Abstract
Comprehensive genomic profiling (CGP) expands treatment options for solid tumor patients and identifies hereditary cancers. However, in Japan, confirmatory tests have been conducted in only 31.6% of patients with presumed germline pathogenic variants (GPVs) detected through tumor-only testing. Paired tumor-normal analysis enables differentiation between somatic and germline variants. GenMineTOP, covered by Japan’s national health insurance since August 2023, analyzes paired samples and reports GPVs in 40 genes. This study provides an initial characterization of GPVs based on clinical findings collected during the first year of GenMineTOP implementation. We analyzed 1356 solid tumor patients who underwent GenMineTOP testing in the Center for Cancer Genomics and Advanced Therapeutics (C-CAT) database between August 2023 and July 2024, focusing on GPV detection rates, gene distribution, and comparisons with other CGP tests. Among the analyzed cancer types, GenMineTOP had a higher proportion of CNS/brain, soft tissue, bone, and head and neck cancers compared to other CGP tests. GPVs were detected in 73 patients (5.4%), with 38.2% classified as off-tumor. HR-related GPVs (ATM, BRCA1, BRCA2, BRIP1, PALB2, RAD51C, RAD51D) were found in both males (median age: 69) and females (median age: 54). Among males, 57.9% were aged 65 or older. GPVs may be detected in any cancer patients, including those with off-tumor findings, particularly in older male patients, especially in HR-related genes. These findings support the use of paired CGP to improve the diagnosis of hereditary cancers that could otherwise remain undetected.
Similar content being viewed by others
Introduction
Comprehensive genomic profiling (CGP) creates individual genomic profiles of tumors or tumor/normal tissues to explore therapeutic options. The primary objective of CGP testing is to guide patient treatment; however, it also has the potential to reveal the presence of germline pathogenic variants (GPVs). Here, GPVs are defined as germline-derived pathogenic variants in genes associated with autosomal dominant hereditary cancers. In Japan, based on the ACMG SF v3.2 [1], the Kosugi Group List designates 53 genes for the disclosure of secondary findings (Supplementary Table 1). This list includes genes deemed clinically actionable when GPVs are detected through CGP testing or other comprehensive genetic analyses.
In tumor-only panels, it is not possible to determine whether pathogenic variants, suspected to be of germline origin based on medical history, the Variant Allele Frequency (VAF) values and gene-specific germline conversion rates, are truly germline-derived. To confirm whether a presumed GPV is a true GPV, germline confirmatory testing (hereafter referred to as ‘confirmatory tests’) is necessary. In contrast, tumor/normal paired panels can detect GPVs without the need for confirmatory tests.
Reports from international studies indicate that the detection rate of GPVs through CGP ranges from 4.3% to 17.5% [2,3,4,5,6,7,8]. Identifying hereditary cancers not only benefits the affected individual but also facilitates health management for their relatives [3, 7, 9].
As of November 2024, five types of CGP have been clinically applicable in Japan. All genomic profiling data and clinical information are transferred to the Center for Cancer Genomics and Advanced Therapeutics (C-CAT) under written informed consent (consent rate: 99.7%), where the data is available for research purposes [10]. Notably, CGP testing under Japan’s public health insurance system is only applicable to patients who have completed or are expected to complete standard treatment. Consequently, this dataset consists predominantly of patients with poor-prognosis cancers. The five types of CGP tests include a tumor-only panel (FoundationOne® CDx), two liquid biopsy panels (FoundationOne Liquid® CDx and Guardant360® CDx), and two tumor/normal paired panels (OncoGuide™ NCC Oncopanel System (NOP) [10, 11] and GenMineTOP). Among CGP tests in Japan, the most frequently used tumor-only panel is FoundationOne® CDx (75%), while the liquid biopsy panels account for 11%. Tumor/normal paired panel usage remains limited to 14.3% in Japan [12, 13]. In tumor-only panels, patients undergoing CGP testing have completed standard treatment, and the rate of confirmatory tests for presumed GPVs is only 23.3–31.6% [14, 15]. In Japan, 9.6% of patients tested with CGP exhibited presumed GPVs, but only 49 patients (23.3%) underwent confirmatory tests, and among them, 15 patients (30.6%) were confirmed as GPVs. This suggests that hereditary cancers were diagnosed in only 0.6% of all patients who underwent FoundationOne® CDx testing [14]. Therefore, hereditary cancers based on tumor-only panels are likely underdiagnosed.
GenMineTOP is the first CGP test in Japan that incorporates both DNA and RNA panels, covering 737 and 455 genes, respectively. Notably, the RNA panel is particularly advantageous for detecting a wide range of gene fusions, which can support both therapeutic decision-making and accurate diagnosis [16]. Until the approval of GenMineTOP in August 2023, NOP was the only tumor/normal paired panel available in Japan. Initially, NOP analyzed 114 genes, of which 16 were designated for GPV disclosure [17]. In February 2021, the number of target genes increased to 124, and all detected GPVs were subsequently disclosed. However, 20 genes the Kosugi Group List recommended were still not included [13]. In contrast, GenMineTOP analyzes 737 DNA panel genes, including all genes from the Kosugi Group List [18], with 40 highly recommended genes designated for reporting (Supplementary Fig. 1A). As of October 2024, the number of germline disclosure genes in GenMineTOP has been revised to 59 (Supplementary Fig. 1B), although tumor-normal paired testing is not a substitute for dedicated germline testing, which follows different pipelines and methodologies for germline analysis.
To date, nationwide real-world analysis on CGP-detected GPVs has only evaluated NOP (e.g., Yamaguchi et al., 2021). Furthermore, investigation of homologous recombination (HR) related genes other than BRCA1/2 and the impact of differences in target genes between panels on GPV detection has been limited. The objective of this study was to clarify the current challenges in germline analysis as well as the clinical utility of GenMineTOP through its detection of GPVs.
Materials and methods
Patient samples of GenMineTOP from the C-CAT database
The data were obtained from the C-CAT database, curated by the National Cancer Center of Japan, which houses the CGP test results [10]. We accessed the C-CAT database to collect data on GenMineTOP cases registered between August 2023 and June 2024, downloading their clinical and genomic data on July 4, 2024. Additionally, we collected data on 21,169 CGP cases other than GenMineTOP, registered between July 2023 and June 2024, and downloaded their data on November 21, 2024. This study was approved by the Research Ethics Committee of the Faculty of Medicine at the University of Tokyo (approval number: 2021341G, G10114-(21)) and the C-CAT Data Utilization Review Board (approval number: CDU2022-026N).
GenMineTOP testing
GenMineTOP, which analyzes 737 genes in its DNA panel and 455 genes in its RNA panel, has been covered by health insurance since August 2023 in Japan. It enables the detection of fusion genes in 455 genes and exon skipping in 5 genes with high sensitivity. In this study, GPVs were assessed for 40 hereditary cancer-related genes, although currently, GPVs for 59 genes are covered (Supplementary Fig. 1A, B). In GenMineTOP, germline single nucleotide variants (SNVs) and insertions/deletions (indels) in 40 genes are reported if classified as pathogenic or likely pathogenic in the ClinVar or Ambry Genetics Corporation databases. Additionally, for tumor suppressor genes, null variants (including nonsense mutations, splice site mutations, frameshift mutations, and start codon extensions) are also reported. All reported germline variants were manually reviewed to ensure accuracy. Allele-specific chromosomal copy number diagrams determined from over 8000 SNP probes are included in the Supplementary Report. VAF of GPVs is reported for both normal and corresponding tumor samples.
However, tumor VAF values were not available in the C-CAT database used in this study and thus could not be incorporated into the analysis.
Germline pathogenic variants
Germline pathogenic variants (GPVs) were evaluated based on the 2015 guidelines of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG/AMP). Variants classified as pathogenic or likely pathogenic were defined as GPVs in this study. Variants associated with autosomal recessive inheritance were considered GPVs only when present in a homozygous or compound heterozygous state; heterozygous carriers of such variants were excluded. For tumor suppressor genes, null variants were also reported in the dataset. The system may capture variants with uncertain significance, such as C-terminal null variants (e.g., BRCA2 p.R3384*); however, these variants were excluded from the definition of GPVs. For POLE variants, classification was based on recent recommendations specific to germline variants in the exonuclease domain (ED), emphasizing that pathogenic variants are typically non-disruptive missense mutations within the ED. In contrast, loss-of-function variants—such as nonsense or frameshift mutations—are generally not considered to be associated with cancer predisposition [19].
Classification of tumors based on genetic alterations
Cancer susceptibility genes are linked to specific tumor types, termed “on-tumor”. In this study, the classification of on-tumor genes (Supplementary Table 2) was based on multiple sources, including the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®), such as Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate (Version 3, 2025) and Colorectal, Endometrial, and Gastric (Version 4, 2024), among others [20,21,22,23,24]. For example, a pathogenic BRCA1 variant is considered “on-tumor” in breast, pancreatic, ovarian, or prostate cancer because it increases the risk of these cancers. In contrast, the same variant is considered “off-tumor” in colorectal or liver cancer, as no clear risk association has been established.
Definition of homologous recombination-related genes
BRCA1 and BRCA2 are well-established as key genes of the homologous recombination (HR) repair pathway. Recent studies have demonstrated that other HR-related genes, such as RAD51C/D, PALB2, ATM, CHEK2, FANCA, and FANCD2, also contribute to cancer susceptibility. Aberrations in these genes lead to impaired DNA damage repair, resulting in genomic instability and promoting cancer initiation and progression [25]. In this study, 15 genes (BRCA1, BRCA2, ATM, BRIP1, BARD1, CDK12, CHEK1, CHEK2, FANCL, PALB2, PPP2R2A, RAD51B, RAD51C, RAD51D, RAD54L) approved by the FDA for olaparib were defined as HR-related genes [26].
Statistical analysis
Fisher’s exact test was used to compare patient backgrounds between GenMineTOP and other CGP tests, sex-based differences in GPV frequency, age group comparisons, and on-tumor/off-tumor detection rates among gene categories. The Wilcoxon rank-sum test was used to compare continuous variables such as median age. When multiple pairwise comparisons were performed, the Bonferroni correction was applied. A two-tailed P-value < 0.05 was considered statistically significant unless otherwise specified. All statistical analyses were conducted using JMP software (version 18.0.2, SAS Institute Inc., Cary, NC, USA).
Results
Comparison of patient backgrounds in GenMineTOP vs. other panels
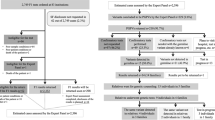
This study included 1356 GenMineTOP cases from the C-CAT database. The median age was 61 (range: 0–90), with equal gender distribution (Supplementary Table 3). We compared 1356 GenMineTOP cases with 21,169 CGP cases excluding GenMineTOP cases (categorized as the “other” group) from the same period. In terms of cancer types analyzed, Fisher’s exact test identified significant differences in the proportions of specific cancer types
between the GenMineTOP and the other group (p < 0.05). GenMineTOP had a higher proportion of patients with CNS/brain (11% vs. 2%), soft tissue (12% vs. 3%), bone (3% vs. 0.4%), and head and neck (6% vs. 3%) cancers compared to the other group. Conversely, the proportions were lower for pancreatic (8% vs. 19%), and biliary tract (5% vs. 10%), lung (4% vs. 7%), esophagus/stomach (5% vs. 6%) cancers (Fig. 1A). When analyzed separately by gender, statistically significant differences were observed in males for CNS/brain (13% vs. 2%), soft tissue (11% vs. 3%), bone (5% vs. 0.4%), and head and neck (8% vs. 4%) cancers, where GenMineTOP had a higher proportion (p < 0.05, Fisher’s exact test). Conversely, significant differences were found in pancreatic (10% vs. 20%), prostate (2% vs. 12%), biliary tract (6% vs. 12%), esophagus/stomach (6% vs. 9%), and lung (6% vs. 8%) cancers, where the proportions were lower in GenMineTOP. In females, significant differences were observed for soft tissue (12% vs. 2%) and CNS/brain (10% vs. 2%), uterus (9% vs. 6%), head and neck (4% vs. 2%) cancers where GenMineTOP had a higher proportion (p < 0.05, Fisher’s exact test). However, GenMineTOP had significantly lower proportions in pancreas (7% vs. 17%), breast (8% vs. 13%), biliary tract (4% vs. 8%) cancers (Fig. 1B). Regarding age distribution, GenMineTOP had a significantly higher proportion of the pediatric, adolescent and young adult cancers (0–39 years old), compared to the other group (14.4% vs. 4.3%, p < 0.05, Fisher’s exact test) (Fig. 1C).
Comparison of patient backgrounds between GenMineTOP and other CGP cases. A Proportion of cancer types among all patients analyzed using GenMineTOP (n = 1356) and other CGP cases (n = 21,169). B Proportion of cancer types stratified by sex in GenMineTOP and other CGP cases. C Age distribution of all patients analyzed using GenMineTOP (n = 1356) and other CGP cases (n = 21,169)
Characteristics of patients with detected GPVs
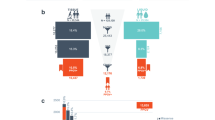
As a result, 76 GPVs were detected in 73 out of 1356 patients (5.4%) (Supplementary Table 4). Among them, 34 patients (46.6%) were male, and 39 patients (53.4%) were female. The age distribution differed by gender. In males, GPVs were the most detected in their 70s (26.5%), whereas females were predominantly in their 40 s (30.7%). GPVs in individuals under 20 years old were exclusively detected in males at 14.7% (Fig. 2A). All 76 GPVs had a disclosure recommendation level of A or higher according to the Kosugi Group List. Among these, 19.7% (15 GPVs) were outside the scope of analysis by the NOP. The breakdown of these 15 GPVs was as follows: RAD51D (n = 8), BRIP1 (n = 2), SDHB (n = 2), SDHA (n = 2), CDH1 (n = 1) (Supplementary Table 5).
Cancers in which at least four GPVs were detected and the GPV detection rate was 3% or higher included ovary/fallopian tube (11.9%, 10/84), pancreas (7.1%, 8/113), soft tissue (5.1%, 8/157), biliary tract (8.3%, 6/72), CNS/brain (4.0%, 6/151), peripheral nervous system (20%, 4/20), and breast (7.7%, 4/52). The detection frequency of GPVs is shown for each cancer type, stratified by sex (Fig. 2B). Among females, the highest detection frequency was observed in ovary/fallopian tube (11.9%, 10/84), followed by biliary tract (10.3%, 3/29), and head and neck (8.3%, 2/24). Among males, the most frequent cancer type with GPVs was pancreas (9.1%, 6/66), followed by biliary tract (7.0%, 3/43), and bone (6.5%, 2/31). These results indicate that the distribution of GPVs varies depending on cancer type and sex (Fig. 2B).
Regarding genes, BRCA2 was the most frequently detected gene in both males and females. Although BRCA1 was more frequently observed in females, there was no statistically significant difference in the distribution of detected genes between sexes (Fig. 2C).
Details of the detected GPVs (Age)
Patients were categorized by age (0–39, 40–64, ≥65 years). Statistical comparison was conducted between those aged ≥65 and <65. No overall sex-based difference was noted; however, in the BRCA1/2 genes, males were significantly more likely to be aged ≥65 years (p < 0.01, Fisher’s exact test) (Fig. 3).
Age distribution by gene category and sex (stacked bar plot). Patients are grouped by gene category and stratified by sex (male, female). Bars represent the number of patients in three age groups: ≥65 years (green), 40–64 years (orange), and 0–39 years (purple). A significant difference in the proportion of elderly patients (≥65 years) between males and females in the BRCA1/2 group was observed (p < 0.001, Fisher’s exact test). The specific genes included in each category for males and females are listed on the right
Among the eight patients (with nine variants) aged 0–39 years, TP53 was the most frequently detected gene, identified in 2 out of 8 patients (25.0%). Other gene alterations included APC, BRCA2, NF1, NF2, SDHB, and ATM/RAD51C, each detected in one patient (12.5%, respectively). Due to the small sample size, statistical comparisons were not performed (Supplementary Fig. 2).
Details of the detected GPVs (Cancer type: On-tumor/Off-tumor)
The detected cancer types and genes are detailed in Fig. 4A. In the peripheral nervous system patients, the breakdown was NF1 (n = 3) and NF2 (n = 1). In the six cases of biliary tract cancer where GPVs were detected, variants in six different genes were identified. In the genes where GPVs were detected in at least three cases (eight genes: BRCA1, BRCA2, RAD51D, NF1, TP53, ATM, MLH1, MSH2), GPVs were identified in at least three different cancer types.
Details of detected GPVs by cancer type (On-tumor/Off-tumor). A A table with GPVs as row headers and cancer types as column headers, categorized into two groups: On-tumor (blue) and Off-tumor (brown). HR-related genes are highlighted in yellow. B On-tumor/Off-tumor distribution by gene category (stacked bar plot). Patients are categorized by gene group, showing the number of cases classified as on-tumor (blue) and off-tumor (brown)
The detection rate of GPV for each cancer type was calculated. On-tumor findings accounted for 61.8% (47/76), while off-tumor findings comprised 38.2% (29/76). Among BRCA1/2, 60.7% (17/28) were classified as on-tumor. BRCA1 was predominantly detected in ovarian cancer, with 77.8% (7/9) of patients classified as on-tumor. In contrast, BRCA2 was detected across various cancer types with 52.6% (10/19) classified as on-tumor. The on-tumor detection rate was 77.8% (7/9) for NF1/NF2, 100% (6/6) for TP53, and 100% (7/7) for MMR genes, indicating that most of these variants were identified in clinically associated cancer types. In Fig. 4B, the on-tumor detection rate for the HRD-related gene group was significantly lower than that for both the TP53 group (p = 0.003) and the MMR group (p = 0.001), based on Fisher’s exact test with Bonferroni correction.
High tumor mutational burden (TMB-high; TMB-H) was observed in 8.2% (6/73) of cases. Five of these involved GPVs in mismatch repair (MMR) genes and showed TMB values ≥25 mut/Mb. The remaining case (TMB: 10.7 mut/Mb) did not involve MMR-GPVs. Overall, 71.4% (5/7) of patients with MMR-GPVs had TMB-H, suggesting a potential link to tumorigenesis. The other two MMR-GPV cases had low TMBs (2.7 and 4.8 mut/Mb), indicating limited functional impact (Supplementary Table 4).
Gender and age of patients with GPVs in HR-related genes
GPVs were detected in seven HR-related genes: BRCA2, BRCA1, RAD51D, ATM, BRIP1, PALB2, and RAD51C. Among patients classified as on-tumor, only 14.3% (1/7) of males were aged ≤64 years, compared to 92.3% (12/13) of females (p < 0.001, Fisher’s exact test) (Fig. 5A). In contrast, among off-tumor patients, the proportion of those aged ≤64 years was similar between males (58.3%, 7/12) and females (54.5%, 6/11) (Fig. 5A). In the overall HRD-related group, the most common age group for males was the 70s (42.1%), while for females, it was the 40s–50s (58.4%). The median age was significantly higher in males (69.0 years, IQR: 56.0–75.0 years) than in females (54.5 years, IQR: 47.3–64.5 years) (Wilcoxon rank-sum test, p = 0.016) (Fig. 5B).
Gender and age distribution of patients with GPVs in HR-related genes. A Number of patients with GPVs in HR-related genes (7 genes), classified as on-tumor (blue) or off-tumor (brown). The number of patients for each detected HR-related gene is also presented. B Age distribution of patients with GPVs in HR-related gene, stratified by sex
Distribution of variant allele frequencies
The average VAF in blood samples analyzed by GenMineTOP was 0.47. Among the six TP53 variants detected as GPV, two variants exhibited low VAF values. The patients with low VAF values included a 75-year-old female diagnosed with soft tissue sarcoma (TP53 p.K132R, VAF = 0.224 [124/553]) and a 62-year-old male diagnosed with pancreatic cancer (TP53 p.H179Y, VAF = 0.255 [116/455]). The cause of the low VAF in these patients cannot be clarified within this study and may possibly reflect clonal hematopoiesis of indeterminate potential (CHIP). Further germline-specific testing is required for a more comprehensive evaluation (Fig. 6).
Detection and clinical implications of GPVs
Among the 73 patients in whom GPVs were detected, five were from our institution. Genetic counseling was conducted for four of these patients (Supplementary Table 6), including one patient whose GPV was already known prior to CGP testing. For the one patient who did not receive genetic counseling, the reason was a deterioration of the patient’s general condition, which prevented the disclosure of the CGP test results. In one patient (Patient 4) with a BRCA2 GPV, a family history of breast cancer facilitated discussions regarding diagnostic evaluation for the patient’s relatives.
As allele-specific copy number graphs are available in “Supplementary Information” (Supplementary Fig. 3A), we assessed the presence of loss of heterozygosity (LOH) by integrating allele-specific copy number graphs (Supplementary Fig. 3B–E), and variant allele frequencies (VAFs) in tumor and normal samples. LOH was inferred when the copy number of the minor allele (shown in blue) was markedly decreased, indicating allelic imbalance.
Considering the histologically estimated tumor content ratio, we presumed that LOH at the locus of the GPV gene was coexistent with GPV in Patients 1, 2 and 5. In Patient 3, a somatic pathogenic variant coexisted with GPV in the NF1 gene. However, in Patient 4 with a BRCA2 GPV, neither LOH nor a somatic pathogenic variant was identified, suggesting that the BRCA2 GPV may be unrelated to the liver cancer and instead represents an incidental finding.
Discussion
This study demonstrated the utility of GenMineTOP in detecting GPVs across diverse cancer types and age groups. In this study, we addressed the expansion of target genes and the significance of the tumor-normal paired panel through analyses based on age, sex, and on/off tumor classification.
In the first year of insurance coverage, GenMineTOP was found to include a high proportion of CNS/brain, soft tissue, bone, and head and neck cancers. As previously noted, one of the distinguishing features of GenMineTOP is its ability to detect gene fusions through RNA-based analysis. This technical advantage may have contributed to its preferential selection for sarcomas and certain other tumor types in our cohort, as shown in Fig. 1A. Compared to CGP tests that analyze only DNA, the inclusion of RNA profiling may provide additional clinical value for tumors in which fusion genes are more prevalent [16]. Previous studies have reported a wide range of GPV detection rates through CGP testing, from 4.3% to 17.5% [2,3,4,5,6,7,8]. Such variation can be attributed to multiple factors, including the number of genes analyzed, variant classification criteria, patient demographics (e.g., cancer types), and ethnic background. Notably, a recent international study using tumor/normal paired CGP testing across multiple cancer types reported an overall GPV detection rate of 7.3%, with higher rates in ovarian (13.8%) and breast cancers (10.8%), and lower rates in bladder (6.6%) and lung cancers (5.8%) [27]. These differences underscore the importance of tumor type when interpreting GPV detection rates. In our analysis, differences in cancer type distribution between GenMineTOP and other CGP tests likely contributed to the variation in GPV detection, and should be considered when making cross-cohort comparisons.
Analysis by cancer type revealed that, in addition to ovarian, breast, and pancreatic cancers, which are widely known for their high frequency of hereditary cancers, GPVs were detected at a rate of 3% or higher, including in soft tissue, CNS/brain, biliary tract, and peripheral nervous system cancers. This indicates the need to be aware of GPVs across a diverse range of cancer types.
The GPV detection rate was 5.4%, while the detection rate in NOP was 4.1–4.5% (n = 3739–6313) [12, 13]. Notably, six genes with 15 unique variants were exclusively detected by GenMineTOP but not in NOP, with RAD51D accounting for eight of these variants. Genes in the RAD51 protein family play a crucial role in homologous recombination and DNA repair. RAD51D has been associated with an increased risk of ovarian cancer, with an estimated germline prevalence of approximately 1% in ovarian cancer patients [28,29,30,31,32]. Additionally, its association with breast cancer risk has been reported [33,34,35,36]. BRIP1, detected in two patients, has also been linked to an increased ovarian cancer risk [37,38,39]. Other detected genes included SDHB, CDH1, and SDHA, highlighting the potential for comprehensive germline testing to identify individuals who could otherwise remain undiagnosed. At the time of this analysis, GenMineTOP included 40 genes for germline variant reporting. However, as of October 2024, the gene panel has expanded to 59 genes, incorporating all genes recommended in the Kosugi Group List (Supplementary Fig. 1B). Further validation of newly added genes is warranted.
This study confirmed that GPVs, particularly in HR-related genes such as BRCA2 and RAD51D, were also detected in older patients. This likely reflects the age distribution of cancers associated with HR-related genes. For instance, prostate cancer primarily affects older men, and pancreatic cancer is more common in older individuals, which may explain the higher detection rate of GPVs in these groups [40, 41]. GPV age distribution also varied by sex, with 92.3% of HR-related genes detected in younger women (<65 years), reflecting the early-onset nature of breast and ovarian cancer [42, 43].These findings underscore the importance of CGP testing across all age groups.
Of note, 38.2% of GPVs in this study were detected in off-tumor patients. While the role of these GPVs in tumorigenesis remains unclear, their detection suggests the potential for underlying hereditary cancers. The detection of BRCA1/2 variants in off-tumor patients, for example, may inform cancer surveillance strategies for other related cancers and contribute to family health management. Particularly, 75.0% of non-BRCA1/2 HR-related genes were detected in off-tumor patients, suggesting their possible but currently unestablished contribution to tumorigenesis. Momozawa et al., have reported that BRCA1/2 variants may increase the risk of gastric, esophageal, and biliary tract cancers [44]. Additional data collection is necessary to clarify the role of non-BRCA1/2 genes. However, GPV detection in off-tumor patients may also be incidental, necessitating consideration of the psychological and medical implications for patients and their families. These findings highlight the critical role of genetic counseling in managing unexpected results.
Two low VAF pathogenic TP53 variants were detected, suggesting CHIP, somatic mosaicism, or germline mosaicism. However, as this study did not analyze normal tissues other than blood, distinguishing these possibilities was not feasible. Notably, the detected variants (p.K132R, p.H179Y) were not among previously reported CHIP hotspots (p.R248W, p.R273H, p.Y220C) [45], emphasizing the complexity of interpreting low-frequency variants in CGP data. It is important to emphasize that tumor-normal paired CGP testing is not a substitute for dedicated germline testing, which employs distinct analytical pipelines and confirmatory procedures tailored to germline variant interpretation. In particular, genes such as TP53 are prone to somatic alterations in blood cells (e.g., CHIP), and low VAF variants in such genes require careful evaluation through additional confirmatory testing. These limitations should be carefully considered when interpreting germline variant findings from tumor-normal CGP data. and the need for additional confirmatory tests.
GenMineTOP allows estimation of LOH for each GPV through its allele-specific chromosomal copy number diagrams, in addition to VAF in both normal and tumor samples. This enables the estimation of whether the detected GPV is a driver of tumorigenesis or an incidental finding. However, in the present study, we used C-CAT-registered data, which did not include tumor VAF values or copy number figures. As a result, LOH could not be assessed in most cases, limiting our ability to evaluate the functional significance of each GPV. Notably, five cases included in the C-CAT data originated from our institution, where access to the full GenMineTOP reports allowed us to review copy number plots and VAF values. For these cases, LOH assessment was feasible and used to support interpretation of the GPVs.
GenMineTOP classifies variants based on established databases like ClinVar and Ambry Genetics Corporation databases, reporting pathogenic or likely pathogenic variants, including null variants in tumor suppressor genes. However, the system may capture variants with uncertain significance, such as C-terminal null variants, necessitating molecular tumor board review for refinement. Further standardization and functional studies could improve the accuracy of germline variant interpretation in precision oncology.
This study has several limitations. First, its retrospective design may introduce selection bias, as only patients undergoing CGP testing were included. Second, reliance on pre-existing databases (C-CAT) limits access to key clinical details such as family and treatment history, which may influence GPV interpretation. Additionally, genetic counseling and confirmatory test results were not always available for patients diagnosed outside our institution, making it unclear whether BRCA1/2 variants detected through CGP had been previously identified. Furthermore, GenMineTOP is not a germline-focused genetic test and does not employ a germline-specific analytical pipeline, such as the detection of large deletions by MLPA, which fundamentally differentiates it from conventional hereditary cancer testing. Because no confirmatory test data was available to validate the pathogenicity of the detected GPVs, we cannot draw definitive conclusions regarding the analytical or clinical utility of these findings. Lastly, the impact of the expanded 59-gene panel (as of October 2024) on GPV detection and clinical outcomes requires further evaluation.
GenMineTOP demonstrated its utility as a CGP test capable of detecting clinically actionable GPVs across a wide range of cancer types and age groups through tumor/normal paired analysis. By incorporating the Kosugi Group List, GenMineTOP covers a broader range of genes and can identify variants undetectable by other panels, underscoring its potential role in advancing precision oncology.
References
Miller DT, Lee K, Abul-Husn NS, Amendola LM, Brothers K, Chung WK, et al. ACMG SF v3.2 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2023;25:100866. https://doi.org/10.1016/j.gim.2023.100866.
Clark DF, Maxwell KN, Powers J, Lieberman DB, Ebrahimzadeh J, Long JM, et al. Identification and confirmation of potentially actionable germline mutations in tumor-only genomic sequencing. JCO Precis Oncol. 2019;3:1–11. https://doi.org/10.1200/PO.19.00076.
DeLeonardis K, Hogan L, Cannistra SA, Rangachari D, Tung N. When should tumor genomic profiling prompt consideration of germline testing?. J Oncol Pr. 2019;15:465–73. https://doi.org/10.1200/JOP.19.00201.
Meric-Bernstam F, Brusco L, Daniels M, Wathoo C, Bailey AM, Strong L, et al. Incidental germline variants in 1000 advanced cancers on a prospective somatic genomic profiling protocol. Ann Oncol. 2016;27:795–800. https://doi.org/10.1093/annonc/mdw018.
Seifert BA, O'daniel JM, Amin K, Marchuk DS, Patel NM, Parker JS, et al. Germline analysis from tumor-germline sequencing dyads to identify clinically actionable secondary findings. Clin Cancer Res. 2016;22:4087–94. https://doi.org/10.1158/1078-0432.CCR-16-0015.
Kuzbari Z, Bandlamudi C, Loveday C, Garrett A, Mehine M, George A, et al. Germline-focused analysis of tumour-detected variants in 49,264 cancer patients: ESMO Precision Medicine Working Group recommendations. Ann Oncol. 2023;34:215–27. https://doi.org/10.1016/j.annonc.2022.12.003.
Schrader KA, Cheng DT, Joseph V, Prasad M, Walsh M, Zehir A, et al. Germline variants in targeted tumor sequencing using matched normal DNA. JAMA Oncol. 2016;2:104–11. https://doi.org/10.1001/jamaoncol.2015.5208.
Mandelker D, Zhang L, Kemel Y, Stadler ZK, Joseph V, Zehir A, et al. Mutation detection in patients with advanced cancer by universal sequencing of cancer-related genes in tumor and normal DNA vs guideline-based germline testing. JAMA. 2017;318:825–35. https://doi.org/10.1001/jama.2017.11137.
Garber JE, Offit K. Hereditary cancer predisposition syndromes. J Clin Oncol. 2005;23:276–92. https://doi.org/10.1200/JCO.2005.10.042.
Kohno T, Kato M, Kohsaka S, Sudo T, Tamai I, Shiraishi Y, et al. C-CAT: the national datacenter for cancer genomic medicine in Japan. Cancer Discov. 2022;12:2509–15. https://doi.org/10.1158/2159-8290.CD-22-0417.
Yoshii Y, Okazaki S, Takeda M. Current status of next-generation sequencing-based cancer genome profiling tests in Japan and prospects for liquid biopsy. Life. 2021;11:796 https://doi.org/10.3390/life11080796.
Yamaguchi T, Ikegami M, Aruga T, Kanemasa Y, Horiguchi SI, Kawai K, et al. Genomic landscape of comprehensive genomic profiling in patients with malignant solid tumors in Japan. Int J Clin Oncol. 2024;29:1417–31. https://doi.org/10.1007/s10147-024-02554-8.
Satake T, Kondo S, Tanabe N, Mizuno T, Katsuya Y, Sato J, et al. Pathogenic germline variants in BRCA1/2 and p53 identified by real-world comprehensive cancer genome profiling tests in Asian patients. Cancer Res Commun. 2023;3:2302–11. https://doi.org/10.1158/2767-9764.CRC-23-0018.
Minamoto A, Yamada T, Shimada S, Kinoshita I, Aoki Y, Oda K, et al. Current status and issues related to secondary findings in the first public insurance covered tumor genomic profiling in Japan: multi-site questionnaire survey. J Hum Genet. 2022;67:557–63. https://doi.org/10.1038/s10038-022-01028-x.
Shimada S, Yamada T, Minamoto A, Matsukawa M, Yabe I, Tada H, et al. Nationwide survey of the secondary findings in cancer genomic profiling: survey including liquid biopsy. J Hum Genet. 2025;70:33–40. https://doi.org/10.1038/s10038-024-01294-x.
Watanabe K, Ogawa M, Shinozaki-Ushiku A, Tsutsumi S, Tatsuno K, Aburatani H, et al. Real-world data analysis of genomic alterations detected by a dual DNA-RNA comprehensive genomic profiling test. Cancer Sci. 2025;116:1984–95. https://doi.org/10.1111/cas.70071.
Sunami K, Ichikawa H, Kubo T, Kato M, Fujiwara Y, Shimomura A, et al. Feasibility and utility of a panel testing for 114 cancer-associated genes in a clinical setting: a hospital-based study. Cancer Sci. 2019;110:1480–90. https://doi.org/10.1111/cas.13969.
Kage H, Shinozaki-Ushiku A, Ishigaki K, Sato Y, Tanabe M, Tanaka S, et al. Clinical utility of Todai OncoPanel in the setting of approved comprehensive cancer genomic profiling tests in Japan. Cancer Sci. 2023;114:1710–7. https://doi.org/10.1111/cas.15717.
Mur P, Viana-Errasti J, García-Mulero S, Magraner-Pardo L, Muñoz IG, Pons T, et al. Recommendations for the classification of germline variants in the exonuclease domain of POLE and POLD1. Genome Med. 2023;15:85. https://doi.org/10.1186/s13073-023-01234-y.
National Comprehensive Cancer Network® (NCCN®). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate. Version 3.2025. 2025. Available at: https://www.nccn.org.
National Comprehensive Cancer Network® (NCCN®). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, and Gastric. Version 4.2024. 2024. Available at: https://www.nccn.org.
National Comprehensive Cancer Network® (NCCN®). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Neuroendocrine and Adrenal Tumors. Version 1.2025. 2025. Available at: https://www.nccn.org.
Evans DG NF2-Related Schwannomatosis. In: Adam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, et al., editors. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1998. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1201/.
Lohmann DR, Gallie BL. Retinoblastoma. In: Adam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1998. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1452/.
Yamamoto H, Hirasawa A. Homologous recombination deficiencies and hereditary tumors. Int J Mol Sci. 2021;23:348 https://doi.org/10.3390/ijms23010348.
Matsubara N, Nishimura K, Kawakami S, Joung JY, Uemura H, Goto T, et al. Olaparib in patients with mCRPC with homologous recombination repair gene alterations: PROfound Asian subset analysis. Jpn J Clin Oncol. 2022;52:441–8. https://doi.org/10.1093/jjco/hyac015.
Yap TA, Ashok A, Stoll J, Mauer E, Nepomuceno VM, Blackwell KL, et al. Prevalence of germline findings among tumors from cancer types lacking hereditary testing guidelines. JAMA Netw Open. 2022;5:e2213070 https://doi.org/10.1001/jamanetworkopen.2022.13070.
Norquist BM, Harrell MI, Brady MF, Walsh T, Lee MK, Gulsuner S, et al. Inherited mutations in women with ovarian carcinoma. JAMA Oncol. 2016;2:482–90. https://doi.org/10.1001/jamaoncol.2015.5495.
Kurian AW, Hughes E, Handorf EA, Gutin A, Allen B, Hartman AR, et al. Breast and ovarian cancer penetrance estimates derived from germline multiple-gene sequencing results in women. JCO Precis Oncol. 2017;1:1–12. https://doi.org/10.1200/PO.16.00066.
Lilyquist J, LaDuca H, Polley E, Davis BT, Shimelis H, Hu C, et al. Frequency of mutations in a large series of clinically ascertained ovarian cancer cases tested on multi-gene panels compared to reference controls. Gynecol Oncol. 2017;147:375–80. https://doi.org/10.1016/j.ygyno.2017.08.030.
Carter NJ, Marshall ML, Susswein LR, Zorn KK, Hiraki S, Arvai KJ, et al. Germline pathogenic variants identified in women with ovarian tumors. Gynecol Oncol. 2018;151:481–8. https://doi.org/10.1016/j.ygyno.2018.09.030.
Loveday C, Turnbull C, Ramsay E, Hughes D, Ruark E, Frankum JR, et al. Germline mutations in RAD51D confer susceptibility to ovarian cancer. Nat Genet. 2011;43:879–82. https://doi.org/10.1038/ng.893.
Hu C, Polley EC, Yadav S, Lilyquist J, Shimelis H, Na J, et al. The contribution of germline predisposition gene mutations to clinical subtypes of invasive breast cancer from a clinical genetic testing cohort. J Natl Cancer Inst. 2020;112:1231–41. https://doi.org/10.1093/jnci/djaa023.
Breast Cancer Association Consortium, Mavaddat N, Dorling L, Carvalho S, Allen J, González-Neira A, et al. Pathology of tumors associated with pathogenic germline variants in 9 breast cancer susceptibility genes. JAMA Oncol. 2022;8:e216744 https://doi.org/10.1001/jamaoncol.2021.6744.
Breast Cancer Association Consortium, Dorling L, Carvalho S, Allen J, González-Neira A, Luccarini C, et al. Breast cancer risk genes - association analysis in more than 113,000 women. N Engl J Med. 2021;384:428–39. https://doi.org/10.1056/NEJMoa1913948.
Hu C, Hart SN, Gnanaolivu R, Huang H, Lee KY, Na J, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384:440–51. https://doi.org/10.1056/NEJMoa2005936.
Ramus SJ, Song H, Dicks E, Tyrer JP, Rosenthal AN, Intermaggio MP, et al. Germline mutations in the BRIP1, BARD1, PALB2, and NBN genes in women with ovarian cancer. J Natl Cancer Inst. 2015;107:djv214 https://doi.org/10.1093/jnci/djv214.
Weber-Lassalle N, Hauke J, Ramser J, Richters L, Groß E, Blümcke B, et al. BRIP1 loss-of-function mutations confer high risk for familial ovarian cancer, but not familial breast cancer. Breast Cancer Res. 2018;20:7. https://doi.org/10.1186/s13058-018-0935-9.
Rafnar T, Gudbjartsson DF, Sulem P, Jonasdottir A, Sigurdsson A, Jonasdottir A, et al. Mutations in BRIP1 confer high risk of ovarian cancer. Nat Genet. 2011;43:1104–7. https://doi.org/10.1038/ng.955.
Kimura T, Takahashi H, Okayasu M, Kido M, Inaba H, Kuruma H, et al. Time trends in histological features of latent prostate cancer in Japan. J Urol. 2016;195:1415–20. https://doi.org/10.1016/j.juro.2015.11.068.
Collaborators GPC. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019;4:934–47. https://doi.org/10.1016/S2468-1253(19)30347-4.
Rojas K, Stuckey A. Breast cancer epidemiology and risk factors. Clin Obstet Gynecol. 2016;59:651–72. https://doi.org/10.1097/GRF.0000000000000239.
Phung MT, Pearce CL, Meza R, Jeon J. Trends of ovarian cancer incidence by histotype and race/ethnicity in the United States 1992-2019. Cancer Res Commun. 2023;3:1–8. https://doi.org/10.1158/2767-9764.CRC-22-0410.
Momozawa Y, Sasai R, Usui Y, Shiraishi K, Iwasaki Y, Taniyama Y, et al. Expansion of cancer risk profile for BRCA1 and BRCA2 pathogenic variants. JAMA Oncol. 2022;8:871–8. https://doi.org/10.1001/jamaoncol.2022.0476.
Chen S, Liu Y. p53 involvement in clonal hematopoiesis of indeterminate potential. Curr Opin Hematol. 2019;26:235–40. https://doi.org/10.1097/MOH.0000000000000509.
Acknowledgements
We would like to express our gratitude to all individuals who indirectly contributed to this research. We also thank Dr. Shinji Kosugi for granting permission to use the Kosugi Group list in this study. This research was supported by AMED under Grant Number JP21km0908001 and by JSPS KAKENHI Grant Number 24K02584.
Funding
Open Access funding provided by The University of Tokyo.
Author information
Authors and Affiliations
Contributions
Conceptualization and Validation: EH, MO, KW, NA, HC, MK, AS, MT, MA, TI, ST, KT, HA, HK, KO. Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources: MO, KW, HK, KO. Funding acquisition: KO. Software and Visualization: EH. Supervision: MO, KW, HK, KO. Writing – original draft: EH, MO, KW, HK, KO. Writing – review & editing: EH, MO, KW, NA, HC, MK, AS, MT, MA, TI, ST, KT, HA, HK, KO.
Corresponding author
Ethics declarations
Competing interests
HK and KO received research funds from Konica Minolta, Inc. KO received research funds and lecture fees from Chugai Pharmaceutical Co. Ltd., AstraZeneca plc, and Takeda Pharmaceutical Co. Ltd. MO and KW are affiliated with an endowed chair funded by Konica Minolta, Inc. HA received advisor remuneration and research funds from Konica Minolta, Inc. and is affiliated with an endowed chair funded by Chugai Pharmaceutical Co. Ltd. MA and TI are employees of Konica Minolta, Inc. The other authors have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
10038_2025_1389_MOESM4_ESM.pdf
Supplementary Table 1. Disclosure Recommendation List of Germline Findings in Cancer Genomic Profiling Tests (Kosugi Group List ver.4.2)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Habano, E., Ogawa, M., Watanabe, K. et al. Germline pathogenic variants detected by GenMineTOP: insight from a nationwide tumor/normal paired comprehensive genomic profiling test, in Japan. J Hum Genet (2025). https://doi.org/10.1038/s10038-025-01389-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s10038-025-01389-z