Key Points
-
Infections are a leading cause of death in patients suffering from acute CNS injury, such as stroke, traumatic brain injury or spinal cord injury. In affected patients infections impede neurological recovery and increase morbidity as well as mortality.
-
CNS injury induces a disturbance of the normally well balanced interplay between the immune system and the CNS.
-
Brain injury leads to a characteristic immunological phenotype, which is immunodepressant.
-
During systemic inflammation, either as a result of bacterial infection or injury, the CNS mounts a homeostatic, counter-regulatory anti-inflammatory response. However, when triggered by CNS injury, in the absence of systemic inflammation, this response may be detrimental because it shuts down defence mechanisms, rendering the affected organism susceptible to infection. Under these conditions, the immunodepression exerted by the brain is not balanced by general immunostimulation.
-
CNS injury suppresses cell-mediated immune responses via three major pathways of neuroimmunomodulation: the hypothalamo–pituitary–adrenal (HPA) axis, and the sympathetic and parasympathetic nervous systems.
-
We propose that 'neurogenic' mechanisms are involved in the induction of CNS injury-induced immunodepression (CIDS). Damage to sites in the nervous system that control neural–immune interactions (such as the hypothalamus) may lead to anti-inflammatory signals, without initial involvement of immune mechanisms.
-
CIDS is an important, independent contributor to the negative outcomes of patients with brain injury.
-
Recognizing and understanding CIDS could lead to novel treatment strategies to improve outcome in patients with CNS injury.
Abstract
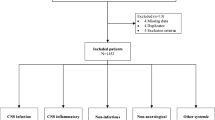
Infections are a leading cause of morbidity and mortality in patients with acute CNS injury. It has recently become clear that CNS injury significantly increases susceptibility to infection by brain-specific mechanisms: CNS injury induces a disturbance of the normally well balanced interplay between the immune system and the CNS. As a result, CNS injury leads to secondary immunodeficiency — CNS injury-induced immunodepression (CIDS) — and infection. CIDS might serve as a model for the study of the mechanisms and mediators of brain control over immunity. More importantly, understanding CIDS will allow us to work on developing effective therapeutic strategies, with which the outcome after CNS damage by a host of diseases could be improved by eliminating a major determinant of poor recovery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Davenport, R. J., Dennis, M. S., Wellwood, I. & Warlow, C. P. Complications after acute stroke. Stroke 27, 415–420 (1996).
Langhorne, P. et al. Medical complications after stroke: a multicenter study. Stroke 31, 1223–1229 (2000).
Weimar, C. et al. Complications following acute ischemic stroke. Eur. Neurol. 48, 133–140 (2002).
Hufeland, C. W. Enchiridion Medicum (Jonas Verlagsbuchhandlung, Berlin, 1836). Classical text book of clinical medicine (in German) containing a vivid description of the natural course of 'apoplexia', and possibly the first article to link fever and stroke.
Georgilis, K., Plomaritoglou, A., Dafni, U., Bassiakos, Y. & Vemmos, K. Aetiology of fever in patients with acute stroke. J. Intern. Med. 246, 203–209 (1999).
Diez-Tejedor, E. & Fuentes, B. Acute care in stroke: the importance of early intervention to achieve better brain protection. Cerebrovasc. Dis. 17 (Suppl. 1), 130–137 (2004).
Hajat, C., Hajat, S. & Sharma, P. Effects of poststroke pyrexia on stroke outcome: a meta-analysis of studies in patients. Stroke 31, 410–414 (2000).
Grau, A. J. et al. Fever and infection early after ischemic stroke. J. Neurol. Sci. 171, 115–120 (1999).
Johnston, K. C. et al. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. RANTTAS Investigators. Stroke 29, 447–453 (1998).
Kalra, L., Yu, G., Wilson, K. & Roots, P. Medical complications during stroke rehabilitation. Stroke 26, 990–994 (1995).
Henon, H. et al. Early predictors of death and disability after acute cerebral ischemic event. Stroke 26, 392–398 (1995).
Rodriguez, R. et al. 3 year survival in patients hospitalized for acute cerebrovascular disorders. Rev. Neurol. 24, 199–206 (1996).
Vernino, S. et al. Cause-specific mortality after first cerebral infarction: a population-based study. Stroke 34, 1828–1832 (2003).
Heuschmann, P. U. et al. Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: the German Stroke Registers Study Group. Arch. Intern. Med. 164, 1761–1768 (2004).
Hilker, R. et al. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke 34, 975–981 (2003).
Katzan, I. L., Cebul, R. D., Husak, S. H., Dawson, N. V. & Baker, D. W. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 60, 620–625 (2003).
Nakajoh, K. et al. Relation between incidence of pneumonia and protective reflexes in post-stroke patients with oral or tube feeding. J. Intern. Med. 247, 39–42 (2000).
Marik, P. E. Aspiration pneumonitis and aspiration pneumonia. N. Engl. J. Med. 344, 665–671 (2001). Review article describing a concise concept of pneumonitis and pneumonia following aspiration, its differentiation and risk factors (for example, stroke).
Perry, L. & Love, C. P. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia 16, 7–18 (2001).
Nakagawa, T. et al. Silent cerebral infarction: a potential risk for pneumonia in the elderly. J. Intern. Med. 247, 255–259 (2000).
Fabregas, N. & Torres, A. Pulmonary infection in the brain injured patient. Minerva Anestesiol. 68, 285–290 (2002).
Piek, J. et al. Extracranial complications of severe head injury. J. Neurosurg. 77, 901–907 (1992).
Chastre, J. & Fagon, J. Y. Ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 165, 867–903 (2002).
Bronchard, R. et al. Early onset pneumonia: risk factors and consequences in head trauma patients. Anesthesiology 100, 234–239 (2004).
Ewig, S. et al. Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Incidence, risk factors, and association with ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 159, 188–198 (1999).
Woratyla, S. P., Morgan, A. S., Mackay, L., Bernstein, B. & Barba, C. Factors associated with early onset pneumonia in the severely brain-injured patient. Conn. Med. 59, 643–647 (1995).
Campbell, W., Hendrix, E., Schwalbe, R., Fattom, A. & Edelman, R. Head-injured patients who are nasal carriers of Staphylococcus aureus are at high risk for Staphylococcus aureus pneumonia. Crit. Care Med. 27, 798–801 (1999).
Woiciechowsky, C. et al. Early IL-6 plasma concentrations correlate with severity of brain injury and pneumonia in brain-injured patients. J. Trauma 52, 339–345 (2002).
Ishikawa, K. et al. Characteristics of infection and leukocyte count in severely head-injured patients treated with mild hypothermia. J. Trauma 49, 912–922 (2000).
Nadal, P., Nicolas, J. M., Font, C., Vilella, A. & Nogue, S. Pneumonia in ventilated head trauma patients: the role of thiopental therapy. Eur. J. Emerg. Med. 2, 14–16 (1995).
Kollef, M. H., Silver, P., Murphy, D. M. & Trovillion, E. The effect of late-onset ventilator-associated pneumonia in determining patient mortality. Chest 108, 1655–1662 (1995).
Sirvent, J. M. et al. Protective effect of intravenously administered cefuroxime against nosocomial pneumonia in patients with structural coma. Am. J. Respir. Crit. Care Med. 155, 1729–1734 (1997).
Jackson, A. B. & Groomes, T. E. Incidence of respiratory complications following spinal cord injury. Arch. Phys. Med. Rehabil. 75, 270–275 (1994).
Waites, K. B., Canupp, K. C., Chen, Y., DeVivo, M. J. & Moser, S. A. Bacteremia after spinal cord injury in initial versus subsequent hospitalizations. J. Spinal Cord Med. 24, 96–100 (2001).
DeVivo, M. J., Black, K. J. & Stover, S. L. Causes of death during the first 12 years after spinal cord injury. Arch. Phys. Med. Rehabil. 74, 248–254 (1993). References 33–37 detail seminal work using the SCI model system, which reports and quantifies infectious complications after SCI. They provide a clinical-epidemiological hint for a relative state of anergia attributable to SCI.
DeVivo, M. J., Krause, J. S. & Lammertse, D. P. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch. Phys. Med. Rehabil. 80, 1411–1419 (1999).
Ragnarsson, K. T., Carter, R. E., Wilmot, C. B. & Hall, K. M. Spinal Cord Injury: Clinical Outcomes from the Model Systems (eds Stover, S. L., Whiteneck, G. G. & deLisa, J. A.) 79–99 (Aspen Publishers Inc, USA, 1995).
Reines, H. D. & Harris, R. C. Pulmonary complications of acute spinal cord injuries. Neurosurgery 21, 193–196 (1987).
Inamasu, J., Nakamura, Y. & Ichikizaki, K. Induced hypothermia in experimental traumatic spinal cord injury: an update. J. Neurol. Sci. 209, 55–60 (2003).
Meisel, C. et al. Preventive antibacterial treatment improves the general medical and neurological outcome in a mouse model of stroke. Stroke 35, 2–6 (2004).
Cruse, J. M., Lewis, R. E., Bishop, G. R., Kliesch, W. F. & Gaitan, E. Neuroendocrine–immune interactions associated with loss and restoration of immune system function in spinal cord injury and stroke patients. Immunol. Res. 11, 104–116 (1992).
Czlonkowska, A., Cyrta, B. & Korlak, J. Immunological observations on patients with acute cerebral vascular disease. J. Neurol. Sci. 43, 455–464 (1979). One of the first clinical studies demonstrating a marked inhibition of cell-mediated immune responses in patients after cerebral infarction, including suppressed DTH skin reactivity and reduced mitogenic T-cell responses, which correlated with disease severity.
Hoyt, D. B., Ozkan, A. N., Hansbrough, J. F., Marshall, L. & van Berkum-Clark, M. Head injury: an immunologic deficit in T-cell activation. J. Trauma 30, 759–766 (1990).
Quattrocchi, K. B. et al. Impairment of helper T-cell function and lymphokine-activated killer cytotoxicity following severe head injury. J. Neurosurg. 75, 766–773 (1991).
Woiciechowsky, C. et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nature Med. 4, 808–813 (1998). Important study linking brain injury with immunodepression caused by sympathetic overactivation
Kossmann, T. et al. Intrathecal and serum interleukin-6 and the acute-phase response in patients with severe traumatic brain injuries. Shock 4, 311–317 (1995).
Meert, K. L., Long, M., Kaplan, J. & Sarnaik, A. P. Alterations in immune function following head injury in children. Crit. Care Med. 23, 822–828 (1995).
Quattrocchi, K. B. et al. Severe head injury: effect upon cellular immune function. Neurol. Res. 13, 13–20 (1991).
Imhoff, M., Gahr, R. H. & Hoffmann, P. Delayed cutaneous hypersensitivity after multiple injury and severe burn. Ann. Ital. Chir. 61, 525–528 (1990).
Miller, C. H., Quattrocchi, K. B., Frank, E. H., Issel, B. W. & Wagner, F. C. Jr. Humoral and cellular immunity following severe head injury: review and current investigations. Neurol. Res. 13, 117–124 (1991).
Wolach, B., Sazbon, L., Gavrieli, R., Broda, A. & Schlesinger, M. Early immunological defects in comatose patients after acute brain injury. J. Neurosurg. 94, 706–711 (2001).
Maerker-Alzer, G., Beckmann, H., Richard, K. E. & Frowein, R. A. Humoral immunodeficiency syndrome in patients with severe head injury? Neurosurg. Rev. 12 (Suppl. 1), 420–428 (1989).
Campagnolo, D. I., Bartlett, J. A., Keller, S. E., Sanchez, W. & Oza, R. Impaired phagocytosis of Staphylococcus aureus in complete tetraplegics. Am. J. Phys. Med. Rehabil. 76, 276–280 (1997). One of the earliest studies documenting impaired host defence as a function of a hampered innate immune response (immune-suppression) following SCI.
Huschak, G., Zur, N. K., Stuttmann, R. & Riemann, D. Changes in monocytic expression of aminopeptidase N/CD13 after major trauma. Clin. Exp. Immunol. 134, 491–496 (2003).
Wolk, K., Docke, W. D., von Baehr, V., Volk, H. D. & Sabat, R. Impaired antigen presentation by human monocytes during endotoxin tolerance. Blood 96, 218–223 (2000).
Asadullah, K. et al. Immunodepression following neurosurgical procedures. Crit. Care Med. 23, 1976–1983 (1995).
Majetschak, M. et al. The extent of traumatic damage determines a graded depression of the endotoxin responsiveness of peripheral blood mononuclear cells from patients with blunt injuries. Crit. Care Med. 27, 313–318 (1999).
Prass, K. et al. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by poststroke T helper cell type 1-like immunostimulation. J. Exp. Med. 198, 725–736 (2003). Provides experimental proof, for the first time, that a neuroendocrine-mediated systemic immunosuppression after acute brain injury results in the development of spontaneous systemic bacterial infections.
Elenkov, I. J., Wilder, R. L., Chrousos, G. P. & Vizi, E. S. The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system. Pharmacol. Rev. 52, 595–638 (2000). Comprehensive review on the role of the sympathetic nerve in the interactions between the brain and the immune system.
Pavlov, V. A. & Tracey, K. J. Neural regulators of innate immune responses and inflammation. Cell. Mol. Life Sci. 61, 2322–2331 (2004).
Steinman, L. Elaborate interactions between the immune and nervous systems. Nature Immunol. 5, 575–581 (2004).
Mulla, A. & Buckingham, J. C. Regulation of the hypothalamo–pituitary–adrenal axis by cytokines. Baillieres Best. Pract. Res. Clin. Endocrinol. Metab. 13, 503–521 (1999).
Pavlov, V. A., Wang, H., Czura, C. J., Friedman, S. G. & Tracey, K. J. The cholinergic anti-inflammatory pathway: a missing link in neuroimmunomodulation. Mol. Med. 9, 125–134 (2003).
Goehler, L. E. et al. Vagal immune-to-brain communication: a visceral chemosensory pathway. Auton. Neurosci. 85, 49–59 (2000).
Banks, W. A., Kastin, A. J. & Broadwell, R. D. Passage of cytokines across the blood–brain barrier. Neuroimmunomodulation 2, 241–248 (1995).
Buller, K. M. Role of circumventricular organs in pro-inflammatory cytokine-induced activation of the hypothalamic–pituitary–adrenal axis. Clin. Exp. Pharmacol. Physiol. 28, 581–589 (2001).
Weindl, A. in Frontiers in Neuroendocrinology (eds Ganong, W. F. & Martini, L.) 3–32 (Oxford Univ. Press, New York, 1973).
Haddad, J. J., Saade, N. E. & Safieh-Garabedian, B. Cytokines and neuro–immune–endocrine interactions: a role for the hypothalamic–pituitary–adrenal revolving axis. J. Neuroimmunol. 133, 1–19 (2002).
Felten, D. L. et al. Noradrenergic sympathetic neural interactions with the immune system: structure and function. Immunol. Rev. 100, 225–260 (1987).
Benschop, R. J., Rodriguez-Feuerhahn, M. & Schedlowski, M. Catecholamine-induced leukocytosis: early observations, current research, and future directions. Brain Behav. Immun. 10, 77–91 (1996).
Borger, P. et al. β-adrenoceptor-mediated inhibition of IFN-γ, IL-3, and GM-CSF mRNA accumulation in activated human T lymphocytes is solely mediated by the β2-adrenoceptor subtype. Am. J. Respir. Cell Mol. Biol. 19, 400–407 (1998).
Sanders, V. M. et al. Differential expression of the β2-adrenergic receptor by Th1 and Th2 clones: implications for cytokine production and B cell help. J. Immunol. 158, 4200–4210 (1997).
Panina-Bordignon, P. et al. β2-agonists prevent Th1 development by selective inhibition of interleukin 12. J. Clin. Invest. 100, 1513–1519 (1997).
Elenkov, I. J., Papanicolaou, D. A., Wilder, R. L. & Chrousos, G. P. Modulatory effects of glucocorticoids and catecholamines on human interleukin-12 and interleukin-10 production: clinical implications. Proc. Assoc. Am. Physicians 108, 374–381 (1996).
Van der Poll, T., Coyle, S. M., Barbosa, K., Braxton, C. C. & Lowry, S. F. Epinephrine inhibits tumor necrosis factor-α and potentiates interleukin 10 production during human endotoxemia. J. Clin. Invest. 97, 713–719 (1996).
Dokur, M., Boyadjieva, N. & Sarkar, D. K. Catecholaminergic control of NK cell cytolytic activity regulatory factors in the spleen. J. Neuroimmunol. 151, 148–157 (2004).
Shakhar, G. & Ben Eliyahu, S. In vivo β-adrenergic stimulation suppresses natural killer activity and compromises resistance to tumor metastasis in rats. J. Immunol. 160, 3251–3258 (1998).
Takamoto, T. et al. Norepinephrine inhibits human natural killer cell activity in vitro. Int. J. Neurosci. 58, 127–131 (1991).
Tracey, K. J. The inflammatory reflex. Nature 420, 853–859 (2002).
Borovikova, L. V. et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405, 458–462 (2000). The first report to demonstrate a neural anti-inflammatory pathway, consisting of afferent and efferent vagus nerve signalling, through which the CNS modulates systemic inflammatory responses.
Wang, H. et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature 421, 384–388 (2003).
Kwon, O. J. et al. Inhibition of interleukin-8 expression by dexamethasone in human cultured airway epithelial cells. Immunology 81, 389–394 (1994).
Szabo, C., Thiemermann, C., Wu, C. C., Perretti, M. & Vane, J. R. Attenuation of the induction of nitric oxide synthase by endogenous glucocorticoids accounts for endotoxin tolerance in vivo. Proc. Natl Acad. Sci. USA 91, 271–275 (1994).
Wilckens, T. & De Rijk, R. Glucocorticoids and immune function: unknown dimensions and new frontiers. Immunol. Today 18, 418–424 (1997).
AyanlarBatuman, O., Ferrero, A. P., Diaz, A. & Jimenez, S. A. Regulation of transforming growth factor-β 1 gene expression by glucocorticoids in normal human T lymphocytes. J. Clin. Invest. 88, 1574–1580 (1991).
Barrat, F. J. et al. In vitro generation of interleukin 10-producing regulatory CD4+ T cells is induced by immunosuppressive drugs and inhibited by T helper type 1 (Th1)- and Th2-inducing cytokines. J. Exp. Med. 195, 603–616 (2002).
Hodge, S., Hodge, G., Flower, R. & Han, P. Methyl-prednisolone up-regulates monocyte interleukin-10 production in stimulated whole blood. Scand. J. Immunol. 49, 548–553 (1999).
Meagher, L. C., Cousin, J. M., Seckl, J. R. & Haslett, C. Opposing effects of glucocorticoids on the rate of apoptosis in neutrophilic and eosinophilic granulocytes. J. Immunol. 156, 4422–4428 (1996).
Smets, L. A., Salomons, G. & van den Berg, J. Glucocorticoid induced apoptosis in leukemia. Adv. Exp. Med. Biol. 457, 607–614 (1999).
Tuosto, L., Cundari, E., Montani, M. S. & Piccolella, E. Analysis of susceptibility of mature human T lymphocytes to dexamethasone-induced apoptosis. Eur. J. Immunol. 24, 1061–1065 (1994).
Zacharchuk, C. M., Mercep, M., Chakraborti, P. K., Simons, S. S. Jr . & Ashwell, J. D. Programmed T lymphocyte death. Cell activation- and steroid-induced pathways are mutually antagonistic. J. Immunol. 145, 4037–4045 (1990).
Cowan, H. B., Vick, S., Conary, J. T. & Shepherd, V. L. Dexamethasone up-regulates mannose receptor activity by increasing mRNA levels. Arch. Biochem. Biophys. 296, 314–320 (1992).
Liu, Y. et al. Glucocorticoids promote nonphlogistic phagocytosis of apoptotic leukocytes. J. Immunol. 162, 3639–3646 (1999).
Piemonti, L. et al. Glucocorticoids increase the endocytic activity of human dendritic cells. Int. Immunol. 11, 1519–1526 (1999).
Pan, J. et al. Dexamethasone inhibits the antigen presentation of dendritic cells in MHC class II pathway. Immunol. Lett. 76, 153–161 (2001).
Schwiebert, L. M., Schleimer, R. P., Radka, S. F. & Ono, S. J. Modulation of MHC class II expression in human cells by dexamethasone. Cell. Immunol. 165, 12–19 (1995).
Blotta, M. H., DeKruyff, R. H. & Umetsu, D. T. Corticosteroids inhibit IL-12 production in human monocytes and enhance their capacity to induce IL-4 synthesis in CD4+ lymphocytes. J. Immunol. 158, 5589–5595 (1997).
Franchimont, D. et al. Inhibition of Th1 immune response by glucocorticoids: dexamethasone selectively inhibits IL-12-induced Stat4 phosphorylation in T lymphocytes. J. Immunol. 164, 1768–1774 (2000).
Ramierz, F., Fowell, D. J., Puklavec, M., Simmonds, S. & Mason, D. Glucocorticoids promote a TH2 cytokine response by CD4+ T cells in vitro. J. Immunol. 156, 2406–2412 (1996).
Weller, M. & Fontana, A. The failure of current immunotherapy for malignant glioma. Tumor-derived TGF-β, T-cell apoptosis, and the immune privilege of the brain. Brain Res. Rev. 21, 128–151 (1995).
Bodmer, S., Huber, D., Heid, I. & Fontana, A. Human glioblastoma cell derived transforming growth-factor-β-2: evidence for secretion of both high and low-molecular-weight biologically-active forms. J. Neuroimmunol. 34, 33–42 (1991).
Csuka, E. et al. IL-10 levels in cerebrospinal fluid and serum of patients with severe traumatic brain injury: relationship to IL-6, TNF-α, TGF-β 1 and blood–brain barrier function. J. Neuroimmunol. 101, 211–221 (1999).
Stanzani, L. et al. Nerve growth factor and transforming growth factor-β serum levels in acute stroke patients: possible involvement of neurotrophins in cerebrovascular disease. Cerebrovasc. Dis. 12, 240–244 (2001).
Castillo, J. et al. The release of tumor necrosis factor-α is associated with ischemic tolerance in human stroke. Ann. Neurol. 54, 811–819 (2003).
Emsley, H. C. et al. An early and sustained peripheral inflammatory response in acute ischaemic stroke: relationships with infection and atherosclerosis. J. Neuroimmunol. 139, 93–101 (2003).
Grau, A. J. et al. Monocyte function and plasma levels of interleukin-8 in acute ischemic stroke. J. Neurol. Sci. 192, 41–47 (2001).
Smith, C. J. et al. Peak plasma interleukin-6 and other peripheral markers of inflammation in the first week of ischaemic stroke correlate with brain infarct volume, stroke severity and long-term outcome. BMC Neurol. 4, 2 (2004).
Vila, N., Castillo, J., Davalos, A. & Chamorro, A. Proinflammatory cytokines and early neurological worsening in ischemic stroke. Stroke 31, 2325–2329 (2000).
Vila, N. et al. Levels of anti-inflammatory cytokines and neurological worsening in acute ischemic stroke. Stroke 34, 671–675 (2003).
Bone, R. C. Immunologic dissonance: a continuing evolution in our understanding of the systemic inflammatory response syndrome (SIRS) and the multiple organ dysfunction syndrome (MODS). Ann. Intern. Med. 125, 680–687 (1996).
Woiciechowsky, C., Schoning, B., Lanksch, W. R., Volk, H. D. & Docke, W. D. Mechanisms of brain-mediated systemic anti-inflammatory syndrome causing immunodepression. J. Mol. Med. 77, 769–780 (1999).
Sharshar, T., Hopkinson, N. S., Orlikowski, D. & Annane, D. Science review: the brain in sepsis — culprit and victim. Crit. Care 9, 37–44 (2005).
Schwartz, M. Harnessing the immune system for neuroprotection: therapeutic vaccines for acute and chronic neurodegenerative disorders. Cell. Mol. Neurobiol. 21, 617–627 (2001).
Feuerstein, G. Z., Liu, T. & Barone, F. C. Cytokines, inflammation, and brain injury: role of tumor necrosis factor-α. Cerebrovasc. Brain Metab. Rev. 6, 341–360 (1994).
Johansson, A., Olsson, T., Carlberg, B., Karlsson, K. & Fagerlund, M. Hypercortisolism after stroke—partly cytokine-mediated? J. Neurol. Sci. 147, 43–47 (1997).
Szczudlik, A., Dziedzic, T., Bartus, S., Slowik, A. & Kieltyka, A. Serum interleukin-6 predicts cortisol release in acute stroke patients. J. Endocrinol. Invest. 27, 37–41 (2004).
Bethin, K. E., Vogt, S. K. & Muglia, L. J. Interleukin-6 is an essential, corticotropin-releasing hormone-independent stimulator of the adrenal axis during immune system activation. Proc. Natl Acad. Sci. USA 97, 9317–9322 (2000).
Brown, R. et al. Suppression of splenic macrophage interleukin-1 secretion following intracerebroventricular injection of interleukin-1 β: evidence for pituitary-adrenal and sympathetic control. Cell. Immunol. 132, 84–93 (1991).
Sullivan, G. M. et al. Intracerebroventricular injection of interleukin-1 suppresses peripheral lymphocyte function in the primate. Neuroimmunomodulation 4, 12–18 (1997).
van der Meer, M. J. et al. Acute stimulation of the hypothalamic–pituitary–adrenal axis by IL-1 β, TNF α and IL-6: a dose response study. J. Endocrinol. Invest. 19, 175–182 (1996).
Sundar, S. K. et al. Intracerebroventricular infusion of interleukin 1 rapidly decreases peripheral cellular immune responses. Proc. Natl Acad. Sci. USA 86, 6398–6402 (1989).
Woiciechowsky, C. et al. Brain-IL-1β induces local inflammation but systemic anti-inflammatory response through stimulation of both hypothalamic–pituitary–adrenal axis and sympathetic nervous system. Brain Res. 816, 563–571 (1999).
Stevens-Felten, S. Y. & Bellinger, D. L. Noradrenergic and peptidergic innervation of lymphoid organs. Chem. Immunol. 69, 99–131 (1997).
Teasell, R. W., Arnold, J. M., Krassioukov, A. & Delaney, G. A. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch. Phys. Med. Rehabil. 81, 506–516 (2000).
Chesnut, R. M., Gautille, T., Blunt, B. A., Klauber, M. R. & Marshall, L. F. Neurogenic hypotension in patients with severe head injuries. J. Trauma 44, 958–963 (1998).
Meyer, S., Strittmatter, M., Fischer, C., Georg, T. & Schmitz, B. Lateralization in autonomic dysfunction in ischemic stroke involving the insular cortex. Neuroreport 15, 357–361 (2004).
Saphier, D. & Feldman, S. Effects of stimulation of the preoptic area on hypothalamic paraventricular nucleus unit activity and corticosterone secretion in freely moving rats. Neuroendocrinology 42, 167–173 (1986).
Tibbs, P. A., Young, B., Ziegler, M. G. & McAllister, R. G. Jr. Studies of experimental cervical spinal cord transection. Part II: plasma norepinephrine levels after acute cervical spinal cord transection. J. Neurosurg. 50, 629–632 (1979).
Feibel, J. H., Hardy, P. M., Campbell, R. G., Goldstein, M. N. & Joynt, R. J. Prognostic value of the stress response following stroke. JAMA 238, 1374–1376 (1977).
Harper, R. M., Bandler, R., Spriggs, D. & Alger, J. R. Lateralized and widespread brain activation during transient blood pressure elevation revealed by magnetic resonance imaging. J. Comp. Neurol. 417, 195–204 (2000).
Kalogeras, K. T. et al. Inferior petrosal sinus sampling in healthy subjects reveals a unilateral corticotropin-releasing hormone-induced arginine vasopressin release associated with ipsilateral adrenocorticotropin secretion. J. Clin. Invest. 97, 2045–2050 (1996).
Meador, K. J. et al. Role of cerebral lateralization in control of immune processes in humans. Ann. Neurol. 55, 840–844 (2004).
Tarkowski, E. et al. Localization of the brain lesion affects the lateralization of T-lymphocyte dependent cutaneous inflammation. Evidence for an immunoregulatory role of the right frontal cortex–putamen region. Scand. J. Immunol. 47, 30–36 (1998).
Robinson, R. G. Differential behavioral and biochemical effects of right and left hemispheric cerebral infarction in the rat. Science 205, 707–710 (1979).
Tarkowski, E., Naver, H., Wallin, B. G., Blomstrand, C. & Tarkowski, A. Lateralization of T-lymphocyte responses in patients with stroke. Effect of sympathetic dysfunction? Stroke 26, 57–62 (1995).
Cechetto, D. F. & Chen, S. J. Subcortical sites mediating sympathetic responses from insular cortex in rats. Am. J. Physiol. 258, R245–R255 (1990).
Sander, D. & Klingelhofer, J. Changes of circadian blood pressure patterns and cardiovascular parameters indicate lateralization of sympathetic activation following hemispheric brain infarction. J. Neurol. 242, 313–318 (1995).
Popovich, P. G. Immunological regulation of neuronal degeneration and regeneration in the injured spinal cord. Prog. Brain Res. 128, 43–58 (2000).
Evans, A. et al. Can differences in management processes explain different outcomes between stroke unit and stroke-team care? Lancet 358, 1586–1592 (2001).
Ronning, O. M. & Guldvog, B. Stroke unit versus general medical wards, II: neurological deficits and activities of daily living: a quasi-randomized controlled trial. Stroke 29, 586–590 (1998).
Ronning, O. M. & Guldvog, B. Stroke units versus general medical wards, I: twelve- and eighteen-month survival: a randomized, controlled trial. Stroke 29, 58–62 (1998).
Furuichi, S. et al. Related changes in sympathetic activity, cerebral blood flow and intracranial pressure, and effect of an alpha-blocker in experimental subarachnoid haemorrhage. Acta Neurochir. (Wien.) 141, 415–423 (1999).
Naredi, S. et al. Increased sympathetic nervous activity in patients with nontraumatic subarachnoid hemorrhage. Stroke 31, 901–906 (2000).
Palasik, W., Popow, J., Lechowicz, W., Fiszer, U. & Czlonkowska, A. The use of gammaglobulin for preventing infection in stroke. Neurol. Neurochir. Pol. 29, 309–316 (1995).
Strand, T., Alling, C., Karlsson, B., Karlsson, I. & Winblad, B. Brain and plasma proteins in spinal fluid as markers for brain damage and severity of stroke. Stroke 15, 138–144 (1984).
Becker, K., Kindrick, D., McCarron, R., Hallenbeck, J. & Winn, R. Adoptive transfer of myelin basic protein-tolerized splenocytes to naive animals reduces infarct size: a role for lymphocytes in ischemic brain injury? Stroke 34, 1809–1815 (2003). Study showing that immunological tolerance and its neuroprotective effects in stroke can be transferred to naive animals and are related to antigen-specific induction of transforming growth factor-β1.
Schwab, J. M., Nguyen, T. D., Meyermann, R. & Schluesener, H. J. Human focal cerebral infarctions induce differential lesional interleukin-16 (IL-16) expression confined to infiltrating granulocytes, CD8+ T-lymphocytes and activated microglia/macrophages. J. Neuroimmunol. 114, 232–241 (2001).
Acknowledgements
The authors' work is supported by the Hermann and Lilly Schilling Foundation, the Wings for Life Spinal Cord Research Foundation, and the Deutsche Forschungsgemeinschaft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
A patent application on preventive anti-infective and immunomodulatory therapy in stroke has been filed by A. M., C. M., K. P. and U. D. to the European Patent Office. Patent owner: Charité Universitätsmedizin Berlin.
Glossary
- INNATE AND ADAPTIVE IMMUNITY
-
The early phases of the host response to a pathogen depend on innate resistance mechanisms. The activation of innate effector mechanisms induces the clonal expansion of antigen-specific lymphocytes and initiates adaptive immune responses, including the development of immunological memory.
- STROKE
-
There are two main types of stroke: ischaemic (caused by blockage in an artery that supplies blood to the brain) and haemorrhagic (caused by the bleeding of ruptured blood vessels in the brain).
- NOSOCOMIAL
-
A disease acquired in hospital.
- HYPOXAEMIA
-
Describes critically decreased arterial oxygen levels.
- SYSTEMIC INFLAMMATORY RESPONSE SYNDROME
-
(SIRS). This describes the host response to a critical illness of either infectious or noninfectious aetiology. The response is mediated by a cascade of pro-inflammatory mediators, such as inflammatory cytokines (for example, TNFα), activated complement factors and lipid mediators.
- HUMORAL
-
Derived from the blood.
- ENDOTOXINS
-
Inflammatory bacterial cell wall products that can cause sepsis.
- TYPE 1 T-HELPER T CELLS
-
(Th1). T-helper cells can be divided on the basis of their cytokine expression pattern. Th1 cells produce mostly IFNγ and mediate delayed-type hypersensitivity and protection against intracellular pathogens.
- TYPE 2 T-HELPER T CELLS
-
(Th2). Th2 cells produce mainly IL-4 and IL-5, and have been implicated in humoral and allergic immune responses.
- COMPENSATORY ANTI-INFLAMMATORY RESPONSE SYNDROME
-
(CARS). The systemic inflammatory response induces, and is then balanced by, counter-regulatory processes, known as CARS. This includes the release of anti-inflammatory molecules (for example, IL-10) and activation of neuroendocrine pathways (for example, the HPA axis).
- NEUROGENIC
-
Caused by a primarily neuronal mechanism through either blockade or stimulation of trans-synaptic nerve conduction.
Rights and permissions
About this article
Cite this article
Meisel, C., Schwab, J., Prass, K. et al. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci 6, 775–786 (2005). https://doi.org/10.1038/nrn1765
Published:
Issue date:
DOI: https://doi.org/10.1038/nrn1765
This article is cited by
-
Red cell distribution width to lymphocyte ratio could serve as a new inflammatory biomarker for predicting hematoma expansion in patients with intracerebral hemorrhage
BMC Neurology (2024)
-
The role of stroke-induced immunosuppression as a predictor of functional outcome in the neurorehabilitation setting
Scientific Reports (2024)
-
Early Intraventricular Antibiotic Therapy Improved In-Hospital-Mortality in Neurocritical Patients with Multidrug-Resistant Bacterial Nosocomial Meningitis and Ventriculitis
Neurocritical Care (2024)
-
Ventilator-associated pneumonia in neurocritically ill patients: insights from the ENIO international prospective observational study
Respiratory Research (2023)
-
The Osaka prognostic score and Naples prognostic score: novel biomarkers for predicting short-term outcomes after spontaneous intracerebral hemorrhage
BMC Neurology (2023)