Key Points
-
The urogenital tract is a complex environment composed of many different types of epithelial tissues and innate immune cells that sample the surrounding milieu. As a host-adapted organism, Neisseria gonorrhoeae can interact with only human forms of many molecules. Moreover, owing to environmental heterogeneities as well as unknown concentrations of oxygen and nutrients in this niche, substantial challenges exist for developing tissue culture and animal models. Advances in standardizing the cell culture techniques of primary tissue culture and transgenic mouse models may help to ameliorate these challenges.
-
Although the prevailing view is that infections in women are mainly asymptomatic whereas infections in men are not, many studies show that asymptomatic infections are prevalent in both sexes. The observations underlying the current dogma likely come from physiological and anatomical differences in the male and female urogenital tracts, making neutrophil influx in men much more noticeable and easier to diagnose than infections in women.
-
N. gonorrhoeae is an obligate human pathogen with the ability to evade and modulate both the innate and adaptive immune systems to benefit its replication and survival. The host-restricted pathogen has subsequently evolved a moderately small but effective set of regulatory mechanisms to quickly adapt to changing oxygen and nutrient concentrations.
-
As N. gonorrhoeae progresses through the stages of disease pathogenesis (transmission, adherence, colonization and invasion, and immune evasion), the bacterium expresses many virulence factors to promote survival and replication while remaining minimally invasive and minimally discoverable by immune cells. It has yet to be settled in the field whether the vast neutrophil influx following symptomatic infection benefits the host or the pathogen.
-
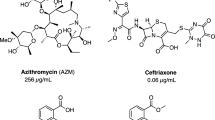
Owing to its natural competence, propensity for horizontal gene transfer, efficient transformation and dynamic and variable genome, N. gonorrhoeae is rapidly developing resistance to every major class of antibiotic. With worldwide antimicrobial resistance on the rise, it is necessary to understand the mechanisms by which resistance determinants confer resistance and to develop novel therapies to avoid an era of untreatable gonorrhoea.
-
The Neisseria genus is composed of many commensals and one other pathogen, Neisseria meningitidis, that are closely related to N. gonorrhoeae genetically but are phenotypically distinct and occupy different niches. Owing to this similarity, it is often difficult to determine which factors are specific virulence factors for N. gonorrhoeae and which facilitate colonization. More research is needed to determine which factors confer pathogenicity and differentiate between these two pathogens.
Abstract
The host-adapted human pathogen Neisseria gonorrhoeae is the causative agent of gonorrhoea. Consistent with its proposed evolution from an ancestral commensal bacterium, N. gonorrhoeae has retained features that are common in commensals, but it has also developed unique features that are crucial to its pathogenesis. The continued worldwide incidence of gonorrhoeal infection, coupled with the rising resistance to antimicrobials and the difficulties in controlling the disease in developing countries, highlights the need to better understand the molecular basis of N. gonorrhoeae infection. This knowledge will facilitate disease prevention, surveillance and control, improve diagnostics and may help to facilitate the development of effective vaccines or new therapeutics. In this Review, we discuss sex-related symptomatic gonorrhoeal disease and provide an overview of the bacterial factors that are important for the different stages of pathogenesis, including transmission, colonization and immune evasion, and we discuss the problem of antibiotic resistance.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
World Health Organization. WHO Guidelines for the Treatment of Neisseria gonorrhoeae (WHO, 2016).
Carmona-Gutierrez, D., Kainz, K. & Madeo, F. Sexually transmitted infections: old foes on the rise. Microb. Cell 3, 361–362 (2016).
Unemo, M. et al. The novel 2016 WHO Neisseria gonorrhoeae reference strains for global quality assurance of laboratory investigations: phenotypic, genetic and reference genome characterization. J. Antimicrob. Chemother. 71, 3096–3108 (2016).
Newman, L. et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLOS ONE 10, e0143304 (2015).
Lee, J. S., Choi, H. Y., Lee, J. E., Lee, S. H. & Oum, B. S. Gonococcal keratoconjunctivitis in adults. Eye 16, 646–649 (2002).
Noble, R. C., Cooper, R. M. & Miller, B. R. Pharyngeal colonisation by Neisseria gonorrhoeae and Neisseria meningitidis in black and white patients attending a venereal disease clinic. Br. J. Vener. Dis. 55, 14–19 (1979).
Danby, C. S. et al. Patterns of extragenital chlamydia and gonorrhea in women and men who have sex with men reporting a history of receptive anal intercourse. Sex. Transm. Dis. 43, 105–109 (2016).
Little, J. W. Gonorrhea: update. Oral Surg., Oral Med., Oral Pathol., Oral Radiol., Endodont. 101, 137–143 (2006).
Sandstrom, I. Etiology and diagnosis of neonatal conjunctivitis. Acta Paediatr. Scand. 76, 221–227 (1987).
Masi, A. T. & Eisenstein, B. I. Disseminated gonococcal infection (DGI) and gonococcal arthritis (GCA): II. Clinical manifestations, diagnosis, complications, treatment, and prevention. Semin. Arthritis Rheum. 10, 173–197 (1981).
Hoffman, O. & Weber, R. J. Pathophysiology and treatment of bacterial meningitis. Ther. Adv. Neurol. Disord. 2, 1–7 (2009).
Marri, P. R. et al. Genome sequencing reveals widespread virulence gene exchange among human Neisseria species. PLOS ONE 5, e11835 (2010).
Liu, G., Tang, C. M. & Exley, R. M. Non-pathogenic Neisseria: members of an abundant, multi-habitat, diverse genus. Microbiology 161, 1297–1312 (2015).
Maiden, M. C. & Harrison, O. B. Population and functional genomics of Neisseria revealed with gene-by-gene approaches. J. Clin. Microbiol. 54, 1949–1955 (2016).
Bratcher, H. B., Corton, C., Jolley, K. A., Parkhill, J. & Maiden, M. C. A gene-by-gene population genomics platform: de novo assembly, annotation and genealogical analysis of 108 representative Neisseria meningitidis genomes. BMC Genomics 15, 1138 (2014).
Joseph, B. et al. Virulence evolution of the human pathogen Neisseria meningitidis by recombination in the core and accessory genome. PLOS ONE 6, e18441 (2011).
Maiden, M. C. Population genomics: diversity and virulence in the Neisseria. Curr. Opin. Microbiol. 11, 467–471 (2008).
Edwards, J. L. & Apicella, M. A. The molecular mechanisms used by Neisseria gonorrhoeae to initiate infection differ between men and women. Clin. Microbiol. Rev. 17, 965–981 (2004).
Sparling, P. F. Biology of Neisseria gonorrhoeae. 3rd edn (McGraw-Hill, 1999).
Walker, C. K. & Sweet, R. L. Gonorrhea infection in women: prevalence, effects, screening, and management. Int. J. Women' Health 3, 197–206 (2011).
Jordan, S. J., Schwebke, J. R., Aaron, K. J., Van Der Pol, B. & Hook, E. W. 3rd. Meatal swabs contain less cellular material and are associated with a decrease in Gram stain smear quality compared to urethral swabs in men. J. Clin. Microbiol. 55, 2249–2254 (2017).
Muzny, C. A. et al. Sexually transmitted infection risk among women is not fully explained by partner numbers. South Med. J. 110, 161–167 (2017).
Grimley, D. M. et al. Sexually transmitted infections among urban shelter clients. Sex. Transm. Dis. 33, 666–669 (2006).
Geisler, W. M., Yu, S. & Hook, E. W. 3rd. Chlamydial and gonococcal infection in men without polymorphonuclear leukocytes on gram stain: implications for diagnostic approach and management. Sex. Transm. Dis. 32, 630–634 (2005).
Xiong, M. et al. Analysis of the sex ratio of reported gonorrhoea incidence in Shenzhen, China. BMJ Open 6, e009629 (2016). This epidemiological study of 1,106 male and 1,420 female participants in Shenzhen, China, shows that undiagnosed, unreported gonorrhoea infections were common in both men and women and that the reported incidence sex ratio was overestimated by a factor of 7.9.
Hook, E. W. 3rd. Gender differences in risk for sexually transmitted diseases. Am. J. Med. Sci. 343, 10–11 (2012).
Hedges, S. R. et al. Limited local and systemic antibody responses to Neisseria gonorrhoeae during uncomplicated genital infections. Infect. Immun. 67, 3937–3946 (1999).
Fichorova, R. N., Desai, P. J., Gibson, F. C. 3rd & Genco, C. A. Distinct proinflammatory host responses to Neisseria gonorrhoeae infection in immortalized human cervical and vaginal epithelial cells. Infect. Immun. 69, 5840–5848 (2001).
Papp, J. R., Schachter, J., Gaydos, C. A. & Van Der Pol, B. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae — 2014. MMWR Morb. Mortal. Wkly Rep. 63, 1–19 (2014).
James-Holmquest, A. N., Swanson, J., Buchanan, T. M., Wende, R. D. & Williams, R. P. Differential attachment by piliated and nonpiliated Neisseria gonorrhoeae to human sperm. Infect. Immun. 9, 897–902 (1974).
Harvey, H. A. et al. Gonococcal lipooligosaccharide is a ligand for the asialoglycoprotein receptor on human sperm. Mol. Microbiol. 36, 1059–1070 (2000). This study shows that gonococcal LOS binds to asialoglycoprotein receptor 1 (ASGPR1) on human sperm, possibly contributing to male-to-female transmission.
Cohen, M. S. et al. Human experimentation with Neisseria gonorrhoeae: rationale, methods, and implications for the biology of infection and vaccine development. J. Infect. Dis. 169, 532–537 (1994).
Ketterer, M. R. et al. Desialylation of Neisseria gonorrhoeae Lipooligosaccharide by Cervicovaginal Microbiome Sialidases: The Potential for Enhancing Infectivity in Men. J. Infect. Dis. 214, 1621–1628 (2016).
Higashi, D. L. et al. Dynamics of Neisseria gonorrhoeae attachment: microcolony development, cortical plaque formation, and cytoprotection. Infect. Immun. 75, 4743–4753 (2007).
Craig, L., Pique, M. E. & Tainer, J. A. Type IV pilus structure and bacterial pathogenicity. Nat. Rev. Microbiol. 2, 363–378 (2004).
Obergfell, K. P. & Seifert, H. S. The pilin N-terminal domain maintains Neisseria gonorrhoeae transformation competence during pilus phase variation. PLOS Genet. 12, e1006069 (2016).
Berry, J.-L. & Pelicic, V. Exceptionally widespread nanomachines composed of type IV pilins: the prokaryotic Swiss Army knives. FEMS Microbiol. Rev. 39, 134–154 (2015).
Cahoon, L. A. & Seifert, H. S. Transcription of a cis-acting, noncoding, small RNA is required for pilin antigenic variation in Neisseria gonorrhoeae. PLOS Pathog. 9, e1003074 (2013). This study demonstrates that transcription of a small, cis -acting, non-coding RNA initiates within the guanine quartet (G4) coding sequence enables the formation of the G4 structure required for pilin antigenic variation.
Dietrich, M. et al. Activation of NF-kappaB by Neisseria gonorrhoeae is associated with microcolony formation and type IV pilus retraction. Cell. Microbiol. 13, 1168–1182 (2011).
Swanson, J., Barrera, O., Sola, J. & Boslego, J. Expression of outer membrane protein II by gonococci in experimental gonorrhea. J. Exp. Med. 168, 2121–2129 (1988).
Jerse, A. E. et al. Multiple gonococcal opacity proteins are expressed during experimental urethral infection in the male. J. Exp. Med. 179, 911–920 (1994). This study shows that when Opa-less variants of N. gonorrhoeae strain FA1090 were inoculated into human male volunteers, a majority of bacteria cultured from the infected subjects were Opa-positive and expressed a variety of Opa variants.
Virji, M., Makepeace, K., Ferguson, D. J. & Watt, S. M. Carcinoembryonic antigens (CD66) on epithelial cells and neutrophils are receptors for Opa proteins of pathogenic neisseriae. Mol. Microbiol. 22, 941–950 (1996).
Simms, A. N. & Jerse, A. E. In vivo selection for Neisseria gonorrhoeae opacity protein expression in the absence of human carcinoembryonic antigen cell adhesion molecules. Infect. Immun. 74, 2965–2974 (2006).
Lambden, P. R., Heckels, J. E., James, L. T. & Watt, P. J. Variations in surface protein composition associated with virulence properties in opacity types of Neisseria gonorrhoeae. J. Gen. Microbiol. 114, 305–312 (1979).
Stern, A., Brown, M., Nickel, P. & Meyer, T. F. Opacity genes in Neisseria gonorrhoeae: control of phase and antigenic variation. Cell 47, 61–71 (1986).
Swanson, J. et al. Gonococcal pilin variants in experimental gonorrhea. J. Exp. Med. 165, 1344–1357 (1987).
James, J. F. & Swanson, J. Studies on gonococcus infection. XIII. Occurrence of color/opacity colonial variants in clinical cultures. Infect. Immun. 19, 332–340 (1978).
Seifert, H. S., Wright, C. J., Jerse, A. E., Cohen, M. S. & Cannon, J. G. Multiple gonococcal pilin antigenic variants are produced during experimental human infections. J. Clin. Invest. 93, 2744–2749 (1994).
Anderson, M. T., Byerly, L., Apicella, M. A. & Seifert, H. S. Seminal plasma promotes Neisseria gonorrhoeae aggregation and biofilm formation. J. Bacteriol. 198, 2228–2235 (2016).
Steichen, C. T., Cho, C., Shao, J. Q. & Apicella, M. A. The Neisseria gonorrhoeae biofilm matrix contains DNA, and an endogenous nuclease controls its incorporation. Infect. Immun. 79, 1504–1511 (2011).
Greiner, L. L. et al. Biofilm Formation by Neisseria gonorrhoeae. Infect. Immun. 73, 1964–1970 (2005).
Steichen, C. T., Shao, J. Q., Ketterer, M. R. & Apicella, M. A. Gonococcal cervicitis: a role for biofilm in pathogenesis. J. Infect. Dis. 198, 1856–1861 (2008).
Wetzler, L. M., Blake, M. S., Barry, K. & Gotschlich, E. C. Gonococcal porin vaccine evaluation: comparison of Por proteosomes, liposomes, and blebs isolated from rmp deletion mutants. J. Infect. Dis. 166, 551–555 (1992).
Song, W., Ma, L., Chen, R. & Stein, D. C. Role of lipooligosaccharide in Opa-independent invasion of Neisseria gonorrhoeae into human epithelial cells. J. Exp. Med. 191, 949–960 (2000).
van Vliet, S. J. et al. Variation of Neisseria gonorrhoeae lipooligosaccharide directs dendritic cell-induced T helper responses. PLOS Pathog. 5, e1000625 (2009).
Wetzler, L. M., Barry, K., Blake, M. S. & Gotschlich, E. C. Gonococcal lipooligosaccharide sialylation prevents complement-dependent killing by immune sera. Infect. Immun. 60, 39–43 (1992). This study shows that sialylation of gonococcal LOS prevents opsonophagocytosis by immune sera, which led to the later confirmation that sialylation of LOS prevents complement activation and killing.
Kellogg, D. S. et al. Neisseria gonorrhoeae. I. Virulence genetically linked to clonial variation. J. Bacteriol. 85, 1274–1279 (1963).
Spence, J. M., Wright, L. & Clark, V. L. Laboratory maintenance of Neisseria gonorrhoeae. Curr. Protoc. Microbiol., Unit 4A (2008). This study compares selectively passaged, piliated N. gonorrhoeae capable of infecting human volunteers with non-selectively passaged, non-piliated clonal variants that became non-infectious, enabling researchers to realize that infectivity can be phenotypically followed by observing piliated and non-piliated colony morphology.
Platt, D. J. Carbon dioxide requirement of Neisseria gonorrhoeae growing on a solid medium. J. Clin. Microbiol. 4, 129–132 (1976).
St Amant, D. C., Valentin-Bon, I. E. & Jerse, A. E. Inhibition of Neisseria gonorrhoeae by Lactobacillus species that are commonly isolated from the female genital tract. Infect. Immun. 70, 7169–7171 (2002).
Spurbeck, R. R. & Arvidson, C. G. Inhibition of Neisseria gonorrhoeae epithelial cell interactions by vaginal Lactobacillus species. Infect. Immun. 76, 3124–3130 (2008).
Spurbeck, R. R. & Arvidson, C. G. Lactobacillus jensenii surface-associated proteins inhibit Neisseria gonorrhoeae adherence to epithelial cells. Infect. Immun. 78, 3103–3111 (2010).
Cassat, J. E. & Skaar, E. P. Iron in infection and immunity. Cell Host Microbe 13, 509–519 (2013).
Doherty, C. P. Host-pathogen interactions: the role of iron. J. Nutr. 137, 1341–1344 (2007).
Bonnah, R. A. & Schryvers, A. B. Preparation and characterization of Neisseria meningitidis mutants deficient in production of the human lactoferrin-binding proteins LbpA and LbpB. J. Bacteriol. 180, 3080–3090 (1998).
Noinaj, N., Buchanan, S. K. & Cornelissen, C. N. The transferrin-iron import system from pathogenic Neisseria species. Mol. Microbiol. 86, 246–257 (2012).
Evans, R. W. & Oakhill, J. S. Transferrin-mediated iron acquisition by pathogenic Neisseria. Biochem. Soc. Trans. 30, 705–707 (2002).
Kehl-Fie, T. E. & Skaar, E. P. Nutritional immunity beyond iron: a role for manganese and zinc. Curr. Opin. Chem. Biol. 14, 218–224 (2010).
Ovcinnikov, N. M. & Delektorskij, V. V. Electron microscope studies of gonococci in the urethral secretions of patients with gonorrhoea. Br. J. Vener. Dis. 47, 419–439 (1971).
Farzadegan, H. & Roth, I. L. Scanning electron microscopy and freeze-etching of gonorrhoeal urethral exudate. Br. J. Vener. Dis. 51, 83–91 (1975).
Evans, B. A. Ultrastructural study of cervical gonorrhea. J. Infect. Dis. 136, 248–255 (1977).
King, G., James, J. F. & Swanson, J. Studies on gonococcus infection. XI. Comparison of in vivo and vitro association of Neisseria gonorrhoeae with human neutrophils. J. Infect. Dis. 137, 38–43 (1978).
Apicella, M. A. et al. The pathogenesis of gonococcal urethritis in men: confocal and immunoelectron microscopic analysis of urethral exudates from men infected with Neisseria gonorrhoeae. J. Infect. Dis. 173, 636–646 (1996).
Criss, A. K. & Seifert, H. S. A bacterial siren song: intimate interactions between Neisseria and neutrophils. Nat. Rev. Microbiol. 10, 178–190 (2012).
Lucas, C. E., Hagman, K. E., Levin, J. C., Stein, D. C. & Shafer, W. M. Importance of lipooligosaccharide structure in determining gonococcal resistance to hydrophobic antimicrobial agents resulting from the mtr efflux system. Mol. Microbiol. 16, 1001–1009 (1995).
Zalucki, Y. M., Dhulipala, V. & Shafer, W. M. Dueling regulatory properties of a transcriptional activator (MtrA) and repressor (MtrR) that control efflux pump gene expression in Neisseria gonorrhoeae. mBio 3, e00446-12 (2012). This study compares the binding affinities and regulatory competition between MtrC–MtrD–MtrE efflux pump operon activator MtrA and repressor MtrR, building on previous data characterizing this important antimicrobial resistance pump and its transcriptional regulation.
Thaler, C. J., Vanderpuye, O. A., McIntyre, J. A. & Faulk, W. P. Lactoferrin binding molecules in human seminal plasma. Biol. Reprod. 43, 712–717 (1990).
Mercante, A. D. et al. MpeR regulates the mtr efflux locus in Neisseria gonorrhoeae and modulates antimicrobial resistance by an iron-responsive mechanism. Antimicrob. Agents Chemother. 56, 1491–1501 (2012).
Laskos, L., Ryan, C. S., Fyfe, J. A. & Davies, J. K. The RpoH-mediated stress response in Neisseria gonorrhoeae is regulated at the level of activity. J. Bacteriol. 186, 8443–8452 (2004).
Householder, T. C., Belli, W. A., Lissenden, S., Cole, J. A. & Clark, V. L. cis- and trans- acting elements involved in the regulation of aniA, the gene encoding the major anaerobically induced outer membrane protein in Nesseria gonorrhoeae. J. Bacteriol. 181, 5411–5551 (1999).
Mellies, J., Rudel, T. & Meyer, T. F. Transcriptional regulation of pilC2 in Neisseria gonorrhoeae: response to oxygen availability and evidence for growth-phase regulation in Escherichia coli. Mol. Gen. Genet. 255, 285–293 (1997).
Whitehead, R. N. et al. The small FNR regulon of Neisseria gonorrhoeae: comparison with the larger Escherichia coli FNR regulon and interaction with the NarQ-NarP regulon. BMC Genomics 8, 35 (2007).
Berish, S. A., Subbarao, S., Chen, C. Y., Trees, D. L. & Morse, S. A. Identification and cloning of a fur homolog from Neisseria gonorrhoeae. Infect. Immun. 61, 4599–4606 (1993). This study identifies and initially characterizes the major iron-regulatory protein Fur in N. gonorrhoeae.
Isabella, V. M. & Clark, V. L. Deep sequencing-based analysis of the anaerobic stimulon in Neisseria gonorrhoeae. BMC Genomics 12, 51 (2011). This study identifies a wide array of genes that are differentially expressed under aerobic and anaerobic conditions in microaerophile N. gonorrhoeae , highlighting the large overlap among genes that are differentially regulated in response to low oxygen, changes in iron levels and the presence of reactive oxygen species.
Ducey, T. F., Carson, M. B., Joshua, O. & Stintzi, A. P. & Dyer, D. W. Identification of the iron-responsive genes of Neisseria gonorrhoaea by microarray analysis in defined medium. J. Bacteriol. 187, 4865–4874 (2005).
Stohl, E. A., Criss, A. K. & Seifert, H. S. The transcriptome response of Neisseria gonorrhoeae to hydrogen peroxide reveals genes with previously uncharacterized roles in oxidative damage protection. Mol. Microbiol. 58, 520–532 (2005).
Makino, S., van Putten, J. P. & Meyer, T. F. Phase variation of the opacity outer membrane protein controls invasion by Neisseria gonorrhoeae into human epithelial cells. EMBO J. 10, 1307–1315 (1991). This study shows a positive correlation between the expression of Opa proteins and the binding and invasion of N. gonorrhoeae into Chang conjunctiva human epithelial cells.
Snyder, L. A., Butcher, S. A. & Saunders, N. J. Comparative whole-genome analyses reveal over 100 putative phase-variable genes in the pathogenic Neisseria spp. Microbiology 147, 2321–2332 (2001).
Jordan, P. W., Snyder, L. A. & Saunders, N. J. Strain-specific differences in Neisseria gonorrhoeae associated with the phase variable gene repertoire. BMC Microbiol. 5, 21 (2005).
Srikhanta, Y. N. et al. Phasevarions mediate random switching of gene expression in pathogenic Neisseria. PLOS Pathog. 5, e1000400 (2009). This study characterizes phase-variable DNA methyltransferase activity in N. gonorrhoeae , showing that it affects the expression of virulence-related genes, antimicrobial resistance, human epithelial cervical cell interactions and biofilm formation.
Gawthorne, J. A., Beatson, S. A., Srikhanta, Y. N., Fox, K. L. & Jennings, M. P. Origin of the diversity in DNA recognition domains in phasevarion associated modA genes of pathogenic Neisseria and Haemophilus influenzae. PLOS ONE 7, e32337 (2012).
Jen, F. E., Seib, K. L. & Jennings, M. P. Phasevarions mediate epigenetic regulation of antimicrobial susceptibility in Neisseria meningitidis. Antimicrob. Agents Chemother. 58, 4219–4221 (2014).
Post, D. M. B. et al. Identification and characterization of AckA-dependent protein acetylation in Neisseria gonorrhoeae. PLOS ONE 12, e0179621 (2017).
Seib, K. L., Jen, F. E., Scott, A. L., Tan, A. & Jennings, M. P. Phase variation of DNA methyltransferases and the regulation of virulence and immune evasion in the pathogenic Neisseria. Pathog. Dis. 75, ftx080 (2017).
Gibson, F. P., Leach, D. R. & Lloyd, R. G. Identification of sbcD mutations as cosuppressors of recBC that allow propagation of DNA palindromes in Escherichia coli K-12. J. Bacteriol. 174, 1222–1228 (1992).
Jackson, L. A., Pan, J. C., Day, M. W. & Dyer, D. W. Control of RNA stability by NrrF, an iron-regulated small RNA in Neisseria gonorrhoeae. J. Bacteriol. 195, 5166–5173 (2013).
Ngampasutadol, J. et al. Human factor H interacts selectively with Neisseria gonorrhoeae and results in species-specific complement evasion. J. Immunol. 180, 3426–3435 (2008). This study demonstrates how sialylated LOS binds human factor H and prevents complement-mediated killing of N. gonorrhoeae.
Densen, P. Interaction of complement with Neisseria meningitidis and Neisseria gonorrhoeae. [Review]. Clin. Microbiol. Rev. 2 (Suppl.), S11–S17 (1989).
Petersen, B. H., Graham, J. A. & Brooks, G. F. Human deficiency of the eighth component of complement. The requirement of C8 for serum Neisseria gonorrhoeae bactericidal activity. J. Clin. Invest. 57, 283–290 (1976).
Edwards, J. L., Brown, E. J., Ault, K. A. & Apicella, M. A. The role of complement receptor 3 (CR3) in Neisseria gonorrhoeae infection of human cervical epithelia. Cell. Microbiol. 3, 611–622 (2001).
Edwards, J. L. & Apicella, M. A. The role of lipooligosaccharide in Neisseria gonorrhoeae pathogenesis of cervical epithelia: lipid A serves as a C3 acceptor molecule. Cell. Microbiol. 4, 585–598 (2002).
Edwards, J. L. et al. A co-operative interaction between Neisseria gonorrhoeae and complement receptor 3 mediates infection of primary cervical epithelial cells. Cell. Microbiol. 4, 571–584 (2002).
Schweinle, J. E. et al. Interaction of Neisseria gonorrhoeae with classical complement components, C1-inhibitor, and a monoclonal antibody directed against the Neisserial H.8 antigen. J. Clin. Invest. 83, 397–403 (1989).
Ram, S. et al. A novel sialic acid binding site on factor H mediates serum resistance of sialylated Neisseria gonorrhoeae. J. Exp. Med. 187, 743–752 (1998).
Ram, S. et al. Binding of complement factor H to loop 5 of porin protein 1A: a molecular mechanism of serum resistance of nonsialylated Neisseria gonorrhoeae. J. Exp. Med. 188, 671–680 (1998).
Ram, S. et al. Binding of C4b-binding protein to porin: a molecular mechanism of serum resistance of Neisseria gonorrhoeae. J. Exp. Med. 193, 281–295 (2001).
Gill, D. B. & Atkinson, J. P. CD46 in Neisseria pathogenesis. Trends Mol. Med. 10, 459–465 (2004).
Feinen, B. & Russell, M. W. Contrasting roles of IL-22 and IL-17 in murine genital tract infection by Neisseria gonorrhoeae. Front. Immunol. 3, 11 (2012).
Edwards, J. L. & Butler, E. K. The pathobiology of Neisseria gonorrhoeae lower female genital tract infection. Front. Microbiol. 2, 102 (2011).
Melly, M. A., McGee, Z. A. & Rosenthal, R. S. Ability of monomeric peptidoglycan fragments from Neisseria gonorrhoeae to damage human fallopian-tube mucosa. J. Infect. Dis. 149, 378–386 (1984). This study demonstrates the ability of different N. gonorrhoeae peptidoglycan monomers to damage human fallopian tube mucosal cells in tissue culture.
Mavrogiorgos, N., Mekasha, S., Yang, Y., Kelliher, M. A. & Ingalls, R. R. Activation of NOD receptors by Neisseria gonorrhoeae modulates the innate immune response. Innate Immun. 20, 377–389 (2014).
Fisette, P. L., Ram, S., Andersen, J. M., Guo, W. & Ingalls, R. R. The Lip lipoprotein from Neisseria gonorrhoeae stimulates cytokine release and NF-kappaB activation in epithelial cells in a Toll-like receptor 2-dependent manner. J. Biol. Chem. 278, 46252–46260 (2003).
Massari, P. et al. Cutting edge: Immune stimulation by neisserial porins is toll-like receptor 2 and MyD88 dependent. J. Immunol. 168, 1533–1537 (2002).
Chateau, A. & Seifert, H. S. Neisseria gonorrhoeae survives within and modulates apoptosis and inflammatory cytokine production of human macrophages. Cell. Microbiol. 18, 546–560 (2016).
Gaudet, R. G. et al. Cytosolic detection of the bacterial metabolite HBP activates TIFA-dependent innate immunity. Science 348, 1251–1255 (2015).
Ortiz, M. C. et al. Neisseria gonorrhoeae modulates immunity by polarizing human macrophages to a M2 profile. PLOS ONE 10, e0130713 (2015).
Sadarangani, M., Pollard, A. J. & Gray-Owen, S. D. Opa proteins and CEACAMs: pathways of immune engagement for pathogenic Neisseria. FEMS Microbiol. Rev. 35, 498–514 (2011).
Schmitter, T., Agerer, F., Peterson, L., Munzner, P. & Hauck, C. R. Granulocyte CEACAM3 is a phagocytic receptor of the innate immune system that mediates recognition and elimination of human-specific pathogens. J. Exp. Med. 199, 35–46 (2004).
Sarantis, H. & Gray-Owen, S. D. The specific innate immune receptor CEACAM3 triggers neutrophil bactericidal activities via a Syk kinase-dependent pathway. Cell. Microbiol. 9, 2167–2180 (2007).
Packiam, M., Veit, S. J., Anderson, D. J., Ingalls, R. R. & Jerse, A. E. Mouse strain-dependent differences in susceptibility to Neisseria gonorrhoeae infection and induction of innate immune responses. Infect. Immun. 78, 433–440 (2010).
Dilworth, J. A., Hendley, J. O. & Mandell, G. L. Attachment and ingestion of gonococci human neutrophils. Infect. Immun. 11, 512–516 (1975). This early study shows adherence and ingestion of two different gonococci strains by polymorphonuclear leukocyte neutrophils (PMNs).
Criss, A. K. & Seifert, H. S. Neisseria gonorrhoeae suppresses the oxidative burst of human polymorphonuclear leukocytes. Cell. Microbiol. 10, 2257–2270 (2008). This study demonstrates how different types of Opa-expressing or Opa-less N. gonorrhoeae grown under different conditions differ in their ability to elicit a PMN oxidative burst, as well as the ability of some strains to inhibit the PMN oxidative burst.
Gunderson, C. W. & Seifert, H. S. Neisseria gonorrhoeae elicits extracellular traps in primary neutrophil culture while suppressing the oxidative burst. mBio 6, e02452-14 (2015).
Criss, A. K., Katz, B. Z. & Seifert, H. S. Resistance of Neisseria gonorrhoeae to non-oxidative killing by adherent human polymorphonuclear leucocytes. Cell. Microbiol. 11, 1074–1087 (2009).
Johnson, M. B. & Criss, A. K. Resistance of Neisseria gonorrhoeae to neutrophils. Front. Microbiol. 2, 77 (2011).
Soler-Garcia, A. A. & Jerse, A. E. A. Neisseria gonorrhoeae catalase mutant is more sensitive to hydrogen peroxide and paraquat, an inducer of toxic oxygen radicals. Microb. Pathog. 37, 55–63 (2004).
Gunesekere, I. C. et al. Ecf, an alternative sigma factor from Neisseria gonorrhoeae, controls expression of msrAB, which encodes methionine sulfoxide reductase. J. Bacteriol. 188, 3463–3469 (2006).
Pilch, B. & Mann, M. Large-scale and high-confidence proteomic analysis of human seminal plasma. Genome Biol. 7, R40 (2006).
Schmidt, K. A. et al. Experimental gonococcal urethritis and reinfection with homologous gonococci in male volunteers. Sex. Transm. Dis. 28, 555–564 (2001).
Cahoon, L. A. & Seifert, H. S. Focusing homologous recombination: pilin antigenic variation in the pathogenic Neisseria. Mol. Microbiol. 81, 1136–1143 (2011).
Mandrell, R. E., Griffiss, J. M. & Macher, B. A. Lipooligosaccharides (LOS) of Neisseria gonorrhoeae and Neisseria meningitidis have components that are immunochemically similar to precursors of human blood group antigens. Carbohydrate sequence specificity of the mouse monoclonal antibodies that recognize crossreacting antigens on LOS and human erythrocytes [published erratum appears in J. Exp Med 1988 Oct 1;168, 1517]. J. Exp. Med. 168, 107–126 (1988).
Mandrell, R. E. Further antigenic similarities of Neisseria gonorrhoeae lipooligosaccharides and human glycosphingolipids. Infect. Immun. 60, 3017–3020 (1992).
Gulati, S., McQuillen, D. P., Mandrell, R. E., Jani, D. B. & Rice, P. A. Immunogenicity of Neisseria gonorrhoeae lipooligosaccharide epitope 2C7, widely expressed in vivo with no immunochemical similarity to human glycosphingolipids. J. Infect. Dis. 174, 1223–1237 (1996).
Liu, Y., Islam, E., Jarvis, G., Gray-Owen, S. & Russell, M. Neisseria gonorrhoeae selectively suppresses the development of Th1 and Th2 cells, and enhances Th17 cell responses, through TGF-α- dependent mechanisms. Mucosal Immunol. 5, 320–331 (2012).
Liu, Y., Liu, W. & Russell, M. W. Suppression of host adaptive immune responses by Neisseria gonorrhoeae: role of interleukin 10 and type 1 regulatory T cells. Mucosal Immunol. 7, 165–176 (2014).
Zhu, W. et al. Neisseria gonorrhoeae suppresses dendritic cell-induced, antigen-dependent CD4 T cell proliferation. PLOS ONE 7, e41260 (2012).
Liu, Y., Feinen, B. & Russell, M. W. New concepts in immunity to Neisseria gonorrhoeae: innate responses and suppression of adaptive immunity favor the pathogen, not the host. Front. Microbiol. 2, 52 (2011).
Jerse, A. E., Bash, M. C. & Russell, M. W. Vaccines against gonorrhea: current status and future challenges. Vaccine 32, 1579–1587 (2014).
Petousis-Harris, H. et al. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhoea in New Zealand: a retrospective case-control study. Lancet 390, 1603–1610 (2017).
Zhao, S. et al. Genetics of chromosomally mediated intermediate resistance to ceftriaxone and cefixime in Neisseria gonorrhoeae. Antimicrob. Agents Chemother. 53, 3744–3751 (2009).
Hagman, K. E. et al. Resistance of Neisseria gonorrhoeae to antimicrobial hydrophobic agents is modulated by the mtrRCDE efflux system. Microbiology 141, 611–622 (1995).
Zhao, S., Tobiason, D. M., Hu, M., Seifert, H. S. & Nicholas, R. A. The penC mutation conferring antibiotic resistance in Neisseria gonorrhoeae arises from a mutation in the PilQ secretin that interferes with multimer stability. Mol. Microbiol. 57, 1238–1251 (2005).
Unemo, M. & Shafer, W. M. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin. Microbiol. Rev. 27, 587–613 (2014).
Jerse, A. E. et al. A gonococcal efflux pump system enhances bacterial survival in a female mouse model of genital tract infection. Infect. Immun. 71, 5576–5582 (2003).
Unemo, M. & Shafer, W. M. Antibiotic resistance in Neisseria gonorrhoeae: origin, evolution, and lessons learned for the future. Ann. NY Acad. Sci. 1230, E19–E28 (2011).
Hook, M. W., Schafer, W., Deal, C., Kirkcaldy, R. D. & Iskander, J. CDC Grand Rounds: the growing threat of multidrug-resistant gonorrhea. MMWR Morb. Mortal. Wkly Rep. 62, 103–106 (2013).
Unemo, M. & Nicholas, R. A. Emergence of multidrug-resistant, extensively drug-resistant and untreatable gonorrhea. Future Microbiol. 7, 1401–1422 (2012).
Aas, F. E., Lovold, C. & Koomey, M. An inhibitor of DNA binding and uptake events dictates the proficiency of genetic transformation in Neisseria gonorrhoeae: mechanism of action and links to Type IV pilus expression. Mol. Microbiol. 46, 1441–1450 (2002).
Hamilton, H. L. & Dillard, J. P. Natural transformation of Neisseria gonorrhoeae: from DNA donation to homologous recombination. Mol. Microbiol. 59, 376–385 (2006).
Bowler, L. D., Zhang, Q. Y., Riou, J. Y. & Spratt, B. G. Interspecies recombination between the penA genes of Neisseria meningitidis and commensal Neisseria species during the emergence of penicillin resistance in N. meningitidis: natural events and laboratory simulation. J. Bacteriol. 176, 333–337 (1994).
Ng, L. K. & Martin, I. E. The laboratory diagnosis of Neisseria gonorrhoeae. Can. J. Infect. Dis. Med. Microbiol. 16, 15–25 (2005).
De Silva, D. et al. Whole-genome sequencing to determine transmission of Neisseria gonorrhoeae: an observational study. Lancet Infect. Dis. 16, 1295–1303 (2016).
Harrison, O. B. et al. Genomic analysis of urogenital and rectal Neisseria meningitidis isolates reveals encapsulated hyperinvasive meningococci and coincident multidrug-resistant gonococci. Sex. Transm. Infect. 93, 445–451 (2017).
Johnson, L. F. & Lewis, D. A. The effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex. Transm. Dis. 35, 946–959 (2008).
Kalichman, S. C., Pellowski, J. & Turner, C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sex. Transm. Infect. 87, 183–190 (2011).
Jerse, A. E. et al. Estradiol-Treated female mice as surrogate hosts for Neisseria gonorrhoeae genital tract infections. Front. Microbiol. 2, 107 (2011).
Zarantonelli, M. L. et al. Transgenic mice expressing human transferrin as a model for meningococcal infection. Infect. Immun. 75, 5609–5614 (2007).
Gu, A., Zhang, Z., Zhang, N., Tsark, W. & Shively, J. E. Generation of human CEACAM1 transgenic mice and binding of Neisseria Opa protein to their neutrophils. PLOS ONE 5, e10067 (2010).
Li, G. et al. Establishment of a human CEACAM1 transgenic mouse model for the study of gonococcal infections. J. Microbiol. Methods 87, 350–354 (2011). This study presents and characterizes a transgenic mouse model for gonorrhoea infection wherein the mouse has been made to express a humanized CEACAM receptor molecule important for adherence and colonization, enabling N. gonorrhoeae to intravaginally colonize the mouse.
Winther-Larsen, H. C. et al. in 13th International Pathogenic Neisseria Conference (eds Caugant, D. A. & Wedege, E.) 37 (Oslo, 2002)
Pearce, W. A. & Buchanan, T. M. Attachment role of gonococcal pili. Optimum conditions and quantitation of adherence of isolated pili to human cells in vitro. J. Clin. Invest. 61, 931–943 (1978).
Kaparakis, M. et al. Bacterial membrane vesicles deliver peptidoglycan to NOD1 in epithelial cells. Cell. Microbiol. 12, 372–385 (2010).
Zhou, X. et al. Hexa-acylated lipid A is required for host inflammatory response to Neisseria gonorrhoeae in experimental gonorrhea. Infect. Immun. 82, 184–192 (2014).
Singleton, T. E., Massari, P. & Wetzler, L. M. Neisserial porin-induced dendritic cell activation is MyD88 and TLR2 dependent. J. Immunol. 174, 3545–3550 (2005).
Liu, X. et al. Gonococcal lipooligosaccharide suppresses HIV infection in human primary macrophages through induction of innate immunity. J. Infect. Dis. 194, 751–759 (2006).
Remmele, C. W. et al. Transcriptional landscape and essential genes of Neisseria gonorrhoeae. Nucleic Acids Res. 42, 10579–10595 (2014).
Lee, E. H. & Shafer, W. M. The farAB-encoded efflux pump mediates resistance of gonococci to long-chained antibacterial fatty acids. Mol. Microbiol. 33, 839–845 (1999).
Lee, E. H., Rouquette-Loughlin, C., Folster, J. P. & Shafer, W. M. FarR regulates the farAB-encoded efflux pump of Neisseria gonorrhoeae via an MtrR regulatory mechanism. J. Bacteriol. 185, 7145–7152 (2003).
Warner, D. M., Folster, J. P., Shafer, W. M. & Jerse, A. E. Regulation of the MtrC-MtrD-MtrE efflux-pump system modulates the in vivo fitness of Neisseria gonorrhoeae. J. Infect. Dis. 196, 1804–1812 (2007).
Seib, K. L. et al. Characterization of the OxyR regulon of Neisseria gonorrhoeae. Mol. Microbiol. 63, 54–68 (2007).
Overton, T. W. et al. Coordinated regulation of the Neisseria gonorrhoeae-truncated denitrification pathway by the nitric oxide-sensitive repressor, NsrR, and nitrite-insensitive NarQ-NarP. J. Biol. Chem. 281, 33115–33126 (2006).
Wu, H. J. et al. PerR controls Mn-dependent resistance to oxidative stress in Neisseria gonorrhoeae. Mol. Microbiol. 60, 401–416 (2006).
Gunesekere, I. C. et al. Comparison of the RpoH-dependent regulon and general stress response in Neisseria gonorrhoeae. J. Bacteriol. 188, 4769–4776 (2006).
Gangaiah, D. et al. Both MisR (CpxR) and MisS (CpxA) are required for Neisseria gonorrhoeae infection in a murine model of lower genital tract infection. Infect. Immun. 85, e00307-17 (2017).
Yu, C., McClure, R., Nudel, K., Daou, N. & Genco, C. A. Characterization of the Neisseria gonorrhoeae iron and Fur regulatory network. J. Bacteriol. 198, 2180–2191 (2016).
Tseng, H. J., McEwan, A. G., Apicella, M. A. & Jennings, M. P. OxyR acts as a repressor of catalase expression in Neisseria gonorrhoeae. Infect. Immun. 71, 550–556 (2003).
Kim, J. J., Zhou, D., Mandrell, R. E. & Griffiss, J. M. Effect of exogenous sialylation of the lipooligosaccharide of Neisseria gonorrhoeae on opsonophagocytosis. Infect. Immun. 60, 4439–4442 (1992).
Blom, A. M. & Ram, S. Contribution of interactions between complement inhibitor C4b-binding protein and pathogens to their ability to establish infection with particular emphasis on Neisseria gonorrhoeae. Vaccine 26 (Suppl. 8), I49–I55 (2008).
Jarvis, G. A. Analysis of C3 deposition and degradation on Neisseria meningitidis and Neisseria gonorrhoeae. Infect. Immun. 62, 1755–1760 (1994).
Yu, Q. et al. Association of Neisseria gonorrhoeae Opa(CEA) with dendritic cells suppresses their ability to elicit an HIV-1-specific T cell memory response. PLOS ONE 8, e56705 (2013).
Ison, C. A., Deal, C. & Unemo, M. Current and future treatment options for gonorrhoea. Sex. Transm. Infect. 89 (Suppl. 4), iv52–iv56 (2013).
Acknowledgements
H.S.S. was supported by the US National Institutes of Health (NIH) grant R37-AI033493. S.J.Q. was partially supported by NIH grant T32-AI0007476.
Author information
Authors and Affiliations
Contributions
S.J.Q. and H.S.S. contributed to researching data for the article. S.J.Q. and H.S.S. substantially contributed to the discussion of content. S.J.Q. and H.S.S. wrote the article. S.J.Q. and H.S.S. reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Exotoxins
-
Bacterial secreted proteins that damage host cells.
- Pelvic inflammatory disease
-
A clinical syndrome where infected fallopian tube tissues are damaged by the host inflammatory response to bacteria.
- Ectopic pregnancy
-
A sequela of pelvic inflammatory disease that occurs when a fertilized egg implants anywhere other than the uterine lining, such as in the fallopian tube, which risks organ damage and blood loss.
- Purulent exudate
-
The hallmark symptom of gonorrhoea; a liquid genital secretion composed of neutrophils and Neisseria gonorrhoeae.
- Microcolonies
-
Collections of bacterial cells that exist as discrete formations.
- Antigenic variation
-
A reversible process by which a microorganism provides many different versions of a gene product at a frequency higher than the normal mutation rate.
- Phase variation
-
A stochastic form of genetic change that varies gene expression on/off or up/down.
- Biofilms
-
Structured formations of bacterial cells within an extracellular matrix that stick to one another and together on a surface.
- C4b-binding protein
-
(C4BP). A classical complement pathway regulatory protein, akin to factor H in the alternative pathway, that regulates complement activation on host cells.
- Factor H
-
A control protein of the alternative complement pathway that binds C3b, displacing activated factor Bb and enabling cleavage and subsequent inactivation of C3b by factor I-induced conversion to iC3b.
- Oxidative burst
-
An antimicrobial response through the release of reactive oxygen species from host cells.
- Transcytosis
-
The transit of the cellular epithelium by a bacterium.
- Nutritional immunity
-
The ability of the host to sequester important nutrients during infection.
- Siderophores
-
Low molecular mass iron-binding chemical compounds secreted by bacteria to chelate iron for subsequent uptake into the bacterial cell.
- Microaerophilic
-
Environments where oxygen concentration is limited but not zero.
- Alternative complement pathway
-
One arm of the complement system that is triggered by C3b binding to a microorganism or other surface, damaged tissue and foreign material.
- Classical complement pathway
-
One arm of the complement system triggered by antigen–antibody complexes with immunoglobulin G (IgG) and IgM antibodies.
- Complement C3
-
An innate immune protein at the centre of the alternative and classical complement pathways.
- Membrane attack complexes
-
Groups of proteins that are formed of complement components C8 and C9 that form pores in the membranes of microorganisms.
- Complement system
-
An innate immune defence that recognizes and kills microorganisms through opsonization and formation of membrane attack complexes.
- Opsonization
-
The process by which host molecules bind to the surface of a microorganism to enhance phagocytosis.
- Outer membrane vesicle
-
A membrane-bound vesicle that is secreted from the bacterial envelope and can contain a variety of cellular material.
- Mosaic alleles
-
Gene alleles that are produced by recombination of different gene sequences.
- Multilocus sequence typing
-
A system to define strains of a species by defining the DNA sequence of alleles of a defined series of housekeeping genes.
Rights and permissions
About this article
Cite this article
Quillin, S., Seifert, H. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat Rev Microbiol 16, 226–240 (2018). https://doi.org/10.1038/nrmicro.2017.169
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/nrmicro.2017.169
This article is cited by
-
Prevalence of Ureaplasma urealyticum, Chlamydia trachomatis, Neisseria gonorrhoeae and Herpes simplex virus in Hangzhou, China
BMC Infectious Diseases (2025)
-
Infections of chlamydia trachomatis, mycoplasma genitalium and neisseria gonorrhoeae among the outpatients of reproductive medicine center in Chongqing, China: a retrospective study
BMC Infectious Diseases (2025)
-
Strain tracking in complex microbiomes using synteny analysis reveals per-species modes of evolution
Nature Biotechnology (2025)
-
Rethinking concepts of virulence with Neisseria gonorrhoeae
Nature Microbiology (2025)
-
A novel GMMA-based gonococcal vaccine demonstrates functional immune responses in mice
npj Vaccines (2025)