Abstract
Background
The growth trajectories of common measurements, including estimated fetal weight (EFW), head circumference (HC), and abdominal circumference (AC), in fetuses with congenital heart disease (CHD) have not been described for different cardiac lesions. We hypothesized that (i) fetuses with CHD have differential growth in utero, and (ii) different categories of CHD demonstrate different in utero growth curves.
Methods
We performed a retrospective observational cohort study of pregnancies with known fetal CHD seen from January 2000 to June 2013. For analysis, the infants were divided into single ventricle (SV), biventricular conotruncal, d-transposition of great arteries (d-TGA), biventricular septal defects (SD; including atrial, ventricular, and atrioventricular SD), and all others (Other).
Results
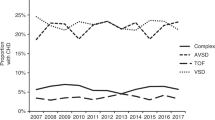
A total of 194 newborns met inclusion criteria. There was significant differential growth of EFW in all CHD types, except d-TGA, starting with low z-scores before 25 weeks gestation, improving toward normal around 30–32 weeks gestation, and then again differential growth with advancing gestation. SV and SD groups had significant differential growth of HC starting early in gestation and linearly progressing negative z-scores with advancing gestation.
Conclusion
We observed differences in the fetal growth curves throughout gestation for the major categories of CHD, including significant differential growth in even “simple” CHD, such as SD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rosenthal GL, Wilson PD, Permutt T, Boughman JA, Ferencz C . Birth weight and cardiovascular malformations: a population-based study. The Baltimore-Washington Infant Study. Am J Epidemiol 1991;133:1273–81.
Rosenthal GL . Patterns of prenatal growth among infants with cardiovascular malformations: possible fetal hemodynamic effects. Am J Epidemiol 1996;143:505–13.
Cnota JF, Hangge PT, Wang Y et al. Somatic growth trajectory in the fetus with hypoplastic left heart syndrome. Pediatr Res 2013;74:284–9.
Hahn E, Szwast A, Cnota J et al. The association of fetal growth, cerebral blood flow, and neurodevelopmental outcome in single ventricle fetuses. Ultrasound Obstet Gynecol 2015;47:460–5.
Ades AM, Dominguez TE, Nicolson SC et al. Morbidity and mortality after surgery for congenital cardiac disease in the infant born with low weight. Cardiol Young 2010;20:8–17.
Nikkilä A, Källén B, Marsál K . Fetal growth and congenital malformations. Ultrasound Obstet Gynecol 2007;29:289–95.
Källén K . Increased risk of perinatal/neonatal death in infants who were smaller than expected at ultrasound fetometry in early pregnancy. Ultrasound Obstet Gynecol 2004;24:30–4.
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK . Estimation of fetal weight with the use of head, body, and femur measurements—a prospective study. Am J Obstet Gynecol 1985;151:333–7.
Committee on Obstetric Practice, the American Institute of Ultrasound in Medicine, and the Society for Maternal-Fetal Medicine. Committee Opinion No 700: methods for estimating the due date. Obstet Gynecol 2017;129:e150–4.
Miller A, Riehle-Colarusso T, Alverson CJ, Frías JL, Correa A . Congenital heart defects and major structural noncardiac anomalies, Atlanta, Georgia, 1968 to 2005. J Pediatr 2011;159 (1): 70–78.e2.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS . New intrauterine growth curves based on United States data. Pediatrics 2010;125:e214–24.
International Fetal and Newborn Growth Consortium for the 21st century Article: International Fetal Growth Standards - latest charts available - INTERGROWTH-21st https://intergrowth21.tghn.org/articles/international-fetal-growth-standards-latest-charts-available/ Published 2015. Accessed 22 January 2016.
Hickey EJ, Nosikova Y, Zhang H et al. Very low-birth-weight infants with congenital cardiac lesions: is there merit in delaying intervention to permit growth and maturation? J Thorac Cardiovasc Surg 2012;143:126–36.
Tabbutt S, Gaynor JW, Newburger JW . Neurodevelopmental outcomes after congenital heart surgery and strategies for improvement. Curr Opin Cardiol 2012;27:82–91.
von Rhein M, Buchmann A, Hagmann C et al. Severe congenital heart defects are associated with global reduction of neonatal brain volumes. J Pediatr 2015;167 (6): 1259–63.e1.
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A . Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr 2008;153:807–13.
Williams IA, Fifer WP, Andrews H . Fetal growth and neurodevelopmental outcome in congenital heart disease. Pediatr Cardiol 2015;36:1135–44.
Lin S, Leonard D, Co MAM et al. Pre-eclampsia has an adverse impact on maternal and fetal health. Transl Res 2015;165:449–63.
Brodwall K, Leirgul E, Greve G et al. Possible common aetiology behind maternal preeclampsia and congenital heart defects in the child: a Cardiovascular Diseases in Norway Project Study. Paediatr Perinat Epidemiol 2016;30:76–85.
Jones HN, Olbrych SK, Smith KL et al. Hypoplastic left heart syndrome is associated with structural and vascular placental abnormalities and leptin dysregulation. Placenta 2015;36:1078–86.
Sullivan PM, Dervan LA, Reiger S, Buddhe S, Schwartz SM . Risk of congenital heart defects in the offspring of smoking mothers: a population-based study. J Pediatr 2015;166:978–84.
Acknowledgements
We are grateful to the staff in the ultrasound and echocardiography laboratories at the involved institutes, as well as to the patients for whom we have the privilege to provide care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary material is linked to the online version of the paper
Supplementary information
Rights and permissions
About this article
Cite this article
Puri, K., Warshak, C., Habli, M. et al. Fetal somatic growth trajectory differs by type of congenital heart disease. Pediatr Res 83, 669–676 (2018). https://doi.org/10.1038/pr.2017.275
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.275
This article is cited by
-
Incidence, distribution, disease spectrum, and genetic deficits of congenital heart defects in China: implementation of prenatal ultrasound screening identified 18,171 affected fetuses from 2,452,249 pregnancies
Cell & Bioscience (2023)
-
Altered erythropoiesis in newborns with congenital heart disease
Pediatric Research (2022)
-
The Effect of Size and Asymmetry at Birth on Brain Injury and Neurodevelopmental Outcomes in Congenital Heart Disease
Pediatric Cardiology (2022)