Abstract
Intentional weight loss is often followed by unintentional weight regain. The causes of weight regain are uncertain but may include a myriad of responses that result in increased hunger and decreased energy expenditure. An individual’s psychological state and social and physical environments are also thought to influence weight regain in ways that can either support or derail weight loss maintenance. Funded by the National Institutes of Health, the Physiology of the WEight Reduced State (POWERS) study is a multi-center clinical trial aimed at describing the molecular, cellular, physiological, behavioral, environmental and psychosocial factors that may be associated with an individual’s ability to maintain their new weight after weight loss. This report provides the rationale for and describes the environmental, psychological and social determinants of health measures used in the POWERS study.
Similar content being viewed by others
Introduction
The Physiology of the WEight Reduced State (POWERS) study is a multi-center, longitudinal clinical trial in the United States. Its overarching goal is to explore the physiological basis for variability in weight regain among adults with obesity following intentional weight loss achieved through participation in a behavioral weight loss program. With extensive phenotyping, biospecimen collection, and qualitative assessments, the POWERS study is a discovery science initiative aimed at identifying pathways and predictors of the adaptations that occur after weight loss and their contributions to the heterogeneity of subsequent weight regain. Adults with obesity (N = 205; body mass index [BMI], 30– <40 kg/m2; 25– <60 y), are studied before, immediately following, and during the 12 months after weight loss. The current paper focuses on the environmental, psychological, and social determinants of health (SDoH) measures used in the study. Additional POWERS study design papers describe the study organization and overarching design [1], measures of energy balance [2], biomarkers [3], and behavioral constructs, which also address psychological constructs such as restrained eating and hedonic hunger [4].
Already complex at the biological level, many of the regulatory factors involved in weight regain after weight loss are likely attributed to individual differences in the molecular, cellular, physiological, psychological, and behavioral realms [2,3,4]. When investigating these regulatory factors, it is important to acknowledge two key features of the obesity epidemic. First, the rise in obesity is relatively recent; in the United States, the prevalence of obesity in adults increased from 15% in 1976–80 to 31% and 42% in 1999–2000 and 2020, respectively [5, 6]. Although a small decrease was observed in 2023 (46.0% in 2022 to 45.6% in 2023), obesity prevalence remains high [7]. Second, obesity is increasing in nations as they urbanize and industrialize [8]. Together, these facts suggest that weight cannot be considered solely an individual’s fate or a mere consequence of biology.
Excess weight and adiposity appear, in part, to be a community trait strongly tied to the various nested types of environments that an individual encounters, as well as the individual’s perceived place in these environments. Key environments and environmental characteristics that may be considered include: the home [9], family, and friends; employment, school [10], and faith groups [11]; cultural attitudes [12]; policies and laws [13]; ethnic, local, and regional variations in food availability [14]; and national-level food production [15] and distribution systems [16]. Healthy People 2030, a multi-pronged public health initiative of the United States government, underscores the importance of SDoH by specifying that one of its five overarching goals is to “create social, physical, and economic environments that promote attaining the full potential for health and well-being for all” [17]. SDoH are defined as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks” [8]. While little data exists on the social determinants affecting weight regain after weight loss, national surveys cast some light on potential contributors to obesity. In a study using 2013 to 2017 data from the National Health Interview Survey, an aggregate SDoH score—derived from 38 factors grouped into six categories (economic stability, neighborhood, physical environment, social cohesion, community and social context, food insecurity, education, and health care system)—was found to be strongly associated with obesity, independent of clinical and demographic factors [18]. Compared with the quartile with the fewest SoDH-related challenges, the quartile with the greatest had a 50% higher prevalence of obesity class 1 (BMI 30–<35 kg/m2) [18]. Some SDoH are becoming less relevant over time as obesity affects more US adults; for example, National Health and Nutrition Examination Survey data show that between 2015 and 2020, obesity increased more rapidly in individuals with higher versus lower incomes, such that by 2020, there was little difference in obesity prevalence among these groups [19].
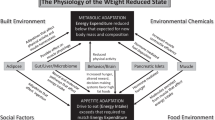
Food, neighborhood, family and social environmental factors may influence an individual’s behaviors and physical health directly and via psychological processes (Fig. 1). Such factors can manifest in health-related behaviors like diet and physical activity or exert their influence directly via neuroendocrine changes. Importantly, these health-related behaviors or reactions can be protective of health (e.g., resiliency, a sense of purpose) or pose risk to health (e.g., stress, anxiety, depressive symptoms, helplessness, loneliness) [20,21,22].
The balance between energy intake due to eating and energy expenditure due to physical activity, thermic effect of food, and resting energy expenditure determines weight and the ability to maintain reduced weight after weight loss. The regulation of body weight via energy intake and expenditure is influenced by intrinsic factors such as psychological traits and personality factors, as listed in the figure. These are in turn influenced by a variety of environmental extrinsic factors that include socioeconomic, food, neighborhood, family and social environments.
Given the tight interaction between SDoH, psychological and environmental factors, the unique contribution of one factor to an observable trait—such as hormone levels under conditions of stress [23, 24], restraint during eating [25, 26], or preferences for particular foods [27]—may be difficult to extract. Mechanisms affected by environmental, social, and psychological factors leading to heterogeneity in weight regain after weight loss are likely to include the following:
-
cost and types of food and access to food, including gardens, grocery stores, and farmer’s markets [28, 29];
-
local social norms (family and community) about meals and snacking, food preparation, body weight, and appearance [30, 31];
-
safe housing, transportation, and neighborhoods [32,33,34,35];
-
access to safe spaces for exercise (e.g., parks and gyms) [36, 37];
-
income inequality, education, job opportunities, language fluency [32, 38, 39];
-
access to health care and resources for disease prevention [41, 42];
-
experiences of stress, anxiety, depression, loneliness, hope, etc. [43,44,45,46]; and
-
unknown potential environmental contributors (e.g., pollution, environmental toxins, food additives) [47, 48].
Assessment tools
The POWERS study carefully compiled, validated and investigator-created questionnaires to collect data on SDoH, (socioeconomic status, neighborhood, food, family and social environments), and psychological variables with particular relevance to weight regain following weight loss. Many of the questionnaires were drawn from the Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) initiative, as a parsimonious set of questionnaires recommended for inclusion in the assessment of response to weight loss treatment [49]. A list of these questionnaires, as well as administration time and other specifics, is provided in Table 1. Behavioral and psychological measures related to food intake, physical activity and weight collected in the POWERS study are described in Mayer et al. [4]. These include the Coping subscale from the Palatable Eating Motives Scale, which measures emotional eating, the Power of Food Scale, which measures hedonic hunger, and the Weight Bias Internalized Scale, which measures internalization of negative weight stereotypes.
Ethics approval and consent to participate
The protocol and informed consent forms were approved by the single Institutional Review Board at the University of Pittsburgh (CR21120046-021). All participants undergo informed consent prior to enrolling in the study described in this manuscript.
Questionnaires are completed by participants using a web-based data entry system, except for questions on perception of familial body shape, which are completed on paper. The participant may complete web-based questionnaires using any device (e.g., tablet, phone, computer) with internet access. If a participant prefers not to use a device or has challenges accessing an online portal, questionnaires are provided for completion on paper. Most questionnaires are completed during each of the study's four assessment periods: before weight loss intervention (BL); following stabilization of a new, lower weight of at least 7% below baseline weight (T0); and at 4 (T4) and 12 (T12) months after weight stabilization. Exceptions are noted below. Questionnaires must be started and completed during the corresponding assessment period, and applicable questionnaires may be completed at home.
Most of the instruments described below have been used in a variety of contexts to study associations with weight and weight loss. The unique contribution of POWERS is to combine them with rigorous physiological and molecular measures to longitudinally study the dynamic state of weight maintenance following weight loss, with a goal of identifying factors that strongly correlate with an individual's ability to maintain weight loss.
The POWERS Demographics Form captures participant-level-information, including on socio-economic status. In addition, zip code information from the demographics form will help to assess geographic area-level characteristics, including built environment and food environment.
The Neighborhood Environment Measures Survey-Perceived (NEMS-P) Core Items is a 19-item survey that assesses three dimensions of a person's perceived food environment [50]. Dimension one covers the community nutrition environment, with questions about the type, location, and accessibility of stores and restaurants within a person's neighborhood; dimension two assesses consumer nutrition environments, with questions about healthy food options (e.g., fruits and vegetables), and the price, promotion, and nutrition information within stores and restaurants; and dimension three covers the home food environment, with questions about the availability and accessibility of healthy and unhealthy foods in the home (e.g., ready-to-eat foods in the refrigerator or on the counter).
Some survey items in NEMS-P, notably those on household food environment, are relevant to understanding trends in weight management and may indicate one’s ability to adhere to lifestyle weight loss interventions. Information on an individual’s perceived food environment can provide valuable insight into dietary choices that ultimately affect weight status. In a study by Alber et al., higher perceived food quality in the home was associated with higher fruit and vegetable intake. Interestingly, the study also linked BMI with perceived fruit and vegetable price, with a higher BMI being associated with a higher perception of costs [51]. By capturing valuable measures like the perceived cost of produce, NEMS-P provides information on the overall perception of access to quality food, which may have implications for individual food choices and dietary intake. Modifications to the home food environment, therefore, provide a potential avenue to prevent weight regain.
The NIH Toolbox General Life Satisfaction Survey-B is a 5-item tool that assesses global feelings and attitudes about one’s life [52]. Items are rated on a five-point Likert scale, with response options ranging from “strongly disagree” to “strongly agree.” Items are summed to yield a total score, with higher scores indicative of greater general life satisfaction. Scores ≥1 standard deviation (SD) below the mean (T ≤ 40) suggest low levels of general life satisfaction, and scores ≥1 SD above the mean (T ≥ 60) suggest high levels of general life satisfaction.
General life satisfaction can arise from a multitude of life factors. In a large dataset, Kuroki found that the correlation between BMI and life satisfaction is modulated by different confounding factors. For example, the negative association between life satisfaction and being overweight is only statistically significant when socio-economic characteristics are controlled for, whereas it lacks significance when exogenous variables are controlled for exclusively [53]. Use of the General Life Satisfaction Survey for the analyses of predictors of weight regain may warrant its combination with other demographic or lifestyle questionnaires to better characterize the source of one’s relative satisfaction with life and its relationship with weight status.
The NIH Toolbox Meaning and Purpose Survey is a 7-item tool that assesses the extent to which people feel their life matters or makes sense [54]. Items are rated on a five-point Likert scale, with response options ranging from “strongly disagree” to “strongly agree.” Items are summed to yield a total score, with higher scores indicative of more meaning and purpose. Scores ≥1 SD below the mean (T ≤ 40) suggest low levels of meaning and purpose, and scores ≥1 SD above the mean (T ≥ 60) suggest high levels of meaning and purpose.
The degree of an individual’s self-perceived meaning and purpose in life may have large implications for their ability to maintain health or regulate weight. Participants who perceive their life as lacking meaning or purpose may struggle with self-efficacy and regulating energy intake. They also may not see the value in making healthy dietary choices, potentially leading to weight regain. Conversely, those who believe that their life is important and has purpose are more likely to take active steps in maintaining their health [55,56,57].
The Center for Epidemiological Studies-Depression (CES-D) is a 20-item measure that asks respondents to rate how often over the past week they experienced symptoms associated with depression, such as depressed mood, feelings of guilt and worthlessness, feelings of helplessness and hopelessness, psychomotor retardation, restless sleep, poor appetite, and feeling lonely [58]. Items are rated on a 4-point Likert scale, with response options ranging from “rarely or none of the time” to “most or almost all the time.” Total scores range from 0 to 60, with higher scores indicating greater depressive symptoms. Four domains are commonly recognized for this scale: Depressive Affect (7 items), Positive Affects (4 items), Somatic Complaints/Activity Inhibition (7 items), and Interpersonal Difficulties (2 items), however, the domains are not scored separately [59].
Major depression can be associated with weight loss or weight gain. The CES-D provides useful data to explore which elements of depression correlate with adiposity. Sutin and Zonderman investigated this link with participants from the Baltimore Longitudinal Study of Aging by modeling the trajectory of adiposity and depressive symptoms over adulthood using BMI, waist circumference, and hip circumference. The relationship between adiposity and depressive symptoms was found to be partially moderated by sex: women with depressive symptoms had greater increases in BMI compared to their male counterparts when controlling for other covariates like demographics [60]. Evaluating the separate relationship of the positive and negative affects collected using the CES-D in relation to weight loss maintenance may provide valuable insights into factors associated with success or challenges.
The Spielberger State-Trait Anxiety Inventory (STAI) is a commonly used measure of trait and state anxiety [61] included in ADOPT [49]. It includes 40 items, with half assessing trait anxiety and the other half assessing state anxiety. Examples of state anxiety items include “I am tense; I am worried” and “I feel calm; I feel secure.” Examples of trait anxiety items include “I worry too much over something that really doesn’t matter” and “I am content; I am a steady person.” All items are rated on a four-point Likert scale (e.g., from “almost never” to “almost always”). Scores for each of the trait and state subscales range from 20 to 80, with higher scores indicating greater anxiety.
As with depression, anxiety can be associated with changes in appetite and food intake. Thus, when studying weight loss and maintenance, it is critical to understand an individual’s trait and state anxiety in the context of eating behavior. Schneider et al. investigated the link between anxiety and eating behavior in individuals with normal weight or obesity by evaluating the food intake of participants after implementing tasks designed to induce specific emotions. Using STAI, the study found that trait anxiety is positively associated with food intake in individuals with obesity, but not those who are lean, following an event that induces anxiety. The study postulates that individuals with obesity may use food to cope with stressful events [62].
The Perceived Stress Scale (PSS-10) is a 10-item questionnaire included in ADOPT [49] that measures perceived stress during the past month [63]. It was designed to measure how often people experience events that are perceived as unpredictable or uncontrollable. Items are rated on a five-point Likert scale and summed to yield a total score ranging from 0 to 40, with higher scores indicating higher stress.
Stress can alter our dietary patterns and eating habits. Notably, the degree to which stress can cause under- or over-eating may be influenced by the severity of the stressor. Chronic life stress is associated with greater preference for foods dense in nutrients and high in sugar and fat [64]. Longitudinal studies show that chronic life stress may be causally linked to weight gain, with stress-induced eating as a factor contributing to obesity [64]. The Prevention of Diabetes through Lifestyle Intervention and Population Studies in Europe and around the World (PREVIEW), conducted in adults with overweight and prediabetes, featured a 6-month weight loss intervention phase followed by a 2.5-year weight maintenance phase. The study found that higher perceived stress at 6 months (i.e., post-weight loss) was associated with higher disinhibition (i.e., the disposition to overeat in the face of “certain external and internal stimuli”) and inhibited flexible restraint (i.e., the ability to incorporate control of overeating into one’s lifestyle without depriving oneself). Reductions in flexible restraint were most apparent in participants who did not experience successful weight reduction [65], which may suggest these eating behaviors act as a mechanism by which perceived stress can impact weight regulation. People experiencing high stress may have difficulty making mindful food choices, perhaps due to preoccupation with their stressors.
The Barratt Impulsiveness Scale (BIS-11) is a 30-item self-report instrument designed to assess the behavioral construct of impulsiveness [66]. The BIS-11 assesses 3 s-order factors (attentional, motor, non-planning) and 6 first-order factors (attention, cognitive instability, motor, perseverance, self-control, cognitive complexity). It is one of the most common self-report measures of impulsiveness in research and clinical settings. Items are rated on a four-point Likert scale, from “rarely/never” to “almost always/always.” Items are summed to yield a total score, ranging from 30 to 120 points, with higher scores indicating higher impulsiveness.
Higher levels of impulsiveness have been reported to be positively associated with alcohol consumption, appetizer consumption, higher caloric intake, and overall unhealthy eating; they have been negatively associated with the consumption of fruit and vegetables, meat and poultry, processed meat, dairy products, milk-based desserts, and starchy foods [67]. Impulsiveness also has been shown to be positively associated with snacking and risk of eating disorders (e.g., bulimia nervosa, hyperphagic disorders) [67]. The BIS-11 has the potential to capture degrees of impulsiveness in relation to weight regain and dietary habits in participants post-intervention. Since higher caloric intake has been associated with impulsiveness, the BIS-11 also may serve as a predictor of weight regain.
The Monetary Choice Questionnaire (MCQ) is a 27-item survey in which the participant chooses between a smaller, immediate monetary reward and a larger, delayed monetary reward. The questionnaire is scored by calculating where the respondent’s answers place them within the context of reference discounting curves as indicated by a “k value.” k typically falls between 0.0 and 0.5, with smaller values indicating a lack of discounting and preference for delayed rewards and higher values indicating strong discounting and a preference for immediate rewards. Thus, higher values of k are indicative of higher levels of impulsivity [68]. The score is moderately associated (d ~ 0.4–0.6) with a broad range of addictive behaviors and can predict initiation of substance use [69, 70]. Notably, the MCQ is highly correlated (r = 0.82) with computer-based experimental methods.
The degree to which one values immediate versus delayed gratification may have a significant influence on eating behaviors. Lim and Bruce administered the MCQ, as well as an adapted version of the MCQ using weight loss as a reward, to 42 participants who expressed a desire to lose weight. The study found that participants who preferred receiving smaller but more proximate sums of money also preferred smaller but sooner weight loss [71]. Other studies have supported the idea that individuals with obesity score higher, on average, for temporal monetary discounting (preference for smaller, sooner rewards) [72]. Those who place more value on immediate pleasure in general also may choose more tasty, high-calorie options, in contrast to the delayed reward of long-term weight maintenance. Similarly, individuals who prefer immediate/sooner rewards may be less likely to tolerate the negative affective state of hunger, potentially resulting in poor adherence to dietary restrictions. In theory, such inclinations could be an important predictor of weight regain.
The USDA Food Insecurity Survey, developed by the United States Department of Agriculture, was used to assess the food environment. This instrument, featuring a subset of questions from the 18-item standard module, collects data on the prevalence of food insecurity or insufficiency in the respondent’s household [73].
Studies corroborate the general association between food insecurity and BMI; findings support the idea that more feasible access to affordable, low-quality foods may partially mediate the association between poverty and higher overall BMI [74]. However, extensive longitudinal studies that validate a mechanistic explanation for this phenomenon do not yet exist [75].
Two study-investigator-created surveys and the Questionnaire on Eating and Weight Patterns-5 (QEWP-5, and is described in Mayer et al. [4]) were used to collect information about family and environment. The study-investigator-created surveys include a demographics form and a substance use survey.
The POWERS Demographics Form, created by POWERS study investigators, captures the participant’s date of birth, gender identity, relationship status, number of children and adults living in the home, household income, student status, highest completed level of education, current employment status, type of health insurance, and zip code. Biological sex, ethnicity, and race are obtained by interview during the screening process. When possible, questions and response sets were selected or adapted from sources such as the 2020 US Census and the American Community Survey [76].
The variety of data obtained from the demographics form and screening process can provide valuable information on access to quality food and dietary practices associated with culture or socioeconomic status. A participant’s zip code can provide information on their ability to access quality foods, which may affect their ability to adhere to a healthy diet geared toward weight maintenance. One’s occupation, education, or household income also provides valuable socioeconomic data that can serve as an indicator of the quality and affordability of foods or whether they dictate weight maintenance efforts. Cultural and ethnic information can shed light on certain dietary staples that are heavily integrated into a participant’s diet; the nutritional quality and macronutrient quantity of these staples can then be evaluated to indicate the potential drivers of a participant’s weight regulation.
The Substance Use Survey was created from questions developed by the Centers for Disease Control and Prevention and asked on the Behavioral Risk Factor Surveillance System (BRFSS) [77] to assess tobacco, marijuana, and alcohol use. Study instruments providing temporal context to substance use in relation to weight status may clarify the interplay between BMI and substance use. For example, increased food consumption and weight gain are common following cessation of many addictive substances, such as nicotine [78]. Substance use surveys also could be used to quantify disposition to addictive behaviors, which may be evaluated alongside measures of binge eating as well as other behavioral measures collected in the POWERS study [4] to serve as a potential explanation for weight status. In this sense, common mechanisms between substance addiction and addictive dietary habits could mediate an observed association between substance use and weight regain.
The participant’s perception of biological parental body build is from the QEWP-5 questionnaire. Highest parental weight status is assessed through silhouettes, giving one measure of obesity in the ancestors of the participant. Parental weight can help explain the response of an individual to post-intervention weight regain. Some individuals may have a predisposition to obesity and adiposity based on genetic ancestry. People also may adopt lifestyle behaviors from their parents that may be indicative of current weight status or poor eating habits [79, 80].
Statistical analysis
The statistical analysis used for measures of environmental, psychological and SDoH will employ the same methods as other data collected in POWERS, which is described here and in the overview paper [1].
The primary analysis aims to identify factors associated with weight change using regression models with least absolute shrinkage and selection operator for variable selection and estimation. The independent variables will be expressed as:
-
1.
Observed values at different timepoints
-
2.
Absolute and percent changes between assessments
-
3.
Trajectories using latent group-based trajectory models
-
4.
For some variables, integrated values over the entire observation period.
Integrative (Causal) analysis
We will explore the use of probabilistic graphical models to collectively analyze data from different modalities (e.g., physiological, molecular, behavioral) to identify networks of complex potential cause-effect relations between variables across datasets. Probabilistic graphical models can identify confounding variables and distinguish direct (“causal”) relations from simple correlates. They can be used to select the most informative variables around any outcome variable to build an efficient classifier that uses a subset of the potential variables.
Summary
Recent weight and BMI trends clearly indicate that many Americans are susceptible to weight gain in their current environment. This statistic accompanies the fact that an individual is unique and complex with regard to biology, personality, preferences, and experience. Each individual likely faces different challenges when it comes to their weight and other health needs. As evidence, many people can lose weight temporarily using one of the available lifestyle, surgical, or pharmaceutical therapies, but there is enormous interindividual variability in weight regain over longer timeframes. We know that psychological and environmental factors and SDoH correlate with weight status and are therefore part of the rich menu of factors underlying obesity. These non-physiological factors, combined with an altered physiological state that supports weight regain, are very likely to be key players in variable success with weight maintenance. By better understanding the relationships between psychological, social, environmental, behavioral and biological factors, we hope to develop the tools to tailor weight maintenance interventions to the individual, thereby increasing the likelihood of success.
References
Belle SH, Gallagher D, Roberts SB, Laughlin MR, Das SK, Whyte KJ, et al. The Physiology Of the WEight Reduced State (POWERS) Study: overview and study design. Int J Obes. 2025 (Submitted for publication).
Rosenbaum M, Allison KC, Laughlin MR, Whyte K, Jakicic JM, Mayer LES, et al. The Physiology Of the WEight Reduced State (POWERS) Study: assessing energy balance. Int J Obes. 2025 (Submitted for publication).
Rosenbaum M, Allison KC, Laughlin MR, Kelley SS, Nunez-Matos J, Rickels M, et al. The Physiology Of the WEight Reduced State (POWERS) Study: strategies for the analysis of biological specimens. Int J Obes. 2025 (Submitted for publication).
Mayer LES, Lowe M, Allison KC, Ashby-Thompson M, Benasi G, Burger KS, et al. The Physiology Of the WEight Reduced State (POWERS) Study: design and rationale for assessment of food intake, physical activity and other behavioral constructs. Int J Obes. 2025 (Submitted for publication).
Adult Obesity Facts: Centers for Disease Control and Prevention; 2024 [Available from: https://www.cdc.gov/obesity/adult-obesity-facts/index.html.
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats [Internet]. 2021. Available from: https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/overweight-obesity-adults-H.pdf.
Rader B, Hazan R, Brownstein JS. Changes in adult obesity trends in the US. JAMA Health Forum. 2024;5:e243685.
Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33:673–89.
Emery CF, Olson KL, Lee VS, Habash DL, Nasar JL, Bodine A. Home environment and psychosocial predictors of obesity status among community-residing men and women. Int J Obes. 2015;39:1401–7.
Chandran A, Burjak M, Petimar J, Hamra G, Melough MM, Dunlop AL, et al. Changes in body mass index among school-aged youths following implementation of the Healthy, Hunger-Free Kids Act of 2010. JAMA Pediatr. 2023;177:401–9.
Cline KM, Ferraro KF. Does religion increase the prevalence and incidence of obesity in adulthood?. J Sci Study Relig. 2006;45:269–81.
Dao MC, Thiron S, Messer E, Sergeant C, S‚vign‚ A, Huart C. et al. Cultural influences on the regulation of energy intake and obesity: a qualitative study comparing food customs and attitudes to eating in adults from France and the United States. Nutrients. 2021;13:63.
Elbel B, Mijanovich T, Dixon LB, Abrams C, Weitzman B, Kersh R, et al. Calorie labeling, fast food purchasing and restaurant visits. Obesity. 2013;21:2172–9.
Chen M, Creger T, Howard V, Judd SE, Harrington KF, Fontaine KR. Association of community food environment and obesity among US adults: a geographical information system analysis. J Epidemiol Community Health. 2019;73:148–55.
Crimarco A, Landry MJ, Gardner CD. Ultra-processed foods, weight gain, and co-morbidity risk. Curr Obes Rep. 2022;11:80–92.
Na M, Sliwinski MJ, Kris-Etherton PM. Food insufficiency, supplemental nutrition assistance program status, and variability in weight and body composition: longitudinal analysis of the national health and aging trends study cohort 2012-2021. Am J Clin Nutr. 2025;121:463–9.
Healthy People 2030: Social Determinants of Health: Office of Disease Prevention and Health Promotion; Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health.
Javed Z, Valero-Elizondo J, Maqsood MH, Mahajan S, Taha MB, Patel KV, et al. Social determinants of health and obesity: findings from a national study of US adults. Obesity. 2022;30:491–502.
Liu M, Aggarwal R, Zheng Z, Yeh RW, Kazi DS, Joynt Maddox KE, et al. Cardiovascular health of middle-aged U.S. adults by income level, 1999 to March 2020: a serial cross-sectional study. Ann Intern Med. 2023;176:1595–605.
Thomas K, Nilsson E, Festin K, Henriksson P, Lowén M, Löf M, et al. Associations of psychosocial factors with multiple health behaviors: a population-based study of middle-aged men and women. Int J Environ Res Public Health. 2020;17:1239.
Das SK, Mason ST, Vail TA, Blanchard CM, Chin MK, Rogers GT, et al. Sustained long-term effectiveness of an energy management training course on employee vitality and purpose in life. Am J Health Promot. 2020;34:177–88.
Rannaud-Bartaire P, Demeneix BA, Fini JB. Pressures of the urban environment on the endocrine system: adverse effects and adaptation. Mol Cell Endocrinol. 2024;583:112125.
van der Valk ES, Savas M, van Rossum EFC. Stress and obesity: are there more susceptible individuals?. Curr Obes Rep. 2018;7:193–203.
Hackett RA, Gareddu A, Panagi L, Steptoe A, Poole L. Dysregulated responses to stress and weight in people with type 2 diabetes. J Psychosom Res. 2023;170:111354.
Flack KD, Anderson III RE, McFee KF, Day BT. Characterizing motor impulsivity of individuals classified as overweight to obese. Sports Med Health Sci. 2023;5:314–8.
Saelens BE, Melhorn SJ, Rowland MG, Scholz K, De Leon MRB, Elfers CT, et al. General and food-specific impulsivity and inhibition related to weight management. Child Obes. 2022;18:84–91.
Spinelli S, Monteleone E. Food preferences and obesity. Endocrinol Metab. 2021;36:209–19.
Wilde PE, Peterman JN. Individual weight change is associated with household food security status. J Nutr.2006;136:1395–400.
Myers CA, Mire EF, Katzmarzyk PT. Trends in adiposity and food insecurity among U.S. adults. JAMA Netw Open. 2020;3:e2012767.
Leahey TM, Gokee LaRose J, Fava JL, Wing RR. Social influences are associated with BMI and weight loss intentions in young adults. Obesity. 2011;19:1157–62.
Nolan LJ, Eshleman A. Paved with good intentions: Paradoxical eating responses to weight stigma. Appetite. 2016;102:15–24.
Xiao Q, Myott E, Schlundt DG, Stancil W. Association of neighborhood economic trajectories with changes in weight status among black and white adults in the Southeastern US. JAMA Netw Open. 2022;5:e2230697.
Kim SJ, Blesoff JR, Tussing-Humphrys L, Fitzgibbon ML, Peterson CE. The association between neighborhood conditions and weight loss among older adults living in a large urban city. J Behav Med. 2023;46:882–9.
Duran AC, Zenk SN, Tarlov E, Duda S, Smith G, Lee JM, et al. Foreclosures and weight gain: differential associations by longer neighborhood exposure. Prev Med. 2019;118:23–9.
Sugiyama T, Ding D, Owen N. Commuting by Car: weight gain among physically active adults. Am J Prev Med. 2013;44:169–73.
Stark JH, Neckerman K, Lovasi GS, Quinn J, Weiss CC, Bader MD, et al. The impact of neighborhood park access and quality on body mass index among adults in New York City. Prev Med. 2014;64:63–8.
Phelan S, Liu T, Gorin A, Lowe M, Hogan J, Fava J, et al. What distinguishes weight-loss maintainers from the treatment-seeking obese? Analysis of environmental, behavioral, and psychosocial variables in diverse populations. Ann Behav Med. 2009;38:94–104.
Brown WJ, Flores TR, Keating SE, Mielke GI. Trajectories and determinants of weight gain in two cohorts of young adult women born 16 years apart. Int J Obes. 2021;45:1553–64.
Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29:470–7.
Gee GC, Ro A, Gavin A, Takeuchi DT. Disentangling the effects of racial and weight discrimination on body mass index and obesity among Asian Americans. Am J Public Health. 2008;98:493–500.
Roser P, Bajaj SS, Stanford FC. International lack of equity in modern obesity therapy: the critical need for change in health policy. Int J Obes. 2022;46:1571–2.
Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB. Regional disparities in obesity prevalence in the United States: a spatial regime analysis. Obesity. 2015;23:481–7.
Konttinen H, van Strien T, Männistö S, Jousilahti P, Haukkala A. Depression, emotional eating and long-term weight changes: a population-based prospective study. Int J Behav Nutr Phys Act. 2019;16:28.
Brumpton B, Langhammer A, Romundstad P, Chen Y, Mai XM. The associations of anxiety and depression symptoms with weight change and incident obesity: the HUNT study. Int J Obes. 2013;37:1268–74.
Kelsey KS, DeVellis BM, Gizlice Z, Ries A, Barnes K, Campbell MK. Obesity, hope, and Health: findings from the HOPE Works Community Survey. J Community Health. 2011;36:919–24.
Henriksen RE, Nilsen RM, Strandberg RB. Loneliness as a risk factor for metabolic syndrome: results from the HUNT study. J Epidemiol Community Health. 2019;73:941–6.
Wang Y, Tan H, Zheng H, Ma Z, Zhan Y, Hu K, et al. Exposure to air pollution and gains in body weight and waist circumference among middle-aged and older adults. Sci Total Environ. 2023;869:161895.
Kladnicka I, Bludovska M, Plavinova I, Muller L, Mullerova D. Obesogens in foods. Biomolecules. 2022;12:680.
Saelens BE, Arteaga SS, Berrigan D, Ballard RM, Gorin AA, Powell-Wiley TM, et al. Accumulating data to optimally predict obesity treatment (ADOPT) core measures: environmental domain. Obesity. 2018;26:S35–S44.
Green SH, Glanz K. Development of the perceived nutrition environment measures survey. Am J Prev Med. 2015;49:50–61.
Alber JM, Green SH, Glanz K. Perceived and observed food environments, eating behaviors, and BMI. Am J Prev Med. 2018;54:423–9.
Salsman JM, Butt Z, Pilkonis PA, Cyranowski JM, Zill N, Hendrie HC, et al. Emotion assessment using the NIH Toolbox. Neurology. 2013;80:S76–86.
Kuroki M. Life satisfaction, overweightness and obesity. Int J Wellbeing. 2016;6:93–110.
Salsman JM, Schalet BD, Park CL, George L, Steger MF, Hahn EA, et al. Assessing meaning & purpose in life: development and validation of an item bank and short forms for the NIH PROMIS(®). Qual Life Res. 2020;29:2299–310.
Kim ES, Shiba K, Boehm JK, Kubzansky LD. Sense of purpose in life and five health behaviors in older adults. Prev Med. 2020;139:106172.
Fernqvist F, Spendrup S, Tellström R. Understanding food choice: a systematic review of reviews. Heliyon. 2024;10:e32492.
Berkowitz L, Mateo C, Salazar C, Samith B, Sara D, Pinto V, et al. Healthy eating as potential mediator of inverse association between purpose in life and waist circumference: emerging evidence from US and Chilean cohorts. Int J Environ Res Public Health. 2023;20:7099.
Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. J Clin Psychol. 2006;62:123–46.
Sutin AR, Zonderman AB. Depressive symptoms are associated with weight gain among women. Psychol Med. 2012;42:2351–60.
Spielberger C, Gorsuch R, Lushene R, Vagg PR, Jacobs G. Manual for the State-Trait Anxiety Inventory (Form Y1 – Y2) 1983. Publisher: Palo Alto, CA: Consulting Psychologists Press.
Schneider KL, Appelhans BM, Whited MC, Oleski J, Pagoto SL. Trait anxiety, but not trait anger, predisposes obese individuals to emotional eating. Appetite. 2010;55:701–6.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–94.
Jalo E, Konttinen H, Westerterp-Plantenga M, Adam T, Drummen M, Huttunen-Lenz M, et al. Perceived stress as a predictor of eating behavior during the 3-year PREVIEW lifestyle intervention. Nutr Diab. 2022;12:47.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74.
Bénard M, Bellisle F, Kesse-Guyot E, Julia C, Andreeva VA, Etilé F, et al. Impulsivity is associated with food intake, snacking, and eating disorders in a general population. Am J Clin Nutr. 2019;109:117–26.
Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87.
Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking?. Drug Alcohol Depend. 2009;103:99–106.
MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology. 2011;216:305–21.
Lim SL, Bruce AS. Can’t wait to lose weight? Characterizing temporal discounting parameters for weight-loss. Appetite. 2015;85:8–13.
Bickel WK, George Wilson A, Franck CT, Terry Mueller E, Jarmolowicz DP, Koffarnus MN, et al. Using crowdsourcing to compare temporal, social temporal, and probability discounting among obese and non-obese individuals. Appetite. 2014;75:82–9.
U.S. Household Food Security Survey Module: Six-Item Short Form. Food Security in the US—Survey Tools [Internet]. 2024. Available from: https://www.ers.usda.gov/sites/default/files/_laserfiche/DataFiles/50764/short2024.pdf.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16.
Carvajal-Aldaz D, Cucalon G, Ordonez C. Food insecurity as a risk factor for obesity: a review. Front Nutr. 2022;9:1012734.
American Community Survey: United States Census Bureau; 2019 [Available from: https://data.census.gov/cedsci/table?d=ACS%201-Year%20Estimates%20Data%20Profiles&tid=ACSDP1Y2019.DP05.
Behavioral Risk Factor Surveillance System Survey Questionnaire. BRFSS Questionnaires [Internet]. 2020.
Sahle BW, Chen W, Rawal LB, Renzaho AMN. Weight gain after smoking cessation and risk of major chronic diseases and mortality. JAMA Netw Open. 2021;4:e217044.
Ellis JM, Galloway AT, Webb RM, Martz DM, Farrow CV. Recollections of pressure to eat during childhood, but not picky eating, predict young adult eating behavior. Appetite. 2016;97:58–63.
Crossman A, Anne Sullivan D, Benin M. The family environment and American adolescents’ risk of obesity as young adults. Soc Sci Med. 2006;63:2255–67.
Acknowledgements
POWERS was funded as a Cooperative Agreement between the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the NIH Offices of Disease Prevention (ODP), Behavior and Social Science Research (OBSSR), and Nutrition Research (ONR) to the following investigators: Rudolph L. Leibel, MD [Contact], Dympna Gallagher, EdD, Laurel Mayer, MD, Michael Rosenbaum, MD (UH3 DK128302); MRL PhD [Contact], Kelly Allison, PhD, Matthew Hayes, PhD, Susan Roberts, PhD (UH3 DK128298); and Steven H. Belle, PhD, MScHyg (U24 DK128125). Additional funding to support this study was provided to Panayiotis V. Benos, PhD (R01 HL159805), Rudolph L. Leibel, MD (P30 DK026687 Human Phenotyping Core, Molecular Biology Molecular Genetics Core), Muredach Reilly, MBBCh, MSCE (UL1TR001873 Clinical Research Resource; Bionutrition Unit), Dympna Gallagher, EdD (T32 DK007559 in support of Giada Benasi, PhD and K26 DK138418), and Anthony W. Ferrante, MD, PhD (Hunter Eastman Fellowship in Translational Research in support of Maxine Ashby-Thompson, EdD). Roger A Fielding, PhD was partially supported by the US Department of Agriculture (USDA), under agreement No. 58-8050-9-004, by NIH Boston Claude D. Pepper Center (OAIC; 1P30AG031679) and Sai Krupa Das was supported by the USDA Agricultural Research Service Cooperative Agreements # 58-8050-9-004 and # 1950-51000-071-01S. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the views of the USDA. We also thank the University of Pennsylvania Diabetes Research Center (DRC) for the use of the Radioimmunoassay Core (NIH DK019525). The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5-UL1-TR-001878-09. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additional support was provided by the Robard Corporation, Mt Laurel, New Jersey, which supplied Numetra meal replacement products.
Author information
Authors and Affiliations
Consortia
Contributions
All authors participated in designing the protocol. SKD and MRL were responsible for designing and preparing the manuscript and critically reviewing it prior to submission. WCK, SZY, GB, SSK, LESM, JMJ, KW, MRL and SBR were responsible for reviewing the manuscript and providing edits.
Corresponding author
Ethics declarations
Competing interests
Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and are not to be construed as reflecting the views of the of the National Institutes of Health, Department of Health and Human Services, United States Department of Agriculture or employers of the authors. Dr. Jakicic is a member of the Scientific Advisory Board for Wondr Health, Inc., and his institution received research funding from Epitomee Medical, Inc. Dr. Yanovski reports that her spouse has received research project support to his Institution from Soleno Therapeutics and Rhythm Pharmaceutical and receives medication for studies from Hikma Pharmaceuticals and Versanis Bio. Dr. Whyte is partially funded by Eli Lilly & Company. Dr. Lowe receives licensing fees for the Power of Food Scale, but not from the POWERS consortium. Dr. Roberts is a Board member of Danone and founder of www.theidiet.com. The remaining authors declare no competing financial interests.
Ethics
The protocol and informed consent forms were approved by the single Institutional Review Board at the University of Pittsburgh (CR21120046-021). All participants will undergo informed consent prior to enrolling in the study described in this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Das, S.K., Benasi, G., Jakicic, J.M. et al. The Physiology of the WEight-Reduced State (POWERS) study: environmental, psychological, and social determinants of health. Int J Obes 50, 166–173 (2026). https://doi.org/10.1038/s41366-025-01911-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01911-5
This article is cited by
-
The Physiology Of the WEight Reduced State (POWERS) study: design and rationale for assessment of food intake, physical activity and other behavioral constructs
International Journal of Obesity (2026)