage of the continuum is characterized by the presence of clinically overt CVD, advanced-stage renal failure, or both, owing to the progression of TOD and atherosclerosis. Both conditions eventually lead to a lethal cardiovascular event or to end-stage renal disease, which, in the absence of dialysis, is also fatal. Even if high BP and associated cardiovascular risk factors are actively treated, a late intervention at stage 3 of the cardiorenal continuum, unfortunately, often merely delays the incidence of new cardiovascular or renal events.
The identification of patients at high risk of developing cardiovascular and renal events while they are in the first two stages of the cardiorenal continuum is of great importance because the majority of such events occur in these two stages.30,31 Clues for the identification of high-risk patients are age (<50 years) accompanied by the clustering of cardiovascular and renal risk factors, and the presence of diverse forms of TOD.
Challenges in antihypertensive therapy
How valid are office BP measurements?
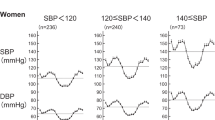
Clinicians generally agree home BP measurement should be implemented in clinical practice together with the use of ambulatory BP monitoring, both of which improve the assessment of 'real' BP levels of patients with hypertension.3,12 Both methods avoid the white-coat effect, in which patients experience elevated blood pressure in a clinical setting but not in other situations, and also allow the diagnosis of masked hypertension. Table 1 contains data from patients with established CVD or diabetes with accompanying TOD, comparing the values obtained by office BP measurement and mean 24-h systolic BP.32 Obviously, an important discrepancy exists between these two measures. A relevant percentage of patients with high-normal (prehypertension) or optimal office BP values are uncontrolled in ambulatory BP monitoring and can be considered to have masked hypertension. On the other hand, around two-thirds of patients who have high-normal values of office BP present with 24-h BP values <130 mmHg probably do not need antihypertensive therapy beyond the intervention that would be indicated if office BP was considered alone. The same is true for the >40% of patients with grade 1 hypertension who present with mean 24-h BP values <130 mmHg. These differences could help to explain the results of several trials in which differences in BP between active therapy and placebo were not accompanied by differences in cardiovascular outcomes.33 The initial BP of the participants in those trials was in the range 140–150 mmHg, but office BP measurements might not have expressed the 'real' BP of these patients. However, the Blood Pressure Lowering Treatment Trialist Collaboration reviewed data from 201,566 patients to determine whether the magnitude of the benefit of reducing BP varies with the clinical BP level.34 The authors concluded that it was “unlikely that the effectiveness of BP-lowering treatments depends substantively upon starting BP levels.”34 The data were supportive of the utilization of BP-lowering regimens in high-risk patients with and without hypertension.
Data obtained over the past 2 years have increased interest in, and highlighted the need of controlling, BP variability (meaning the variability between office visits) and BP instability (that is, transient fluctuations in BP, usually in response to a specific stimulus such as stress or the lack of compliance) in visit-to-visit BP estimation.35,36,37 Different classes of antihypertensive drugs have different effects on the control of long-term BP variability, with calcium-channel blockers (CCBs) seeming to provide the best level of control.38 In summary, threshold and in particular goal BP are enormously important for adequate control of BP, and the use of home or ambulatory BP estimations can help estimating the exact situation of the patient and improve the information obtained through office BP measurements.
Threshold and target BPs
Recommendations in current guidelines
Authors of all guidelines agree that pharmacological treatment of patients with hypertension should be initiated as soon as BP rises >140/90 mmHg.3,4,12 In patients with grade 1 hypertension and low or moderate cardiovascular risk (≤2 risk factors), a period of initial treatment with nonpharmacological measures is recommended, with antihypertensive drug therapy being initiated if this approach fails.3 An exception are patients with high-normal BP and a high global cardiovascular risk owing to the presence of diabetes, chronic kidney disease, or established CVD in whom guidelines recommend the initiation of pharmacological therapy.3,4,12 Nonetheless, in the reappraisal of the ESH guidelines,39 the absence of evidence regarding the outcome of these patients led to the recommendation that such individuals should not be treated pharmacologically unless they have type 2 diabetes and TOD (in particular microalbuminuria or macroalbuminuria).
Is <130/80 mmHg an appropriate BP goal?
Most trials of antihypertensive therapies that have reported clear reductions in major cardiovascular events have included individuals with an initial systolic BP >160 mmHg,40 and only in a few trials was mean systolic BP lowered to <140 mmHg. By contrast, diastolic BP of <90 mmHg for BP was achieved in most trials.41 However, findings from trials showing the advantages of a BP reduction <140/90 mmHg, albeit incomplete, suggest that the return of grade 1–2 BP to 130–139/80–89 mmHg is adequate in patients with hypertension.39 By contrast, data indicate that attaining BP values <120/80 mmHg can be dangerous, as indicated in the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET),42 the International VerapamilSR-Trandolapril (INVEST) study,43 and the Randomized Olmesartan and Diabetes Microalbuminuria Prevention (ROADMAP) study,23 in which cardiovascular death was more prevalent in patients with established coronary artery disease and systolic BP values <120 mmHg. Similarly, strict control to systolic BP values <120 mmHg in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study44 did not reduce the incidence of fatal and nonfatal cardiovascular events in patients with diabetes. These findings could preclude the consideration of a target BP of 130/80 mmHg,3,4 at least in patients with established CVD, and contrast with the beneficial effects of antihypertensive therapy demonstrated in the meta-analysis of studies in normotensive individuals.17 However, in this meta-analysis, cardiovascular mortality was similar in patients receiving antihypertensive drugs for secondary prevention and in untreated controls.
In patients with chronic kidney disease, a low target BP of <130/80 mmHg (or even lower in the presence of proteinuria) is considered appropriate.3,4,12 This target BP has been questioned by results obtained in the extension of the African American Study in Kidney Disease (AASKD) study45 and by data from the ACCORD study,44 in which a target BP <120/80 mmHg was not accompanied by an improvement in renal function. Nonetheless, findings from the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) study46 seem to be in favor of a low BP goal for renal protection. A low BP target was also beneficial in patients with hypertensive kidney disease and proteinuria,45 but the fact that chronic kidney disease and CVD are so closely related makes the separation of cardiovascular and renal BP goals difficult in these patients,39 as a low target BP goal that might be beneficial for the kidney could be deleterious for the coronary arteries.
The possibility that low BP levels are better tolerated by the cerebral circulation than by the coronary circulation is an interesting hypothesis. This concept is supported by data from Thompson and colleauges,17 the ONTARGET42 and ACCORD44 studies, as well as from a 2011 meta-analysis on the effects of intensive BP-reduction in 73,913 patients with diabetes.47 However, the absence of a beneficial effect of telmisartan when compared with placebo, despite a difference in BP between the two groups in the Prevention Regimen for Effectively avoiding Second Strokes (PROFFESS) trial,48 seems to disagree with this hypothesis.
The evidence for the adequacy of BP targets contained in guidelines3,4 in antihypertensive treatment has been reviewed.40 Available data support the reduction of BP to values to <140/90 mmHg, but do not favor a reduction to <130/80 mmHg, in patients with diabetes or a history of CVD, as indicated by most guidelines because of the absence of evidence obtained in prospective studies. The authors of the reappraisal of the ESH guidelines conclude that “on the basis of current data, it may be prudent to recommend lowering [systolic/diastolic BP] to values within the range 130–139/80–85 mmHg, and possibly closer to the lower values in this range, in all hypertensive patients. More critical evidence from specific randomized trials is desirable, however.”39 In summary, the goal BP <130/80 mmHg has been discarded for two reasons: firstly, because no concluding evidence exists that would support it, and, secondly, because a goal BP <130/80 mmHg can be accompanied by an increased risk of cardiac events in patients with established CAD and in whose with diabetes.
How to start treatment
For many years, the initial pharmacological treatment of arterial hypertension was antihypertensive monotherapy, which was then followed by one of two options: either the addition of a second drug, if required, or the switch to another drug, in an attempt to find the appropriate monotherapy for each individual patient (also know as 'sequential therapy'). Administration of a combination of at least two drugs from the start of treatment is recommended in the guidelines,3,4 particularly in patients in whom actual BP and target BP differ by >20 mmHg. This measure facilitates and accelerates the early control of BP,49,50 and contributes to the maintenance of adequate long-term BP control, as shown in the ACCOMPLISH study.51
The drug combination can be either administered in the form of various individual pills or in one pill as a fixed combination, which significantly improves compliance.49 The most-widely used combinations are those containing an RAAS suppressor (such as an angiotensin-converting-enzyme inhibitor or an angiotensin-receptor blocker) and a diuretic. However, the positive cardiovascular and renal outcomes of the ACCOMPLISH study51,52 greatly promoted the combined use of an RAAS suppressor and a CCB. Irrespective of how treatment is begun, clinicians generally agree that rapid initial reduction of BP within the first 3 months of therapy is required to improve cardiovascular outcomes.53,54
A triple combination is needed in ≥30% of patients with hypertension in order to reach the target BP.50 The most-frequently used fixed triads consist of an RAAS suppressor (valsartan or olmesartan), a CCB (amlodipine), and a thiazide diuretic (hydrochlorothiazide).55 The combined effects of the three drugs at optimal doses control BP in a high percentage (>50%) of patients who require triple therapy. Hydrochlorothiazide has been substituted by the more-potent chlorthalidone at similar doses in several studies.56,57,58
Antihypertensive therapy in elderly patients
No trial of elderly patients (>65 years) with initial BP levels between 140–160 mmHg has been performed and, in trials involving elderly patients with initial systolic BP levels of >160 mmHg, systolic BP has never been reduced to <140 mmHg.39 In elderly patients, the systolic BP goal should be <140 mmHg, provided that treatment is conducted with particular attention to adverse responses to antihypertensive mediction.3,40 For patients aged >80 years, the target systolic BP should be <150 mmHg, which reflects the findings of the Hypertension in the Very Elderly Trial (HYVET).59 HYVET was the first prospective trial in patients with hypertension who were >80 years of age (so far, available data were post-hoc meta-analyses of elderly patients who were included in other trials).60 Data of a meta-analysis showed that antihypertensive therapy decreased the incidence of nonfatal cardiovascular events—in particular of stroke—but not cardiovascular death. The results of HYVET indicated that lowering BP to a goal <150 mmHg prevented fatal and nonfatal events. The treatment was initiated with a diuretic (indapamide), and in >80% of patients combined with an angiotensin-converting-enzyme inhibitor (perindopril) to achieve target BP.
Another challenge in the treatment of elderly patients with hypertension is the presence of orthostatic hypotension, which is defined as a decrease >20 mmHg in systolic BP or of >10 mmHg in diastolic BP when a person moves from a supine to a sitting or standing position. Orthostatic hypotension is particularly prevalent in the elderly, occurring in up to 26% of individuals aged >85 years who have hypertension.61 The presence of orthostatic hypotension is a predictor of cardiovascular events,61 precipitates intercurrent complications (such as falls), and requires a reconsideration of antihypertensive treatment in elderly patients.62 The need for a trial in elderly hypertensive individuals with orthostatic hypotension that compares the discontinuation of antihypertensive therapy with continued treatment has been highlighted.63 Elderly patients with hypertension require close medical attention. Antihypertensive therapy should be initiated slowly, using lower doses than usual, which are then slowly titrated up. A combination with other drugs can be required by many patients, as shown in HYVET.59 BP has to be measured sitting and standing to discard orthostatism. As many elderly patients require polymedication because of comorbidities, drug–drug interactions can make it more difficult to achieve compliance and long-term adherence.
Resistant hypertension
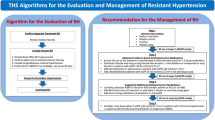
Resistant hypertension is defined as BP (measured at the clinician's office [office BP]) that remains above target levels (<140/90 mmHg) despite the concurrent use of three or more antihypertensive drugs (one of them being a diuretic) at adequate doses. The relevance of this form of hypertension is exemplified by the fact that it conveys the worse prognosis of all the various grades of BP (together with malignant hypertension). The prevalence of resistant hypertension among patients with elevated BP remains unknown, but has been estimated to vary between 20 and 30%.64 Using prospective data, investigators from Spain65 and the USA66 have shown the prevalence of resistant hypertension among patients treated for hypertension to be 12.2% and 12.8%, respectively. In both studies, resistant hypertension was diagnosed on the basis of office BP measurements. However, the additional determination of ambulatory BP in the patients of the Spanish Ambulatory Blood Pressure Monitoring Registry revealed that 37.5% of these patients had white-coat hypertension—in other words, their ambulatory BP values were totally normal.65 Compared with patients who had white-coat hypertension, individuals with resistant hypertension were younger (mean 1 year) and predominantly male, but both groups had a similar BMI. In the US study, patients with resistant hypertension tended to be older, were more-likely of African–American origin, and had a higher BMI than patients with controlled hypertension. In both patient series, resistance to antihypertensive therapy was associated with a worse risk profile than that of patients with controlled hypertension, including more-severe microalbuminuria, reduced renal function, and a history of cardiovascular events.65,66
Findings from various studies have demonstrated improvements in therapy for resistant hypertension, which is particularly difficult to treat. The addition of the aldosterone blocker spironolactone on top of triple therapy has been shown to reduce BP to target levels in up to 50% of patients with resistant hypertension.64,67 Such a good response is, in some cases, ligated to the presence of an undiagnosed primary aldosteronism. The prevalence of primary aldosteronism in patients with resistant hypertension has been estimated to be 14–23%.68 Elevated plasma aldosterone levels directly contribute to the pathogenesis of insulin resistance and endothelial dysfunction—two processes that are, in turn, involved in maladaptive renal and cardiovascular remodeling and promote the development of resistant hypertension.69 In these patients, a rapid reversal of left ventricular hypertrophy and intracardiac volume overload, accompanied by a prominent diuretic effect, have been shown to take place after mineralocorticoid-receptor blockade.70 Besides the possibility of a primary aldosteronism, other causes of secondary hypertension (amply reviewed elsewhere64) have to be excluded in patients who present with resistant hypertension. Of particular relevance are increased sodium intake, the presence of sleep disturbances (for example, obstructive sleep apnea), and the use of drugs that can increase BP, such as NSAIDs.
Beyond pharmacological therapy, two new forms of treatment for patients with resistant hypertension are being developed. During catheter-based bilateral renal denervation,71 a catheter is advanced into the renal artery, connected to a radiofrequency generator, and 4–6 radiofrequency treatments applied are over the length of the two arteries. This technique has yielded excellent results that lasted for a minimum of 2 years and were accompanied by a substantial improvement in insulin resistance.72 Chronic electrical stimulation of the carotid baroreflex, by means of a surgically located device in the neck, has also shown promising results.73
Adherence and clinical inertia
Daily compliance and long-term adherence to treatment are the most-important objectives of therapy in hypertensive patients,3,4,12 given that many patients abandon therapy after a few months or years. Unlike statins and antidiabetic therapy, abandoning antihypertensive therapy is not accompanied by any legacy effects,74 indicating that the cardiovascular risk conferred by hypertension is recovered rapidly if therapy is interrupted. Box 3 contains the most-important recommendations to improve long-term adherence to treatment of patients with hypertension. Ideally, a close relationship between doctor, nurse, and patient has to be maintained for the rest of the patient's life. Self measurement of BP at home enhances the patient's responsibility for their own treatment and is, therefore, of great value in improving patient compliance and maintaining long-term adherence to antihypertensive medication.75 A continuous dialog between the doctor, the patient, and their family will also facilitate control of BP and accompanying cardiovascular risk factors,3,4,12 while precluding 'clinical inertia' (meaning that appropriate action is not taken) on the side of the doctor.76
Good long-term adherence to antihypertensive medication is important for the outcome of patients with hypertension. This issue was highlighted in a study that included data from 18,806 newly diagnosed patients with hypertension and no evidence of CVD.77 Patients who adhered to treatment on ≥80% of days showed a significant decrease in the risk of cardiovascular events compared with those who did not adhere to the same extent (HR 0.62; 95% CI 0.40–0.96; P = 0.032). Early initiation of antihypertensive treatment and adherence to therapy thus provide major benefits for patients.
Confirming that patients are taking their medication on a regular basis is particularly important in cases of resistant hypertension. Findings from studies with small numbers of participants suggest that poor adherence could contribute to the high prevalence of resistant hypertension. Among patients taking multidrug regimens for resistant hypertension, but whose BP remained uncontrolled, target BPs were achieved when the same drugs were administered by clinical staff.78 Another example of the relevance of adherence is the capability of maintaining a low-sodium intake to control BP in patients with resistant hypertension. This simple intervention can decrease systolic BP and diastolic BP by 22.7 and 9.1 mmHg, respectively.79
Conclusions
Many important decisions in hypertension management are taken without the support of evidence from large, randomized controlled trials.3 As a consequence, further studies are needed, particularly trials comparing the effectiveness of life-style changes and of antihypertensive drug therapy in patients with grade 1 hypertension (Box 4). Drug-based trials need to include elderly patients with grade 1 hypertension and patients with high-normal BP levels at baseline. The need to attain a target BP <130/80 mmHg to prevent future cardiovascular events and death in patients without established CVD should also be investigated.
The problem with these new trials is the high number of patients required and, as a consequence, the high cost that will complicate their execution. Personally, I believe that all of these trials will prevent cardiovascular events—but will the number of cardiovascular events and deaths prevented be high enough to make these trials cost-effective? In other words, would the number of patients needed to treat to prevent one single cardiovascular event be adequate, allowing the wide use of the tested treatment in daily clinical practice? Alternatively, would many patients have to be treated to prevent one single event, rendering the cost of the intervention unsustainable?
Future studies must also contemplate the simultaneous evolution of CVD and renal disease, as done in the ACCORD,44 ADVANCE,46,80 and Avoiding Cardiovascular Events in Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) studies.51,52 Investigation of this issue will improve our knowledge of how the treatment of arterial hypertension and its associated risk factors affects the interlinked development of cardiovascular and renal problems. The results of the ADVANCE46,80 and ACCOMPLISH51,52 studies have shown that the same medication improved both cardiovascular51,80 and renal46,52 outcomes.
Key to the successful clinical management of hypertension is attaining the best BP control among patients with hypertension after having adequately established that BP is elevated and whether other cardiovascular risk factors exist. The long-term benefits of an adequate management of hypertension in a given patient are determined by the stage of cardiovascular and renal disease when treatment is initiated and on the basis of the adequacy of the simultaneous control of other coexisting cardiovascular risk factors. Although office BP measurement will remain the most-widely used method for assessing patients in the foreseeable future, ambulatory BP monitoring and home BP measurement can replace office BP readings when available.
The development of novel therapeutic targets for hypertension is needed.81 Novel pharmacological approaches are targeted towards treating resistant hypertension, improving BP control, and reducing cardiovascular risk beyond that achieved by BP-lowering alone. Modulation of the RAAS provides the rationale for current antihypertensive therapies and new RAAS blockers with a higher efficacy and effectiveness than established drugs will soon be available.82,83
Review criteria
A search of online database including MEDLINE for articles published in English and between 1990 and June 2011 has been performed using the keywords “hypertension”, “blood pressure”, “prehypertension”, “antihypertensive agents”, and “CV disease”. Most references have been published between 2005 and 2011, with the exception of selected old references about specific challenges in therapeutic management of patients with hypertension.
References
Lawes, C. M., Vander Hoorn, S., Rodgers, A. & International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 371, 1513–1518 (2008).
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective Studies. Lancet 360, 1903–1913 (2002).
Mancia, G. et al. 2007 guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and calcium-channel blocker f the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Chobanian, A. V. et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension 42, 1206–1252 (2003).
Collins, R. et al. Blood pressure, stroke and coronary heart disease. Part 2: Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 335, 827–838 (1990).
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA 265, 3255–3264 (1991).
Sacks, F. M. et al. Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH): a multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann. Epidemiol. 5, 108–118 (1995).
Appel, L. J. et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 336, 1117–1124 (1997).
Kastorini, C. M. et al. The effect of the Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 57, 1299–1313 (2011).
De Lorgeril, M. et al. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications alter myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 99, 779–785 (1999).
He, F. J. & MacGregor, G. A. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet 378, 380–382 (2011).
Williams, B. et al. The BHS guidelines working party, for the British Hypertension Society guidelines for hypertension Management, 2004–BHS IV. BMJ 328, 634–640 (2004).
Vasan, R. S., Larson, M. G., Leip, E. P., Kannel, W. B. & Levy, D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 358, 1682–1686 (2001).
Vasan, R. S. et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl. J. Med. 345, 1291–1297 (2001).
Julius, S. et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N. Engl. J. Med. 354, 1685–1697 (2006).
Lüders, S. et al. The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: a prospective, randomized controlled prevention trial of the German Hypertension League. J. Hypertens. 26, 1487–1496 (2008).
Thompson, A. M. et al. Antihypertensive treatment and secondary prevention of cardiovascular disease events among persons without hypertension. A meta-analysis. JAMA 305, 913–922 (2011).
Ventura, H. O. & Lavie, C. J. Antihypertensive therapy for prehypertension. Relationship with cardiovascular outcomes. JAMA 305, 940–941 (2011).
Dzau, V. J. & Braunwald, E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshops consensus statement. Am. Heart J. 121, 1244–1263 (1991).
Dzau, V. J. et al. The cardiovascular disease continuum validated: clinical evidence of improved patient outcomes: part I: pathophysiology and clinical trial evidence (risk factors through stable coronary disease). Circulation 114, 2850–2870 (2006).
Dzau, V. J. et al. The cardiovascular disease continuum validated: clinical evidence of improved patient outcomes: part II: clinical trial evidence (acute coronary syndrome through renal disease) and future directions. Circulation 114, 2871–2891 (2006).
Ruggenenti, P. et al. Preventing microalbuminuria in type 2 diabetes. N. Engl. J. Med. 351, 1941–1951 (2004).
Haller, H. et al. Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N. Engl. J. Med. 364, 907–917 (2011).
Ruggenenti, P. et al. Preventing left ventricular hypertrophy by ACE inhibition in hypertensive patients with type 2 diabetes: a prespecified analysis of the Bergamo Nephrologic Diabetes Complications Trial (BENEDICT). Diabetes Care 31, 1629–1634 (2008).
Sehestedt, T. et al. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur. Heart J. 31, 883–891 (2010).
Ibsen, H. et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients with left ventricular hypertrophy and diabetes. J. Nephrol. 21, 566–569 (2008).
Schmieder R. et al. Changes in albuminuria predict mortality and morbidity in patients with cardiovascular disease. J. Am. Soc. Nephrol. 22, 1353–1364 (2011).
Wachtell, K. et al. Regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy and reduction in sudden cardiac death. Circulation 116, 700–705 (2007).
Verdecchia, P. et al. Effects of telmisartan, ramipril, and their combination on left ventricular hypertrophy in individuals at high vascular risk in the Ongoing Telmisartan Alone and in Combination With Ramipril Global End Point Trial and the Telmisartan Randomized Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease. Circulation 120, 1380–1389 (2009).
Yusuf, S. & Pitt, B. A lifetime of prevention: the case of heart failure. Circulation 106, 2997–2998 (2002).
Ruilope, L. M. & Bakris, G. L. Renal function and target organ damage in hypertension. Eur. Heart J. 32, 1599–1604 (2011).
Banegas, J. R. et al. Discrepancies between office and ambulatory blood pressure: clinical implications. Am. J. Med. 122, 1136–1141 (2009).
Zanchetti, A. et al. Facts and fallacies of blood pressure control in recent trials: implications in the management of patients with hypertension. J. Hypertens. 27, 673–679 (2009).
Czernichow, S. et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J. Hypertens. 29, 4–16 (2011).
Mancia, G. Prognostic value of long-term blood pressure variability. The evidence is growing. Hypertension 57, 141–143 (2011).
Rothwell, P. M. et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 375, 895–905 (2010).
Muntner, P. et al. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population. Findings from NHANES III, 1988 to 1994. Hypertension 57, 160–166 (2011).
Webb, A. J., Fischer, U., Mehta, Z. & Rothwell, P. M. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 375, 906–915 (2010).
Mancia, G. et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J. Hypertens. 27, 2121–2158 (2009).
Zanchetti, A., Grassi, G. & Mancia, G. When should antihypertensive drug treatment be initiated and to what levels should systolic blood pressure be lowered? A critical reappraisal. J. Hypertens. 27, 923–934 (2009).
Mancia, G. & Grassi, G. Management of essential hypertension. Br. Med. Bull. 94, 189–199 (2010).
Sleight, P. et al. Prognostic value of blood pressure in patients at high risk of vascular events in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J. Hypertens. 27, 1360–1369 (2009).
Cooper-DeHoff, R. M. et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 304, 61–68 (2010).
ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 362, 1575–1585 (2010).
Appel, L. J. et al. Intensive blood pressure control in hypertensive chronic kidney disease. N. Engl. J. Med. 363, 918–929 (2010).
De Galan, B. E. et al. Lowering blood pressure reduces renal events in type 2 diabetes. J. Am. Soc. Nephrol. 20, 883–892 (2009).
Reboldi, G. et al. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J. Hypertens. 29, 1253–1269 (2011).
Yusuf, S. et al. Telmisartan to prevent recurrent stroke and cardiovascular events. N. Engl. J. Med. 359, 1225–1237 (2008).
Gupta, A. K., Arshad, S. & Poulter, N. R. Compliance, safety, and effectiveness of fixed dose combinations of antihypertensive agents. Hypertension 55, 399–407 (2010).
Ruilope, L. M. & Bakris, G. L. in Therapeutic strategies in hypertension (Ed. Bakris, G. L.) 1–8 (Clinical Publishing, Oxford, 2006).
Jamerson, K. et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high risk patients. N. Engl. J. Med. 359, 2417–2418 (2008).
Bakris, G. et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet 375, 1173–1181 (2010).
Basile, J. The importance of prompt blood pressure control. J. Clin. Hypertens. (Greenwich) 10, 13–19 (2008).
Berlowitz, D. R. & Franklin, S. The clock is ticking: the case for achieving more rapid control of hypertension. J. Clin. Hypertens. (Greenwich) 12, 323–327 (2010).
Deeks, E. D. Olmesartan medoxomil/amlodipine/hydrochlorothiazide: fixed dose combination in hypertension. Drugs 71, 209–220 (2011).
Messerli, F. H. et al. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring. A meta-analysis of randomized trials. J. Am. Coll. Cardiol. 57, 590–600 (2011).
Pitt, B. The role of chlorthalidone in patients with high risk hypertension. J. Clin. Hypertens. (Greenwich) 11, 460–461 (2009).
Dorsch, M. P., Gillespie, B. W., Erickson, S. R., Bleske, B. E. & Weder, A. B. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide. A retrospective cohort analysis. Hypertension 57, 689–694 (2011).
Beckett, N. S. et al. Treatment of hypertension in patients 80 years of age or older. N. Engl. J. Med. 358, 1887–1898 (2008).
Gueyffiert, F. et al. Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDAN Group. Lancet 353, 793–796 (1999).
Rutan, G. H. et al. Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 19, 508–519 (1992).
Robertson, D. Orthostatic hypertension. The last hemodynamic frontier. Hypertension 57, 158–159 (2011).
Campese, V. & Schneider, E. L. Reevaluating the use of antihypertensive medications, a first step toward reducing polypharmacy in very old patients. J. Clin. Hypertens. (Greenwich) 12, 621–624 (2010).
Calhoun, D. A. et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 51, 1403–1419 (2008).
De la Sierra, A. et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 57, 898–902 (2011).
Persell, S. D. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 57, 1076–1080 (2011).
de Souza, F., Muxfeldt, E., Fiszman, R. & Salles, G. Efficacy of spironolactone therapy in patients with true resistant hypertension. Hypertension 55, 147–152 (2010).
Acelajado, M. C. & Calhoun, D. A. Aldosteronism and resistant hypertension. Int. J. Hypertens. 2011, 837817 (2011).
Sowers, J. R., Whaley-Connell, A. & Epstein, M. Narrative review: the emerging clinical implications of the role of aldosterone in the metabolic syndrome and resistant hypertension. Ann. Intern. Med. 150, 776–783 (2009).
Gaddam, K. et al. Rapid reversal of left ventricular hypertrophy and intracardiac volume overload in patients with resistant hypertension and hyperaldosteronism: a prospective clinical study. Hypertension 56, e26 (2010).
Simplicity HTN-2 Investigators. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 376, 1903–1909 (2010).
Mahfoud, F. et al. Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension. Circulation 123, 1940–1946 (2011).
Wustmannn, K. et al. Effects of chronic baroreceptor stimulation on the autonomic cardiovascular regulation in patients with drug resistant arterial hypertension. Hypertension 54, 530–536 (2009).
Holman, R. R., Paul, S. K., Bethel, M. A., Neil, H. A. & Matthews, D. R. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N. Engl. J. Med. 359, 1565–1576 (2008).
Agarwal, R., Bills, J. E., Hecht, T. J. & Light, R. P. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension 57, 29–38 (2011).
Phillips, L. S. et al. Clinical inertia. Ann. Intern. Med. 135, 825–834 (2001).
Mazzaglia, G. et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 120, 1598–1605 (2009).
Bunker, J., Callister, W., Chang, C. L. & Sever, P. S. How common is true resistant hypertension. J. Hum. Hypertens. 25, 137–140 (2011).
Pimenta, E. et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension. Results from a randomized trial. Hypertension 54, 475–481 (2009).
Patel, A. et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitas (the ADVANCE trial): a randomised controllled trial. Lancet 370, 829–840 (2007).
Paulis, L. & Unger, T. Novel therapeutic targets for hypertension. Nat. Rev. Cardiol. 7, 431–441 (2010).
Ruilope, L. M. et al. Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet 375, 1255–1266 (2010).
White, W. B. et al. Effects of the angiotensin receptor blocker azilsartan medoxomil versus olmesartan and valsartan on ambulatory and clinic blood pressure in patients with stages 1 and 2 hypertension. Hypertension 57, 413–420 (2011).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Ruilope, L. Current challenges in the clinical management of hypertension. Nat Rev Cardiol 9, 267–275 (2012). https://doi.org/10.1038/nrcardio.2011.157
Published:
Issue date:
DOI: https://doi.org/10.1038/nrcardio.2011.157
This article is cited by
-
Traditional Chinese medicine suppresses left ventricular hypertrophy by targeting extracellular signal-regulated kinases signaling pathway in spontaneously hypertensive rats
Scientific Reports (2017)
-
Sacubitril/valsartan in the treatment of arterial hypertension: an unaccomplished promise?
Hypertension Research (2017)
-
General practice and ethnicity: an experimental study of doctoring
BMC Family Practice (2014)
-
Physician Underutilization of Effective Medications for Resistant Hypertension at Office Visits in the United States: NAMCS 2006–2010
Journal of General Internal Medicine (2014)
-
Olmesartan vs. Ramipril in Elderly Hypertensive Patients: Review of Data from Two Published Randomized, Double-Blind Studies
High Blood Pressure & Cardiovascular Prevention (2014)