Abstract
Background:
International guidelines suggest that growth of preterm infants should match intrauterine rates. However, the trajectory for extrauterine growth may deviate from the birth percentile due to an irreversible, physiological loss of extracellular fluid during postnatal adaptation to extrauterine conditions. To which “new” physiological growth trajectory preterm infants should adjust to after completed postnatal adaptation is unknown. This study analyzes the postnatal growth trajectories of healthy preterm infants using prospective criteria defining minimal support, as a model for physiological adaptation.
Methods:
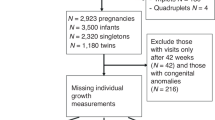
International, multi-center, longitudinal, observational study at five neonatal intensive care units (NICUs). Daily weights until day of life (DoL) 21 of infants with undisturbed postnatal adaptation were analyzed (gestational ages: (i) 25–29 wk, (ii) 30–34 wk).
Results:
981 out of 3,703 admitted infants included. Maximum weight loss was 11% (i) and 7% (ii) by DoL 5, birth weight regained by DoL 15 (i) and 13 (ii). Infants transitioned to growth trajectories parallel to Fenton chart percentiles, 0.8 z-scores below their birth percentiles. The new trajectory after completed postnatal adaptation could be predicted for DoL 21 with R2 = 0.96.
Conclusion:
This study provides a robust estimate for physiological growth trajectories of infants after undisturbed postnatal adaptation. In the future, the concept of a target postnatal trajectory during NICU care may be useful.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rochow N, Landau-Crangle E, Fusch C. Challenges in breast milk fortification for preterm infants. Curr Opin Clin Nutr Metab Care 2015;18:276–84.
Agostoni C, Buonocore G, Carnielli VP, et al.; ESPGHAN Committee on Nutrition. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr 2010;50:85–91.
Nutrition Committee Canadian Paediatric Society. Nutrient needs and feeding of premature infants. CMAJ 1995;152:1765–85.
American Academy of Pediatrics Committee on Nutrition. Nutritional Needs of Peterm Infants. In: Kleinman R, Greer F, eds. Pediatric Nutrition. 7th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2013:83–122.
Barker DJ. The developmental origins of adult disease. J Am Coll Nutr 2004;23(6 Suppl):588S–95S.
Rochow N, Fusch G, Mühlinghaus A, et al. A nutritional program to improve outcome of very low birth weight infants. Clin Nutr 2012;31:124–31.
Cole TJ, Statnikov Y, Santhakumaran S, Pan H, Modi N ; Neonatal Data Analysis Unit and the Preterm Growth Investigator Group. Birth weight and longitudinal growth in infants born below 32 weeks’ gestation: a UK population study. Arch Dis Child Fetal Neonatal Ed 2014;99:F34–40.
Ehrenkranz RA. Nutrition, growth and clinical outcomes. World Rev Nutr Diet 2014;110:11–26.
Horemuzova E, Söder O, Hagenäs L. Growth charts for monitoring postnatal growth at NICU of extreme preterm-born infants. Acta Paediatr 2012;101:292–9.
Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R. Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant. BMC Pediatr 2013;13:92.
Pereira-da-Silva L, Virella D. Is intrauterine growth appropriate to monitor postnatal growth of preterm neonates? BMC Pediatr 2014;14:14.
Tang W, Ridout D, Modi N. Influence of respiratory distress syndrome on body composition after preterm birth. Arch Dis Child Fetal Neonatal Ed 1997;77:F28–31.
Bauer K, Versmold H. Postnatal weight loss in preterm neonates less than 1,500 g is due to isotonic dehydration of the extracellular volume. Acta Paediatr Scand Suppl 1989;360:37–42.
Singhi S, Sood V, Bhakoo ON, Ganguly NK, Kaur A. Composition of postnatal weight loss & subsequent weight gain in preterm infants. Indian J Med Res 1995;101:157–62.
Kusuma S, Agrawal SK, Kumar P, Narang A, Prasad R. Hydration status of exclusively and partially breastfed near-term newborns in the first week of life. J Hum Lact 2009;25:280–6.
Fusch C, Jochum F. Water, sodium, potassium and chloride. World Rev Nutr Diet 2014;110:99–120.
Senterre T, Rigo J. Reduction in postnatal cumulative nutritional deficit and improvement of growth in extremely preterm infants. Acta Paediatr 2012;101:e64–70.
Stephens BE, Walden RV, Gargus RA, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics 2009;123:1337–43.
Tan MJ, Cooke RW. Improving head growth in very preterm infants–a randomised controlled trial I: neonatal outcomes. Arch Dis Child Fetal Neonatal Ed 2008;93:F337–41.
Blackwell MT, Eichenwald EC, McAlmon K, et al. Interneonatal intensive care unit variation in growth rates and feeding practices in healthy moderately premature infants. J Perinatol 2005;25:478–85.
Bauer K, Bovermann G, Roithmaier A, Götz M, Pröiss A, Versmold HT. Body composition, nutrition, and fluid balance during the first two weeks of life in preterm neonates weighing less than 1500 grams. J Pediatr 1991;118(4 Pt 1):615–20.
Ramel SE, Gray HL, Davern BA, Demerath EW. Body composition at birth in preterm infants between 30 and 36 weeks gestation. Pediatr Obes 2015;10:45–51.
Ehrenkranz RA, Younes N, Lemons JA, et al. Longitudinal growth of hospitalized very low birth weight infants. Pediatrics 1999;104(2 Pt 1):280–9.
Horbar JD, Ehrenkranz RA, Badger GJ, et al. Weight Growth Velocity and Postnatal Growth Failure in Infants 501 to 1500 Grams: 2000-2013. Pediatrics 2015;136:e84–92.
Hofer N, Kothari R, Morris N, Müller W, Resch B. The fetal inflammatory response syndrome is a risk factor for morbidity in preterm neonates. Am J Obstet Gynecol 2013;209:542.e1–542.e11.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 2013;13:59.
de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull 2004;25(1 Suppl):S15–26.
Crossland DS, Richmond S, Hudson M, Smith K, Abu-Harb M. Weight change in the term baby in the first 2 weeks of life. Acta Paediatr 2008;97:425–9.
Cleveland WS, Devlin SJ. Locally weighted regression - an approach to regression analysis by local fitting. J Am Stat Assoc 1988;83:596–610.
Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken: Wiley; 2011.
Efron B, Tibshirani RJ. An Introduction to the Bootstrap (Monographs on Statistics and Applied Probability). New York: Chapman and Hall; 1993.
Chin J, Rochow N, Fusch G, Murthy P, Radke D, Pogorzelski D, et al. Preliminary Report: Body Composition of Preterm Infants Using Air Displacement Plethysmography During the First Weeks of Life. Annual Meeting of Pediatric Academic Societies; Washington, USA; 2013. p. E-PAS2013:3828.460.
Schmelzle HR, Quang DN, Fusch G, Fusch C. Birth weight categorization according to gestational age does not reflect percentage body fat in term and preterm newborns. Eur J Pediatr 2007;166:161–7.
Rochow N, Raja P, Straube S, Voigt M. Misclassification of newborns due to systematic error in plotting birth weight percentile values. Pediatrics 2012;130:e347–51.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rochow, N., Raja, P., Liu, K. et al. Physiological adjustment to postnatal growth trajectories in healthy preterm infants. Pediatr Res 79, 870–879 (2016). https://doi.org/10.1038/pr.2016.15
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2016.15
This article is cited by
-
Nutritional intake and growth until two years of age in moderate and late preterms
Pediatric Research (2024)
-
Contemporary definitions of infant growth failure and neurodevelopmental and behavioral outcomes in extremely premature infants at two years of age
Journal of Perinatology (2024)
-
Growth after implementing a donor breast milk program in neonates <33 weeks gestational age or birthweight <1500 grams: Retrospective cohort study
Journal of Perinatology (2023)
-
Postnatal growth and body composition in extremely low birth weight infants fed with individually adjusted fortified human milk: a cohort study
European Journal of Pediatrics (2023)
-
Postnatal growth of preterm infants 24 to 26 weeks of gestation and cognitive outcomes at 2 years of age
Pediatric Research (2021)