Abstract
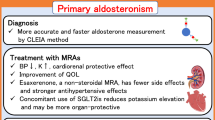
Mineralocorticoid-receptor antagonists (MRAs) reduce blood pressure and albuminuria in patients treated with angiotensin-converting-enzyme inhibitors or angiotensin-II-receptor blockers. The use of MRAs, however, is limited by the occurrence of hyperkalaemia, which frequently occurs in patients older than 65 years with impaired kidney function, and/or diabetes. Patients with these characteristics might still benefit from MRA therapy, however, and should not be excluded from this treatment option. This limitation raises the question of how to optimize the therapeutic use of MRAs in this population of patients. Understanding the individual variability in patients' responses to MRAs, in terms of albuminuria, blood pressure and serum potassium levels, might lead to targeted intervention. MRA use might be restricted to patients with high levels of mineralocorticoid activity, evaluated by circulating renin and aldosterone levels or renal excretion of potassium. In addition, reviewing the patient's diet and concomitant medications might prove useful in reducing the risk of developing subsequent hyperkalaemia. If hyperkalaemia does develop, treatment options exist to decrease potassium levels, including administration of calcium gluconate, insulin, β2-agonists, diuretics and cation-exchange resins. In combination with novel aldosterone blockers, these strategies might offer a rationale with which to optimize therapeutic intervention and extend the population of patients who can benefit from use of MRAs.
Key Points
-
Hyperkalaemia is a well-known adverse effect of mineralocorticoid-receptor antagonist (MRA) therapy that can cause cardiac dysfunction and even lead to premature death
-
Understanding intraindividual variability in responses to MRA therapy—in terms of albuminuria, blood pressure and serum K+ levels—might help to dissociate beneficial effects of MRAs from harmful ones
-
Identification of risk factors that predispose patients to develop hyperkalaemia and monitoring of mineralocorticoid activity might help to improve personalization of MRA therapy
-
Serum levels of K+ should be closely monitored in the first 2 weeks of MRA therapy, for example by trans-tubular potassium gradient measurement
-
Use of loop and osmotic diuretics, treatment with Na+ bicarbonate, reducing K+ intake and avoiding medications that affect K+ homeostasis might reduce the risk of hyperkalaemia during MRA therapy
-
Several pharmacological options are currently available (and others are in development) to prevent and control hyperkalaemia in patients with chronic kidney disease receiving MRAs
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
MacKinnon, M. et al. Combination therapy with an angiotensin receptor blocker and an ACE inhibitor in proteinuric renal disease: a systematic review of the efficacy and safety data. Am. J. Kidney Dis. 48, 8–20 (2006).
Werner, C. et al. RAS blockade with ARB and ACE inhibitors: current perspective on rationale and patient selection. Clin. Res. Cardiol. 97, 418–431 (2008).
de Zeeuw, D. et al. Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Int. 65, 2309–2320 (2004).
de Zeeuw, D. et al. Albuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathy. Circulation 110, 921–927 (2004).
Holtkamp, F. A. et al. Albuminuria and blood pressure, independent targets for cardioprotective therapy in patients with diabetes and nephropathy: a post hoc analysis of the combined RENAAL and IDNT trials. Eur. Heart J. 32, 1493–1499 (2011).
Ong, K. L., Cheung, B. M., Man, Y. B., Lau, C. P. & Lam, K. S. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 49, 69–75 (2007).
Coresh, J., Astor, B. C., Greene, T., Eknoyan, G. & Levey, A. S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am. J. Kidney Dis. 41, 1–12 (2003).
Bomback, A. S. & Klemmer, P. J. The incidence and implications of aldosterone breakthrough. Nat. Clin. Pract. Nephrol. 3, 486–492 (2007).
Gilbert, K. C. & Brown, N. J. Aldosterone and inflammation. Curr. Opin. Endocrinol. Diabetes Obes. 17, 199–204 (2010).
Epstein, M. Aldosterone as a mediator of progressive renal disease: pathogenetic and clinical implications. Am. J. Kidney Dis. 37, 677–688 (2001).
Waanders, F. et al. Aldosterone, from (patho)physiology to treatment in cardiovascular and renal damage. Curr. Vasc. Pharmacol. 9, 594–605 (2011).
Bianchi, S., Bigazzi, R. & Campese, V. M. Antagonists of aldosterone and proteinuria in patients with CKD: an uncontrolled pilot study. Am. J. Kidney Dis. 46, 45–51 (2005).
Bianchi, S., Bigazzi, R. & Campese, V. M. Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease. Kidney Int. 70, 2116–2123 (2006).
Boesby, L., Elung-Jensen, T., Klausen, T. W., Strandgaard, S. & Kamper, A. L. Moderate antiproteinuric effect of add-on aldosterone blockade with eplerenone in non-diabetic chronic kidney disease. A randomized cross-over study. PLoS ONE 6, e26904 (2011).
Chrysostomou, A. & Becker, G. Spironolactone in addition to ACE inhibition to reduce proteinuria in patients with chronic renal disease. N. Engl. J. Med. 345, 925–926 (2001).
Chrysostomou, A., Pedagogos, E., MacGregor, L. & Becker, G. J. Double-blind, placebo-controlled study on the effect of the aldosterone receptor antagonist spironolactone in patients who have persistent proteinuria and are on long-term angiotensin-converting enzyme inhibitor therapy, with or without an angiotensin II receptor blocker. Clin. J. Am. Soc. Nephrol. 1, 256–262 (2006).
Furumatsu, Y. et al. Effect of renin-angiotensin-aldosterone system triple blockade on non-diabetic renal disease: addition of an aldosterone blocker, spironolactone, to combination treatment with an angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker. Hypertens. Res. 31, 59–67 (2008).
Epstein, M. et al. Selective aldosterone blockade with eplerenone reduces albuminuria in patients with type 2 diabetes. Clin. J. Am. Soc. Nephrol. 1, 940–951 (2006).
González, M. E. et al. Addition of spironolactone to dual blockade of renin angiotensin system dramatically reduces severe proteinuria in renal transplant patients: an uncontrolled pilot study at 6 months. Transplant. Proc. 42, 2899–2901 (2010).
Mehdi, U. F., Adams-Huet, B., Raskin, P., Vega, G. L. & Toto, R. D. Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy. J. Am. Soc. Nephrol. 20, 2641–2650 (2009).
Rachmani, R. et al. The effect of spironolactone, cilazapril and their combination on albuminuria in patients with hypertension and diabetic nephropathy is independent of blood pressure reduction: a randomized controlled study. Diabet. Med. 21, 471–475 (2004).
Rossing, K., Schjoedt, K. J., Smidt, U. M., Boomsma, F. & Parving, H. H. Beneficial effects of adding spironolactone to recommended antihypertensive treatment in diabetic nephropathy: a randomized, double-masked, cross-over study. Diabetes Care 28, 2106–2112 (2005).
Sato, A., Hayashi, K. & Saruta, T. Antiproteinuric effects of mineralocorticoid receptor blockade in patients with chronic renal disease. Am. J. Hypertens. 18, 44–49 (2005).
Schjoedt, K. J. et al. Beneficial impact of spironolactone in diabetic nephropathy. Kidney Int. 68, 2829–2836 (2005).
Schjoedt, K. J. et al. Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy. Kidney Int. 70, 536–542 (2006).
Sengul, E., Sahin, T., Sevin, E. & Yilmaz, A. Effect of spironolactone on urinary protein excretion in patients with chronic kidney disease. Ren. Fail. 31, 928–932 (2009).
Tylicki, L. et al. Triple pharmacological blockade of the renin-angiotensin-aldosterone system in nondiabetic CKD: an open-label crossover randomized controlled trial. Am. J. Kidney Dis. 52, 486–493 (2008).
van den Meiracker, A. H. et al. Spironolactone in type 2 diabetic nephropathy: effects on proteinuria, blood pressure and renal function. J. Hypertens. 24, 2285–2292 (2006).
Sato, A., Hayashi, K., Naruse, M. & Saruta, T. Effectiveness of aldosterone blockade in patients with diabetic nephropathy. Hypertension 41, 64–68 (2003).
Volk, M. J., Bomback, A. S. & Klemmer, P. J. Mineralocorticoid receptor blockade in chronic kidney disease. Curr. Hypertens. Rep. 13, 282–288 (2011).
Levy, D. G., Rocha, R. & Funder, J. W. Distinguishing the antihypertensive and electrolyte effects of eplerenone. J. Clin. Endocrinol. Metab. 89, 2736–2740 (2004).
Mattu, A., Brady, W. J. & Robinson, D. A. Electrocardiographic manifestations of hyperkalemia. Am. J. Emerg. Med. 18, 721–729 (2000).
Desai, A. S. et al. Incidence and predictors of hyperkalemia in patients with heart failure: an analysis of the CHARM Program. J. Am. Coll. Cardiol. 50, 1959–1966 (2007).
Einhorn, L. M. et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch. Intern. Med. 169, 1156–1162 (2009).
Shah, K. B., Rao, K., Sawyer, R. & Gottlieb, S. S. The adequacy of laboratory monitoring in patients treated with spironolactone for congestive heart failure. J. Am. Coll. Cardiol. 46, 845–849 (2005).
Takaichi, K., Takemoto, F., Ubara, Y. & Mori, Y. Analysis of factors causing hyperkalemia. Intern. Med. 46, 823–829 (2007).
Meneton, P., Loffing, J. & Warnock, D. G. Sodium and potassium handling by the aldosterone-sensitive distal nephron: the pivotal role of the distal and connecting tubule. Am. J. Physiol. Renal Physiol. 287, F593–F601 (2004).
Oh, M. S. et al. A mechanism for hyporeninemic hypoaldosteronism in chronic renal disease. Metabolism 23, 1157–1166 (1974).
Schambelan, M., Stockigt, J. R. & Biglieri, E. G. Isolated hypoaldosteronism in adults. A renin-deficiency syndrome. N. Engl. J. Med. 287, 573–578 (1972).
DeFronzo, R. A. Hyperkalemia and hyporeninemic hypoaldosteronism. Kidney Int. 17, 118–134 (1980).
Bakris, G. L. et al. ACE inhibition or angiotensin receptor blockade: impact on potassium in renal failure. VAL-K Study Group. Kidney Int. 58, 2084–2092 (2000).
Csukas, S., Hanke, C. J., Rewolinski, D. & Campbell, W. B. Prostaglandin E2-induced aldosterone release is mediated by an EP2 receptor. Hypertension 31, 575–581 (1998).
Aull, L., Chao, H. & Coy, K. Heparin-induced hyperkalemia. DICP 24, 244–246 (1990).
Mount, D. B. & Zandi-Nejad, K. in Brenner and Rector's The Kidney (ed. Brenner, B. M.) 997–1040 (WB Saunders, Philadelphia, 2004).
Salem, M. M., Rosa, R. M. & Batlle, D. C. Extrarenal potassium tolerance in chronic renal failure: implications for the treatment of acute hyperkalemia. Am. J. Kidney Dis. 18, 421–440 (1991).
Blumberg, A., Weidmann, P., Shaw, S. & Gnädinger, M. Effect of various therapeutic approaches on plasma potassium and major regulating factors in terminal renal failure. Am. J. Med. 85, 507–512 (1988).
Rosa, R. M. et al. Adrenergic modulation of extrarenal potassium disposal. N. Engl. J. Med. 302, 431–434 (1980).
Berl, T., Katz, F. H., Henrich, W. L., de Torrente, A. & Schrier, R. W. Role of aldosterone in the control of sodium excretion in patients with advanced chronic renal failure. Kidney Int. 14, 228–235 (1978).
Schrier, R. W. & Regal, E. M. Influence of aldosterone on sodium, water and potassium metabolism in chronic renal disease. Kidney Int. 1, 156–168 (1972).
Sica, D. A. Diuretic use in renal disease. Nat. Rev. Nephrol. 8, 100–109 (2011).
Perez, G. O., Pelleya, R., Oster, J. R., Kem, D. C. & Vaamonde, C. A. Blunted kaliuresis after an acute potassium load in patients with chronic renal failure. Kidney Int. 24, 656–662 (1983).
Preston, R. A. et al. Mechanisms of impaired potassium handling with dual renin-angiotensin-aldosterone blockade in chronic kidney disease. Hypertension 53, 754–760 (2009).
Musso, C. G. Potassium metabolism in patients with chronic kidney disease (CKD), Part I: patients not on dialysis (stages 3–4). Int. Urol. Nephrol. 36, 465–468 (2004).
Miao, Y. et al. Increased serum potassium affects renal outcomes: a post hoc analysis of the Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan (RENAAL) trial. Diabetologia 54, 44–50 (2011).
Kidney Disease Outcomes Quality Initiative (K/DOQI). (K/DOQI) clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am. J. Kidney Dis. 43, S1–290 (2004).
Gennari, F. J. Hypokalemia. N. Engl. J. Med. 339, 451–458 (1998).
Raymond, C. B., Sood, A. R. & Wazny, L. D. Treatment of hyperkalemia in patients with chronic kidney disease–a focus on medications. CANNT J. 20, 49–53; quiz 54–55 (2010).
Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N. Engl. J. Med. 341, 709–717 (1999).
Pitt, B., Bakris, G., Ruilope, L. M., DiCarlo, L. & Mukherjee, R., EPHESUS Investigators. Serum potassium and clinical outcomes in the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS). Circulation 118, 1643–1650 (2008).
Zannad, F. et al. Eplerenone in patients with systolic heart failure and mild symptoms. N. Engl. J. Med. 364, 11–21 (2011).
Take, C., Ikeda, K., Kurasawa, T. & Kurokawa, K. Increased chloride reabsorption as an inherited renal tubular defect in familial type II pseudohypoaldosteronism. N. Engl. J. Med. 324, 472–476 (1991).
Chacko, M., Fordtran, J. S. & Emmett, M. Effect of mineralocorticoid activity on transtubular potassium gradient, urinary [K]/[Na] ratio, and fractional excretion of potassium. Am. J. Kidney Dis. 32, 47–51 (1998).
Choi, M. J. & Ziyadeh, F. N. The utility of the transtubular potassium gradient in the evaluation of hyperkalemia. J. Am. Soc. Nephrol. 19, 424–426 (2008).
Armanini, D. et al. Aldosterone-receptor deficiency in pseudohypoaldosteronism. N. Engl. J. Med. 313, 1178–1181 (1985).
Kater, C. E. & Biglieri, E. G. Disorders of steroid 17 α-hydroxylase deficiency. Endocrinol. Metab. Clin. North Am. 23, 341–357 (1994).
Clark, B. A., Brown, R. S. & Epstein, F. H. Effect of atrial natriuretic peptide on potassium-stimulated aldosterone secretion: potential relevance to hypoaldosteronism in man. J. Clin. Endocrinol. Metab. 75, 399–403 (1992).
Eudy, R. J. et al. The use of plasma aldosterone and urinary sodium to potassium ratio as translatable quantitative biomarkers of mineralocorticoid receptor antagonism. J. Transl. Med. 9, 180 (2011).
Ramsay, L., Harrison, I., Shelton, J. & Tidd, M. Relative potency of prorenoate and spironolactone in normal man. Clin. Pharmacol. Ther. 18, 391–400 (1975).
Ramsay, L. E., Shelton, J. R. & Tidd, M. J. The pharmacodynamics of single doses of prorenoate potasssium and spironolactone in fludrocortisone treated normal subjects. Br. J. Clin. Pharmacol. 3, 475–482 (1976).
Edmonds, C. J. & Wilson, G. M. The action of hydroflumethiazide in relation to adrenal steroids and potassium loss. Lancet 1, 505–509 (1960).
Eggert, R. C. Spironolactone diuresis in patients with cirrhosis and ascites. Br. Med. J. 4, 401–403 (1970).
Kamel, K. S., Ethier, J. H., Richardson, R. M., Bear, R. A. & Halperin, M. L. Urine electrolytes and osmolality: when and how to use them. Am. J. Nephrol. 10, 89–102 (1990).
Levine, D., Ramsay, L., Auty, R., Branch, R. & Tidd, M. Antagonism of endogenous mineralocorticoids in normal subjects by prorenoate potassium and spironolactone. Eur. J. Clin. Pharmacol. 09, 381–386 (1976).
McInnes, G. T., Perkins, R. M., Shelton, J. R. & Harrison, I. R. Spironolactone dose-response relationships in healthy subjects. Br. J. Clin. Pharmacol. 13, 513–518 (1982).
Ethier, J. H., Kamel, K. S., Magner, P. O., Lemann, J. Jr & Halperin, M. L. The transtubular potassium concentration in patients with hypokalemia and hyperkalemia. Am. J. Kidney Dis. 15, 309–315 (1990).
Rodríguez-Soriano, J., Ubetagoyena, M. & Vallo, A. Transtubular potassium concentration gradient: a useful test to estimate renal aldosterone bio-activity in infants and children. Pediatr. Nephrol. 4, 105–110 (1990).
Mayan, H., Kantor, R. & Farfel, Z. Trans-tubular potassium gradient in patients with drug-induced hyperkalemia. Nephron 89, 56–61 (2001).
Musso, C. et al. Correlation between creatinine clearance and transtubular potassium concentration gradient in old people and chronic renal disease patients. Saudi J. Kidney Dis. Transpl. 18, 551–555 (2007).
Zettle, R. M. et al. Renal potassium handling during states of low aldosterone bio-activity: a method to differentiate renal and non-renal causes. Am. J. Nephrol. 7, 360–366 (1987).
Fujii, H. et al. Life-threatening hyperkalemia during a combined therapy with the angiotensin receptor blocker candesartan and spironolactone. Kobe J. Med. Sci. 51, 1–6 (2005).
Lim, Y. S. et al. Monitoring of transtubular potassium gradient in the diuretic management of patients with cirrhosis and ascites. Liver 22, 426–432 (2002).
Gennari, F. J. & Segal, A. S. Hyperkalemia: an adaptive response in chronic renal insufficiency. Kidney Int. 62, 1–9 (2002).
Raebel, M. A. et al. Diabetes and drug-associated hyperkalemia: effect of potassium monitoring. J. Gen. Intern. Med. 25, 326–333 (2010).
Weir, M. R. & Rolfe, M. Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin. J. Am. Soc. Nephrol. 5, 531–548 (2010).
Lambers Heerspink, H. J., Laverman, G. D., Lewis, J., Parving, H.-H. & de Zeeuw, D. Both hypokalemia and hyperkalemia predict cardiovascular risk during blood pressure lowering therapy in patients with diabetes and nephropathy [abstract # SA-PO2407, 663A]. J. Am. Soc. Nephrol. 21, (2010).
Juurlink, D. N. et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N. Engl. J. Med. 351, 543–551 (2004).
Saudan, P. et al. Safety of low-dose spironolactone administration in chronic haemodialysis patients. Nephrol. Dial. Transplant. 18, 2359–2363 (2003).
Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]). Am. J. Cardiol. 78, 902–907 (1996).
Schjoedt, K. J., Andersen, S., Rossing, P., Tarnow, L. & Parving, H. H. Aldosterone escape during blockade of the renin-angiotensin-aldosterone system in diabetic nephropathy is associated with enhanced decline in glomerular filtration rate. Diabetologia 47, 1936–1939 (2004).
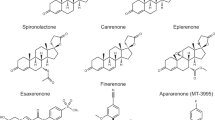
Fagart, J. et al. A new mode of mineralocorticoid receptor antagonism by a potent and selective nonsteroidal molecule. J. Biol. Chem. 285, 29932–29940 (2010).
Nariai, T. et al. SM-368229, a novel selective and potent non-steroidal mineralocorticoid receptor antagonist with strong urinary Na+ excretion activity. J. Pharmacol. Sci. 115, 346–353 (2011).
Nariai, T. et al. Antihypertensive and cardiorenal protective effects of SM-368229, a novel mineralocorticoid receptor antagonist, in aldosterone/salt-treated rats. Pharmacology 89, 44–52 (2012).
Nariai, T. et al. SM-368229, a novel promising mineralocorticoid receptor antagonist, shows anti-hypertensive efficacy with minimal effect on serum potassium level in rats. J. Cardiovasc. Pharmacol. 59, 458–464 (2012).
Lea, W. B. et al. Aldosterone antagonism or synthase inhibition reduces end-organ damage induced by treatment with angiotensin and high salt. Kidney Int. 75, 936–944 (2009).
Rigel, D. F. et al. Pharmacodynamic and pharmacokinetic characterization of the aldosterone synthase inhibitor FAD286 in two rodent models of hyperaldosteronism: comparison with the 11beta-hydroxylase inhibitor metyrapone. J. Pharmacol. Exp. Ther. 334, 232–243 (2010).
Amar, L. et al. Aldosterone synthase inhibition with LCI699: a proof-of-concept study in patients with primary aldosteronism. Hypertension 56, 831–838 (2010).
Calhoun, D. A. et al. Effects of a novel aldosterone synthase inhibitor for treatment of primary hypertension: results of a randomized, double-blind, placebo- and active-controlled phase 2 trial. Circulation 124, 1945–1955 (2011).
Davey, M. & Caldicott, D. Calcium salts in management of hyperkalaemia. Emerg. Med. J. 19, 92–93 (2002).
Sherman, R. A., Hwang, E. R., Bernholc, A. S. & Eisinger, R. P. Variability in potassium removal by hemodialysis. Am. J. Nephrol. 6, 284–288 (1986).
Rastegar, A. & Soleimani, M. Hypokalaemia and hyperkalaemia. Postgrad. Med. J. 77, 759–764 (2001).
Sterns, R. H., Rojas, M., Bernstein, P. & Chennupati, S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J. Am. Soc. Nephrol. 21, 733–735 (2010).
Pitt, B. et al. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur. Heart J. 32, 820–828 (2011).
Pitt, B. et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N. Engl. J. Med. 348, 1309–1321 (2003).
Author information
Authors and Affiliations
Contributions
S. S. Roscioni researched the data for the article, S. S. Roscioni, S. J. L. Bakker and H. J. Lambers Heerspink wrote the manuscript, S. S. Roscioni, D. de Zeeuw, S. J. L. Bakker and H. J. Lambers Heerspink provided substantial contributions to review or editing of the manuscript and discussions of its content before submission.
Corresponding author
Ethics declarations
Competing interests
D. de Zeeuw has consulted for Abbott, Astellas, Bristol–Myers Squibb, Hemocue, Johnson & Johnson, Merck Sharpe & Dohme, Novartis, Reata Pharmaceuticals, and Vitae. H. J. Lambers Heerspink has consulted for Abbott, Johnson & Johnson, Reata Pharmaceuticals and Vitae. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Roscioni, S., de Zeeuw, D., Bakker, S. et al. Management of hyperkalaemia consequent to mineralocorticoid-receptor antagonist therapy. Nat Rev Nephrol 8, 691–699 (2012). https://doi.org/10.1038/nrneph.2012.217
Published:
Issue date:
DOI: https://doi.org/10.1038/nrneph.2012.217
This article is cited by
-
Management of hyperkalemia during treatment with mineralocorticoid receptor blockers: findings from esaxerenone
Hypertension Research (2021)
-
New nonabsorbable potassium-exchange resins in hyperkalaemia
Nature Reviews Nephrology (2015)
-
Minimize drug-induced hyperkalaemia by increasing awareness and using preventative strategies
Drugs & Therapy Perspectives (2015)
-
The effect of RAAS blockade on the progression of diabetic nephropathy
Nature Reviews Nephrology (2014)
-
Drug-Induced Hyperkalemia
Drug Safety (2014)