Key Points
-
Acute kidney injury (AKI) occurs in an estimated one in five adults and one in three children hospitalized with acute illness; the incidence of AKI is increasing
-
Subclinical AKI, defined as elevation in levels of kidney damage biomarkers not fulfilling the conventional criteria for AKI, has characterized a subgroup of patients with increased risk of poor outcome
-
Bedside clinical information systems can enable real-time automated electronic alerting for patients at risk of AKI or who develop early AKI; these systems can be integrated with evidence-based decision support tools
-
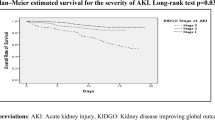
The mortality associated with AKI remains unacceptably high, and increasing severity correlates with increasing mortality, the highest of which is among patients with overt kidney failure requiring renal replacement therapy
-
Reduced health-related quality of life and incident disability are increasingly recognized as important patient-centred outcomes following acute illness complicated by AKI
-
AKI is now recognized as an important risk factor for nonrecovery of kidney function, incident chronic kidney disease, and accelerated progression to end-stage renal disease
Abstract
Acute kidney injury (AKI) is a widespread problem of epidemic status. Compelling evidence indicates that the incidence of AKI is rapidly increasing, particularly among hospitalized patients with acute illness and those undergoing major surgery. This increase might be partially attributable to greater recognition of AKI, improved ascertainment in administrative data and greater sensitivity of consensus diagnostic and classification schemes. Other causes could be an ageing population, increasing incidences of cardiovascular disease, diabetes mellitus and chronic kidney disease (CKD), and an expanding characterization of modifiable risk factors, such as sepsis, administration of contrast media and exposure to nephrotoxins. The sequelae of AKI are severe and characterized by increased risk of short-term and long-term mortality, incident CKD and accelerated progression to end-stage renal disease. AKI-associated mortality is decreasing, but remains unacceptably high. Moreover, the absolute number of patients dying as a result of AKI is increasing as the incidence of the disorder increases, and few proven effective preventative or therapeutic interventions exist. Survivors of AKI, particularly those who remain on renal replacement therapy, often have reduced quality of life and consume substantially greater health-care resources than the general population as a result of longer hospitalizations, unplanned intensive care unit admissions and rehospitalizations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bellomo, R. The epidemiology of acute renal failure: 1975 versus 2005. Curr. Opin. Crit. Care 12, 557–560 (2006).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clin. J. Am. Soc. Nephrol. 8, 1482–1493 (2013).
Uchino, S. The epidemiology of acute renal failure in the world. Curr. Opin. Crit. Care 12, 538–543 (2006).
Lameire, N. H. et al. Acute kidney injury: an increasing global concern. Lancet 382, 170–179 (2013).
Xue, J. L. et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J. Am. Soc. Nephrol. 17, 1135–1142 (2006).
Waikar, S. S., Curhan, G. C., Wald, R., McCarthy, E. P. & Chertow, G. M. Declining mortality in patients with acute renal failure, 1988 to 2002. J. Am. Soc. Nephrol. 17, 1143–1150 (2006).
Kellum, J. A., Bellomo, R. & Ronco, C. Kidney attack. JAMA 307, 2265–2266 (2012).
Li, P. K. et al. Acute kidney injury: global health alert. Kidney Int. 83, 372–376 (2013).
Hoste, E. A. et al. The epidemiology of cardiac surgery-associated acute kidney injury. Int. J. Artif. Organs 31, 158–165 (2008).
Bellomo, R. et al. Acute renal failure–definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit. Care 8, R204–R212 (2004).
Mehta, R. L. et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit. Care 11, R31 (2007).
Kellum, J. A., Levin, N., Bouman, C. & Lameire, N. Developing a consensus classification system for acute renal failure. Curr. Opin. Crit. Care 8, 509–514 (2002).
Kidney Disease Improving Global Outcomes. KDIGO clinical practice guidelines on acute kidney injury. Kidney Int. Suppl. 2, 8–12 (2012).
Ricci, Z., Cruz, D. & Ronco, C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 73, 538–546 (2008).
Bagshaw, S. M. et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit. Care 9, R700–R709 (2005).
de Mendonca, A. et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 26, 915–921 (2000).
Bagshaw, S. M. et al. A comparison of observed versus estimated baseline creatinine for determination of RIFLE class in patients with acute kidney injury. Nephrol. Dial. Transplant. 24, 2739–2744 (2009).
Zavada, J. et al. A comparison of three methods to estimate baseline creatinine for RIFLE classification. Nephrol. Dial. Transplant. 25, 3911–3918 (2010).
Siew, E. D. et al. Use of multiple imputation method to improve estimation of missing baseline serum creatinine in acute kidney injury research. Clin. J. Am. Soc. Nephrol. 8, 10–18 (2013).
Pickering, J. W. & Endre, Z. H. Back-calculating baseline creatinine with MDRD misclassifies acute kidney injury in the intensive care unit. Clin. J. Am. Soc. Nephrol. 5, 1165–1173 (2010).
Pickering, J. W. & Endre, Z. H. GFR shot by RIFLE: errors in staging acute kidney injury. Lancet 373, 1318–1319 (2009).
Doi, K. et al. Reduced production of creatinine limits its use as marker of kidney injury in sepsis. J. Am. Soc. Nephrol. 20, 1217–1221 (2009).
Liu, K. D. et al. Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit. Care Med. 39, 2665–2671 (2011).
Macedo, E. et al. Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit. Care 14, R82 (2010).
Pickering, J. W., Ralib, A. M. & Endre, Z. H. Combining creatinine and volume kinetics identifies missed cases of acute kidney injury following cardiac arrest. Crit. Care 17, R7 (2013).
Macedo, E., Malhotra, R., Bouchard, J., Wynn, S. K. & Mehta, R. L. Oliguria is an early predictor of higher mortality in critically ill patients. Kidney Int. 80, 760–767 (2011).
Mandelbaum, T. et al. Empirical relationships among oliguria, creatinine, mortality, and renal replacement therapy in the critically ill. Intensive Care Med. 39, 414–419 (2013).
Prowle, J. R. et al. Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit. Care 15, R172 (2011).
Macedo, E., Malhotra, R., Claure- Del Granado, R., Fedullo, P. & Mehta, R. L. Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol. Dial. Transplant. 26, 509–515 (2011).
Ralib, A. M., Pickering, J. W., Shaw, G. M. & Endre, Z. H. The urine output definition of acute kidney injury is too liberal. Crit. Care 17, R112 (2013).
McCullough, P. A. et al. Implementation of novel biomarkers in the diagnosis, prognosis, and management of acute kidney injury: executive summary from the tenth consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib. Nephrol. 182, 5–12 (2013).
Bagshaw, S. M., Zappitelli, M. & Chawla, L. S. Novel biomarkers of AKI: the challenges of progress 'amid the noise and the haste'. Nephrol. Dial. Transplant. 28, 235–238 (2013).
Parikh, C. R. et al. Postoperative biomarkers predict acute kidney injury and poor outcomes after pediatric cardiac surgery. J. Am. Soc. Nephrol. 22, 1737–1747 (2011).
Siew, E. D. et al. Distinct injury markers for the early detection and prognosis of incident acute kidney injury in critically ill adults with preserved kidney function. Kidney Int. 84, 786–794 (2013).
Nickolas, T. L. et al. Diagnostic and prognostic stratification in the emergency department using urinary biomarkers of nephron damage: a multicenter prospective cohort study. J. Am. Coll. Cardiol. 59, 246–255 (2012).
Nickolas, T. L. et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann. Intern. Med. 148, 810–819 (2008).
Kashani, K. et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit. Care 17, R25 (2013).
Bagshaw, S. M. Subclinical acute kidney injury: a novel biomarker-defined syndrome. Crit. Care Resusc. 13, 201–203 (2011).
Haase, M., Kellum, J. A. & Ronco, C. Subclinical AKI—an emerging syndrome with important consequences. Nat. Rev. Nephrol. 8, 735–739 (2012).
Haase, M. et al. The outcome of neutrophil gelatinase-associated lipocalin-positive subclinical acute kidney injury: a multicenter pooled analysis of prospective studies. J. Am. Coll. Cardiol. 57, 1752–1761 (2011).
Colpaert, K. et al. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit. Care Med. 40, 1164–1170 (2012).
Brown, J. R., Kramer, R. S., Coca, S. G. & Parikh, C. R. The prognostic value of using the duration of acute kidney injury in cardiac surgery: an example using two antifibrinolytics. J. Extra Corpor. Technol. 43, 227–231 (2011).
Goldstein, S. L. et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132, e756–e767 (2013).
Selby, N. M. et al. Use of electronic results reporting to diagnose and monitor AKI in hospitalized patients. Clin. J. Am. Soc. Nephrol. 7, 533–540 (2012).
Hsu, C. Y. et al. Community-based incidence of acute renal failure. Kidney Int. 72, 208–212 (2007).
Liangos, O. et al. Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin. J. Am. Soc. Nephrol. 1, 43–51 (2006).
Swaminathan, M. et al. Trends in acute renal failure associated with coronary artery bypass graft surgery in the United States. Crit. Care Med. 35, 2286–2291 (2007).
Fujii, T., Uchino, S., Takinami, M. & Bellomo, R. Subacute kidney injury in hospitalized patients. Clin. J. Am. Soc. Nephrol. http://dx.doi.org/10.2215/CJN.04120413.
Waikar, S. S. et al. Validity of international classification of diseases, ninth revision, clinical modification codes for acute renal failure. J. Am. Soc. Nephrol. 17, 1688–1694 (2006).
Hwang, Y. J. et al. Validity of the international classification of diseases, tenth revision code for acute kidney injury in elderly patients at presentation to the emergency department and at hospital admission. BMJ Open 2, e001821 (2012).
Ali, T. et al. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J. Am. Soc. Nephrol. 18, 1292–1298 (2007).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16, 3365–3370 (2005).
Lassnigg, A. et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J. Am. Soc. Nephrol. 15, 1597–1605 (2004).
Hou, S. H., Bushinsky, D. A., Wish, J. B., Cohen, J. J. & Harrington, J. T. Hospital-acquired renal insufficiency: a prospective study. Am. J. Med. 74, 243–248 (1983).
Nash, K., Hafeez, A. & Hou, S. Hospital-acquired renal insufficiency. Am. J. Kidney Dis. 39, 930–936 (2002).
Uchino, S., Bellomo, R., Goldsmith, D., Bates, S. & Ronco, C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit. Care Med. 34, 1913–1917 (2006).
Hsu, R. K., McCulloch, C. E., Dudley, R. A., Lo, L. J. & Hsu, C. Y. Temporal changes in incidence of dialysis-requiring AKI. J. Am. Soc. Nephrol. 24, 37–42 (2013).
Siddiqui, N. F. et al. Secular trends in acute dialysis after elective major surgery—1995 to 2009. CMAJ 184, 1237–1245 (2012).
Andrikos, E. et al. Epidemiology of acute renal failure in ICUs: a multi-center prospective study. Blood Purif. 28, 239–244 (2009).
Bagshaw, S. M. et al. Changes in the incidence and outcome for early acute kidney injury in a cohort of Australian intensive care units. Crit. Care 11, R68 (2007).
Bagshaw, S. M., George, C., Dinu, I. & Bellomo, R. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol. Dial. Transplant. 23, 1203–1210 (2008).
Medve, L. et al. Epidemiology of acute kidney injury in Hungarian intensive care units: a multicenter, prospective, observational study. BMC Nephrol. 12, 43 (2011).
Nisula, S. et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med. 39, 420–428 (2013).
Piccinni, P. et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol. 77, 1072–1083 (2011).
Poukkanen, M. et al. Acute kidney injury in patients with severe sepsis in Finnish intensive care units. Acta Anaesthesiol. Scand. 57, 863–872 (2013).
Thakar, C. V., Christianson, A., Freyberg, R., Almenoff, P. & Render, M. L. Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study. Crit. Care Med. 37, 2552–2558 (2009).
Ostermann, M. & Chang, R. W. Acute kidney injury in the intensive care unit according to RIFLE. Crit. Care Med. 35, 1837–1843 (2007).
Uchino, S. et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294, 813–818 (2005).
Hoste, E. A. et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit. Care 10, R73 (2006).
Clec'h, C. et al. Multiple-center evaluation of mortality associated with acute kidney injury in critically ill patients: a competing risks analysis. Crit. Care 15, R128 (2011).
Vaara, S. et al. Population-based incidence, mortality and quality of life in critically ill patients treated with renal replacement therapy—a nationwide retrospective cohort study in Finnish ICUs. Crit. Care 16, R13 (2012).
Riley, S. et al. Renal impairment among acute hospital admissions in a rural Ethiopian hospital. Nephrology (Carlton) 18, 92–96 (2013).
Xuan, B. H. et al. Swarming hornet attacks: shock and acute kidney injury—a large case series from Vietnam. Nephrol. Dial. Transplant. 25, 1146–1150 (2010).
Khakurel, S., Satyal, P. R., Agrawal, R. K., Chhetri, P. K. & Hada, R. Acute renal failure in a tertiary care center in Nepal. J. Nepal Med. Assoc. 44, 32–35 (2005).
Soliman, A. R. Spectrum of acute kidney injury in a tertiary care hospital in Cairo. Arab J. Nephrol. Transplant. 4, 83–86 (2011).
Daher, E. F. et al. Leptospirosis-associated acute kidney injury: penicillin at the late stage is still controversial. J. Clin. Pharm. Ther. 37, 420–425 (2012).
Liborio, A. B. et al. Acute kidney injury in children with visceral leishmaniasis. Pediatr. Infect. Dis. J. 31, 451–454 (2012).
Krishnamurthy, S. et al. Incidence and etiology of acute kidney injury in southern India. Indian J. Pediatr. 80, 183–189 (2013).
Shukla, V. S., Singh, R. G., Rathore, S. S. & Usha . Outcome of malaria-associated acute kidney injury: a prospective study from a single center. Ren. Fail. 35, 801–805 (2013).
Lombardi, R., Yu, L., Younes-Ibrahim, M., Schor, N. & Burdmann, E. A. Epidemiology of acute kidney injury in Latin America. Semin. Nephrol. 28, 320–329 (2008).
Phillips, L. A. et al. Acute kidney injury risk factor recognition in three teaching hospitals in Ethiopia. S. Afr. Med. J. 103, 413–418 (2013).
Coca, S. G., Cho, K. C. & Hsu, C. Y. Acute kidney injury in the elderly: predisposition to chronic kidney disease and vice versa. Nephron Clin. Pract. 119 (Suppl. 1), c19–c24 (2011).
Ishani, A. et al. Acute kidney injury increases risk of ESRD among elderly. J. Am. Soc. Nephrol. 20, 223–228 (2009).
Boumendil, A. et al. Treatment intensity and outcome of patients aged 80 and older in intensive care units: a multicenter matched-cohort study. J. Am. Geriatr. Soc. 53, 88–93 (2005).
Bagshaw, S. M. et al. Association between renal replacement therapy in critically ill patients with severe acute kidney injury and mortality. J. Crit. Care 28, 1011–1018 (2013).
Ball, E. F. & Kara, T. Epidemiology and outcome of acute kidney injury in New Zealand children. J. Paediatr. Child Health 44, 642–646 (2008).
James, M. T. et al. Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: a cohort study. Lancet 376, 2096–2103 (2010).
Grams, M. E. et al. Albuminuria and estimated glomerular filtration rate independently associate with acute kidney injury. J. Am. Soc. Nephrol. 21, 1757–1764 (2010).
Coca, S. G. et al. Preoperative proteinuria predicts acute kidney injury in patients undergoing cardiac surgery. J. Thorac. Cardiovasc. Surg. 143, 495–502 (2012).
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351, 1296–1305 (2004).
Cho, K. & Hsu, C. Y. Quantifying severity of chronic kidney disease as a risk factor for acute kidney injury. J. Am. Soc. Nephrol. 21, 1602–1604 (2010).
Lafrance, J. P., Djurdjev, O. & Levin, A. Incidence and outcomes of acute kidney injury in a referred chronic kidney disease cohort. Nephrol. Dial. Transplant. 25, 2203–2209 (2010).
Kheterpal, S. et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology 110, 505–515 (2009).
Huen, S. C. & Parikh, C. R. Predicting acute kidney injury after cardiac surgery: a systematic review. Ann. Thorac. Surg. 93, 337–347 (2012).
Mehta, R. H. et al. Bedside tool for predicting the risk of postoperative dialysis in patients undergoing cardiac surgery. Circulation 114, 2208–2216 (2006).
Thakar, C. V., Arrigain, S., Worley, S., Yared, J. P. & Paganini, E. P. A clinical score to predict acute renal failure after cardiac surgery. J. Am. Soc. Nephrol. 16, 162–168 (2005).
Benko, A. et al. Canadian association of radiologists: consensus guidelines for the prevention of contrast-induced nephropathy. Can. Assoc. Radiol. J. 58, 79–87 (2007).
Schneider, V., Levesque, L. E., Zhang, B., Hutchinson, T. & Brophy, J. M. Association of selective and conventional nonsteroidal antiinflammatory drugs with acute renal failure: a population-based, nested case-control analysis. Am. J. Epidemiol. 164, 881–889 (2006).
Bird, S. T., Etminan, M., Brophy, J. M., Hartzema, A. G. & Delaney, J. A. Risk of acute kidney injury associated with the use of fluoroquinolones. CMAJ 185, E475–E482 (2013).
Dormuth, C. R. et al. Use of high potency statins and rates of admission for acute kidney injury: multicenter, retrospective observational analysis of administrative databases. BMJ 346, f880 (2013).
Leonard, C. E. et al. Proton pump inhibitors and traditional nonsteroidal anti-inflammatory drugs and the risk of acute interstitial nephritis and acute kidney injury. Pharmacoepidemiol. Drug Saf. 21, 1155–1172 (2012).
Sorli, L. et al. Trough colistin plasma level is an independent risk factor for nephrotoxicity: a prospective observational cohort study. BMC Infect. Dis. 13, 380 (2013).
Wikman, P. et al. The significance of antiretroviral-associated acute kidney injury in a cohort of ambulatory human immunodeficiency virus-infected patients. Nephrol. Dial. Transplant. 28, 2073–2081 (2013).
Zhao, Y. Y. et al. New fibrate use and acute renal outcomes in elderly adults: a population-based study. Ann. Intern. Med. 156, 560–569 (2012).
Cox, Z. L. et al. Adverse drug events during AKI and its recovery. Clin. J. Am. Soc. Nephrol. 8, 1070–1078 (2013).
Zappitelli, M., Moffett, B. S., Hyder, A. & Goldstein, S. L. Acute kidney injury in non-critically ill children treated with aminoglycoside antibiotics in a tertiary healthcare centre. Nephrol. Dial. Transplant. 26, 144–150 (2011).
Herrera-Gutierrez, M. E., Seller-Perez, G., Sanchez- Izquierdo-Riera, J. A. & Maynar-Moliner, J. Prevalence of acute kidney injury in intensive care units: the “COrte de prevalencia de disFuncion RenAl y DEpuracion en criticos” point-prevalence multicenter study. J. Crit. Care 28, 687–694 (2013).
Ramirez, E. et al. Vancomycin-induced acute kidney injury detected by a prospective pharmacovigilance program from laboratory signals. Ther. Drug Monit. 35, 360–366 (2013).
Wunderink, R. G. et al. Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin. Infect. Dis. 54, 621–629 (2012).
Hoste, E. A. et al. Epidemiology of contrast-associated acute kidney injury in ICU patients: a retrospective cohort analysis. Intensive Care Med. 37, 1921–1931 (2011).
Kheterpal, S. et al. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology 107, 892–902 (2007).
Ho, J. et al. Serum creatinine measurement immediately after cardiac surgery and prediction of acute kidney injury. Am. J. Kidney Dis. 59, 196–201 (2012).
Bastin, A. J. et al. Acute kidney injury after cardiac surgery according to risk/injury/failure/loss/end-stage, acute kidney injury network, and kidney disease: improving global outcomes classifications. J. Crit. Care 28, 389–396 (2013).
Swaminathan, M. et al. Impact of early renal recovery on survival after cardiac surgery-associated acute kidney injury. Ann. Thorac. Surg. 89, 1098–1104 (2010).
Kuitunen, A., Vento, A., Suojaranta-Ylinen, R. & Pettila, V. Acute renal failure after cardiac surgery: evaluation of the RIFLE classification. Ann. Thorac. Surg. 81, 542–546 (2006).
Chertow, G. M., Levy, E. M., Hammermeister, K. E., Grover, F. & Daley, J. Independent association between acute renal failure and mortality following cardiac surgery. Am. J. Med. 104, 343–348 (1998).
Bagshaw, S. M. et al. Early acute kidney injury and sepsis: a multicentre evaluation. Crit. Care 12, R47 (2008).
Murugan, R. et al. Acute kidney injury in non-severe pneumonia is associated with an increased immune response and lower survival. Kidney Int. 77, 527–535 (2010).
Bagshaw, S. M. et al. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 35, 871–881 (2009).
Mehta, R. L. et al. Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med. 37, 241–248 (2011).
Brunkhorst, F. M. et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N. Engl. J. Med. 358, 125–139 (2008).
Myburgh, J. A. et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N. Engl. J. Med. 367, 1901–1911 (2012).
Perner, A. et al. Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis. N. Engl. J. Med. 367, 124–134 (2012).
Shaw, A. D. et al. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann. Surgery 255, 821–829 (2012).
Yunos, N. M. et al. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA 308, 1566–1572 (2012).
Yunos, N. M. et al. The biochemical effects of restricting chloride-rich fluids in intensive care. Crit. Care Med. 39, 2419–2424 (2011).
Chowdhury, A. H., Cox, E. F., Francis, S. T. & Lobo, D. N. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and Plasma-Lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann. Surg. 256, 18–24 (2012).
Grams, M. E. et al. Fluid balance, diuretic use, and mortality in acute kidney injury. Clin. J. Am. Soc. Nephrol. 6, 966–973 (2011).
Payen, D. et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit. Care 12, R74 (2008).
Bouchard, J. et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 76, 422–427 (2009).
Vaara, S. T. et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit. Care 16, R197 (2012).
Goldberg, A. & Hammerman, H. In hospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am. Heart J. 150, 330–337 (2005).
Anzai, A. et al. Prognostic significance of acute kidney injury after reperfused ST-elevation myocardial infarction: synergistic acceleration of renal dysfunction and left ventricular remodeling. J. Card. Fail. 16, 381–389 (2010).
Marenzi, G. et al. Acute kidney injury in ST-segment elevation acute myocardial infarction complicated by cardiogenic shock at admission. Crit. Care Med. 38, 438–444 (2010).
Fonarow, G. C. et al. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA 293, 572–580 (2005).
Abelha, F. J., Botelho, M., Fernandes, V. & Barros, H. Outcome and quality of life of patients with acute kidney injury after major surgery. Nefrologia 29, 404–414 (2009).
Bagshaw, S. M., George, C., Gibney, R. T. & Bellomo, R. A multi-center evaluation of early acute kidney injury in critically ill trauma patients. Ren. Fail. 30, 581–589 (2008).
Lafrance, J. P. & Miller, D. R. Acute kidney injury associates with increased long-term mortality. J. Am. Soc. Nephrol. 21, 345–352 (2010).
Wald, R. et al. Risk of chronic dialysis and death following acute kidney injury. Am. J. Med. 125, 585–593 (2012).
Wu, V. C. et al. Acute-on-chronic kidney injury at hospital discharge is associated with long-term dialysis and mortality. Kidney Int. 80, 1222–1230 (2011).
Palevsky, P. M. et al. Intensity of renal support in critically ill patients with acute kidney injury. N. Engl. J. Med. 359, 7–20 (2008).
The RENAL Replacement Therapy Study Investigators. Intensity of continuous renal-replacement therapy in critically ill patients. N. Engl. J. Med. 361, 1627–1638 (2009).
Selby, N. M. et al. Defining the cause of death in hospitalised patients with acute kidney injury. PLoS ONE 7, e48580 (2012).
Bell, M. et al. Continuous renal replacement therapy is associated with less chronic renal failure than intermittent haemodialysis after acute renal failure. Intensive Care Med. 33, 773–780 (2007).
Korkeila, M., Ruokonen, E. & Takala, J. Costs of care, long-term prognosis and quality of life in patients requiring renal replacement therapy during intensive care. Intensive Care Med. 26, 1824–1831 (2000).
Silvester, W., Bellomo, R. & Cole, L. Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit. Care Med. 29, 1910–1915 (2001).
Schmitt, R. et al. Recovery of kidney function after acute kidney injury in the elderly: a systematic review and meta-analysis. Am. J. Kidney Dis. 52, 262–271 (2008).
Hsu, C. Y. et al. Nonrecovery of kidney function and death after acute on chronic renal failure. Clin. J. Am. Soc. Nephrol. 4, 891–898 (2009).
Chawla, L. S., Amdur, R. L., Amodeo, S., Kimmel, P. L. & Palant, C. E. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 79, 1361–1369 (2011).
Thakar, C. V., Christianson, A., Himmelfarb, J. & Leonard, A. C. Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin. J. Am. Soc. Nephrol. 6, 2567–2572 (2011).
Srisawat, N. et al. Plasma neutrophil gelatinase-associated lipocalin predicts recovery from acute kidney injury following community-acquired pneumonia. Kidney Int. 80, 545–552 (2011).
Sutherland, S. M. et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am. J. Kidney Dis. 55, 316–325 (2009).
Heung, M. et al. Fluid overload at initiation of renal replacement therapy is associated with lack of renal recovery in patients with acute kidney injury. Nephrol. Dial. Transplant. 27, 956–961 (2012).
Karvellas, C. J. et al. A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit. Care 15, R72 (2011).
Smith, O. M. et al. Standard versus accelerated initiation of renal replacement therapy in acute kidney injury (STARRT-AKI): study protocol for a randomized controlled trial. Trials 14, 320 (2013).
Cartin-Ceba, R. et al. Evaluation of “loss” and “end stage renal disease” after acute kidney injury defined by the risk, injury, failure, loss and ESRD classification in critically ill patients. Intensive Care Med. 35, 2087–2095 (2009).
Jacka, M. J., Ivancinova, X. & Gibney, R. T. Continuous renal replacement therapy improves renal recovery from acute renal failure. Can. J. Anaesth. 52, 327–332 (2005).
Lin, Y. F. et al. The 90-day mortality and the subsequent renal recovery in critically ill surgical patients requiring acute renal replacement therapy. Am. J. Surg. 198, 325–332 (2009).
Mehta, R. L. et al. A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int. 60, 1154–1163 (2001).
Schneider, A. G. et al. Choice of renal replacement therapy modality and dialysis dependence after acute kidney injury: a systematic review and meta-analysis. Intensive Care Med. 39, 987–997 (2013).
Uchino, S. et al. Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int. J. Artif. Organs 30, 281–292 (2007).
Wald, R. et al. The association between renal replacement therapy modality and long-term outcomes among critically ill adults with acute kidney injury: a retrospective cohort study. Crit. Care Med. http://dx.doi.org/10.1097/CCM.0000000000000042.
Coca, S. G., Singanamala, S. & Parikh, C. R. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 81, 442–448 (2012).
Pannu, N. et al. Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin. J. Am. Soc. Nephrol. 8, 194–202 (2013).
Hamel, M. B. et al. Outcomes and cost-effectiveness of initiating dialysis and continuing aggressive care in seriously ill hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann. Intern. Med. 127, 195–202 (1997).
Ahlstrom, A., Tallgren, M., Peltonen, S., Rasanen, P. & Pettila, V. Survival and quality of life of patients requiring acute renal replacement therapy. Intensive Care Med. 31, 1222–1228 (2005).
Delannoy, B. et al. Six-month outcome in acute kidney injury requiring renal replacement therapy in the ICU: a multicentre prospective study. Intensive Care Med. 35, 1907–1915 (2009).
Hofhuis, J. G., van Stel, H. F., Schrijvers, A. J., Rommes, J. H. & Spronk, P. E. The effect of acute kidney injury on long-term health-related quality of life: a prospective follow-up study. Crit. Care 17, R17 (2013).
Johansen, K. L. et al. Predictors of health utility among 60-day survivors of acute kidney injury in the Veterans Affairs/National Institutes of Health acute renal failure trial network study. Clin. J. Am. Soc. Nephrol. 5, 1366–1372 (2010).
Joyce, V. R. et al. Health-related quality of life as a predictor of mortality among survivors of AKI. Clin. J. Am. Soc. Nephrol. 7, 1063–1070 (2012).
Morsch, C., Thome, F. S., Balbinotto, A., Guimaraes, J. F. & Barros, E. G. Health-related quality of life and dialysis dependence in critically ill patient survivors of acute kidney injury. Ren. Fail. 33, 949–956 (2011).
Fischer, M. J., Brimhall, B. B., Lezotte, D. C., Glazner, J. E. & Parikh, C. R. Uncomplicated acute renal failure and hospital resource utilization: a retrospective multicenter analysis. Am. J. Kidney Dis. 46, 1049–1057 (2005).
Pan, S. W. et al. Acute kidney injury on ventilator initiation day independently predicts prolonged mechanical ventilation in intensive care unit patients. J. Crit. Care 26, 586–592 (2011).
Vieira, J. M. Jr et al. Effect of acute kidney injury on weaning from mechanical ventilation in critically ill patients. Crit. Care Med. 35, 184–191 (2007).
Dasta, J. F., Kane-Gill, S. L., Durtschi, A. J., Pathak, D. S. & Kellum, J. A. Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol. Dial. Transplant. 23, 1970–1974 (2008).
Elseviers, M. M. et al. Renal replacement therapy is an independent risk factor for mortality in critically ill patients with acute kidney injury. Crit. Care 14, R221 (2010).
Vaara, S. T. et al. Association of ICU size and annual case volume of renal replacement therapy patients with mortality. Acta Anaesthesiol. Scand. 56, 1175–1182 (2012).
Farese, S., Jakob, S. M., Kalicki, R., Frey, F. J. & Uehlinger, D. E. Treatment of acute renal failure in the intensive care unit: lower costs by intermittent dialysis than continuous venovenous hemodiafiltration. Artif. Organs 33, 634–640 (2009).
Manns, B. et al. Cost of acute renal failure requiring dialysis in the intensive care unit: clinical and resource implications of renal recovery. Crit. Care Med. 31, 449–455 (2003).
Rauf, A. A. et al. Intermittent hemodialysis versus continuous renal replacement therapy for acute renal failure in the intensive care unit: an observational outcomes analysis. J. Intensive Care Med. 23, 195–203 (2008).
Srisawat, N. et al. Cost of acute renal replacement therapy in the intensive care unit: results from the beginning and ending supportive therapy for the kidney (BEST Kidney) study. Crit. Care 14, R46 (2010).
Berbece, A. N. & Richardson, R. M. Sustained low-efficiency dialysis in the ICU: cost, anticoagulation, and solute removal. Kidney Int. 70, 963–968 (2006).
Fieghen, H. E. et al. The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol. 11, 32 (2010).
Chionh, C. Y., Soni, S. S., Finkelstein, F. O., Ronco, C. & Cruz, D. N. Use of peritoneal dialysis in AKI: a systematic review. Clin. J. Am. Soc. Nephrol. 8, 1649–1660 (2013).
Phu, N. H. et al. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N. Engl. J. Med. 347, 895–902 (2002).
Bazari, H. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure. N. Engl. J. Med. 348, 858–860 (2003).
Daugirdas, J. T. Peritoneal dialysis in acute renal failure--why the bad outcome? N. Engl. J. Med. 347, 933–935 (2002).
Gabriel, D. P. et al. High volume peritoneal dialysis for acute renal failure. Perit. Dial. Int. 27, 277–282 (2007).
Ponce, D., Berbel, M. N., Abrao, J. M., Goes, C. R. & Balbi, A. L. A randomized clinical trial of high volume peritoneal dialysis versus extended daily hemodialysis for acute kidney injury patients. Int. Urol. Nephrol. 45, 869–878 (2013).
Ponce, D., Berbel, M. N., Regina de Goes, C., Almeida, C. T. & Balbi, A. L. High-volume peritoneal dialysis in acute kidney injury: indications and limitations. Clin. J. Am. Soc. Nephrol. 7, 887–894 (2012).
Callegari, J. G. et al. Peritoneal dialysis for acute kidney injury in sub-Saharan Africa: challenges faced and lessons learned at Kilimanjaro Christian Medical Centre. Kidney Int. 81, 331–333 (2012).
Laukkanen, A., Emaus, L., Pettila, V. & Kaukonen, K. M. Five-year cost-utility analysis of acute renal replacement therapy: a societal perspective. Intensive Care Med. 39, 406–413 (2013).
Wald, R. et al. Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA 302, 1179–1185 (2009).
Honeycutt, A. A. et al. Medical costs of CKD in the medicare population. J. Am. Soc. Nephrol. 24, 1478–1483 (2013).
Manns, B. J., Mendelssohn, D. C. & Taub, K. J. The economics of end-stage renal disease care in Canada: incentives and impact on delivery of care. Int. J. Health Care Finance Econ. 7, 149–169 (2007).
Baboolal, K. et al. The cost of renal dialysis in a UK setting—a multicentre study. Nephrol. Dial. Transplant. 23, 1982–1989 (2008).
Foley, R. N. & Collins, A. J. End-stage renal disease in the United States: an update from the United States Renal Data System. J. Am. Soc. Nephrol. 18, 2644–2648 (2007).
Blake, C., Codd, M. B., Cassidy, A. & O'Meara, Y. M. Physical function, employment and quality of life in end-stage renal disease. J. Nephrol. 13, 142–149 (2000).
Blake, C. & O'Meara, Y. M. Subjective and objective physical limitations in high-functioning renal dialysis patients. Nephrol. Dial. Transplant. 19, 3124–3129 (2004).
Mammen, C. et al. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am. J. Kidney Dis. 59, 523–530 (2012).
Tjaden, L., Tong, A., Henning, P., Groothoff, J. & Craig, J. C. Children's experiences of dialysis: a systematic review of qualitative studies. Arch. Dis. Child. 97, 395–402 (2012).
Tong, A. et al. Quality of life of young adults and adolescents with chronic kidney disease. J. Pediatr. 163, 1179–1185 e5 (2013).
Forman, D. E. et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J. Am. Coll. Cardiol. 43, 61–67 (2004).
Newsome, B. B. et al. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch. Intern. Med. 168, 609–616 (2008).
Yegenaga, I. et al. Clinical characteristics of patients developing ARF due to sepsis/systemic inflammatory response syndrome: results of a prospective study. Am. J. Kidney Dis. 43, 817–824 (2004).
Oppert, M. et al. Acute renal failure in patients with severe sepsis and septic shock—a significant independent risk factor for mortality: results from the German prevalence study. Nephrol. Dial. Transplant. 23, 904–909 (2007).
Gettings, L. G., Reynolds, H. N. & Scalea, T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med. 25, 805–813 (1999).
Van Biesen, W. et al. Relationship between fluid status and its management on acute renal failure (ARF) in intensive care unit (ICU) patients with sepsis: a prospective analysis. J. Nephrol. 18, 54–60 (2005).
Maitland, K. et al. Mortality after fluid bolus in African children with severe infection. N. Engl. J. Med. 364, 2483–2495 (2011).
Gattas, D. J. et al. Fluid resuscitation with 6% hydroxyethyl starch (130/0.4) in acutely ill patients: an updated systematic review and meta-analysis. Anesth. Analg. 114, 159–169 (2012).
Zarychanski, R. et al. Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 309, 678–688 (2013).
O'Malley, C. M. et al. A randomized, double-blind comparison of lactated Ringer's solution and 0.9% NaCl during renal transplantation. Anesth. Analg. 100, 1518–1524 (2005).
Radaelli, G. et al. The use of inhibitors of angiotensin-converting enzyme and its relation to events in the postoperative period of CABG. Rev. Bras. Cir. Cardiovasc. 26, 373–379 (2011).
Centers for Disease Control and Prevention. Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb. Mortal. Wkly Rep. 62, 93–98 (2013).
Martinelli, S. M. et al. Trends in cardiac surgery-associated acute renal failure in the United States: a disproportionate increase after heart transplantation. Ren. Fail. 31, 633–640 (2009).
Acknowledgements
S. M. Bagshaw holds a Canada Research Chair in Critical Care Nephrology and his research is supported by a Clinical Investigator Award from Alberta Innovates–Health Solutions.
Author information
Authors and Affiliations
Contributions
Both authors researched the data for the article, contributed to discussions of the content, wrote the article and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S. M. Bagshaw has consulted for Alere Inc, Baxter Inc and Gambro Inc. O. Rewa declares no competing interests.
Rights and permissions
About this article
Cite this article
Rewa, O., Bagshaw, S. Acute kidney injury—epidemiology, outcomes and economics. Nat Rev Nephrol 10, 193–207 (2014). https://doi.org/10.1038/nrneph.2013.282
Published:
Issue date:
DOI: https://doi.org/10.1038/nrneph.2013.282
This article is cited by
-
Seasonality of acute kidney injury phenotypes in England: an unsupervised machine learning classification study of electronic health records
BMC Nephrology (2023)
-
Use of novel structural features to identify urinary biomarkers during acute kidney injury that predict progression to chronic kidney disease
BMC Nephrology (2023)
-
Risk factors associated with acute kidney injury in a pediatric intensive care unit in Addis Ababa Ethiopia: case-control study
BMC Nephrology (2023)
-
Optimization strategies of mesenchymal stem cell-based therapy for acute kidney injury
Stem Cell Research & Therapy (2023)
-
Amlodipine alleviates renal ischemia/reperfusion injury in rats through Nrf2/Sestrin2/PGC-1α/TFAM Pathway
BMC Pharmacology and Toxicology (2023)