Abstract
Radiochemotherapy-induced oral mucositis (OM) is a common oral complication in patients with tumors following head and neck radiotherapy or chemotherapy. Erosion and ulcers are the main features of OM that seriously affect the quality of life of patients and even the progress of tumor treatment. To date, differences in clinical prevention and treatment plans for OM have been noted among doctors of various specialties, which has increased the uncertainty of treatment effects. On the basis of current research evidence, this expert consensus outlines risk factors, clinical manifestations, clinical grading, ancillary examinations, diagnostic basis, prevention and treatment strategies and efficacy indicators for OM. In addition to strategies such as basic oral care, anti-inflammatory and analgesic agents, anti-infective agents, pro-healing agents, and photobiotherapy recommended in previous guidelines, we also emphasize the role of traditional Chinese medicine in OM prevention and treatment. This expert consensus aims to provide references and guidance for dental physicians and oncologists in formulating strategies for OM prevention, diagnosis, and treatment, standardizing clinical practice, reducing OM occurrence, promoting healing, and improving the quality of life of patients.
Similar content being viewed by others
Introduction
Radiochemotherapy-induced oral mucositis (OM) refers to mucosal lesions characterized by congestion, erosion, ulcers and atrophy that occur in the oral cavity of patients treated with head and neck radiotherapy (RT), chemotherapy (CT), or targeted drugs. Epidemiological data show that the incidence of OM in patients undergoing radiochemotherapy for head and neck tumors ranges from 59.4% to 100%.1 The incidence of OM varies considerably in patients undergoing CT and is related to the type and dose of chemotherapeutic agents. For example, the incidence of OM in patients undergoing high-dose CT prior to hematopoietic stem cell transplantation (HSCT) can be 70% or more.1 OM can lead to pain, difficulty eating, dry mouth, and taste disorders, which seriously affect the survival of patients and even force the interruption of tumor treatment.1,2,3 Therefore, effective prevention and intervention in OM development are of great clinical importance. In recent years, oral mucositis caused by molecular targeted therapy, immunotherapy and other biological therapy strategies has gradually increased, and the clinical treatment principles and significance of OM are the same. Thus, it is also included in tumor therapy-related oral mucositis.
The first evidence-based clinical practice guidelines related to OM were published in 2004 by the Multinational Association of Supportive Care in Cancer and the International Society of Oral Oncology (MASCC/ISOO).4,5,6,7 Subsequently, relevant guidelines were published by the European Society for Medical Oncology (ESMO) and the Cochrane Collaboration (UK).8,9 The China Society for Radiation Oncology (CSTRO) in 2019 and the Antineoplastic Agents Safety Management Committee of the Chinese Society of Clinical Oncology (CSCO) in 2021 took the lead in publishing relevant expert consensuses.10,11 However, to date, there has been a lack of in-depth and comprehensive strategies for the prevention, diagnosis, and treatment of this disease from the perspective of oral specialty practices, a sufficient understanding of the important role of oral health status in the prevention and treatment of OM, and guidance for nondental specialists and caregivers. Therefore, based on of evidence-based medicine as well as existing clinical practice guidelines and expert consensus worldwide, this expert consensus is formulated from the point of view of stomatology. It combines experts and scholars from stomatology, oncology, radiology and other disciplines to develop an expert consensus on the clinical diagnosis and treatment of OM that is clinically instructive and consistent with the national conditions of China. Consensus among experts is reached using the Delphi method. This consensus adds new content, including auxiliary examination, diagnosis and differential diagnosis, and efficacy indicators. New interventions, such as topical glucocorticoids,12,13 recombinant bovine basic fibroblast growth factor (rb-bFGF),14,15,16 and elemental diets,17,18 are recommended in this consensus. Some traditional Chinese medicines have also shown good efficacy in the prevention and treatment of OM, such as Shuanghua Baihe tablets19,20 and Kangfuxin liquid21,22,23; we also discuss and recommend these new intervention strategies.
Epidemiological Characteristics And Pathogenesis
Risk factors
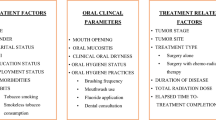
The risk factors for OM can be categorized into patient-related factors and treatment-related factors (Fig. 1).
Patient-related factors
These factors include previous onset of OM after oncologic treatment, poor oral hygiene, decreased salivary secretion function, poor oral habits, smoking, and poorly controlled underlying systemic disease. The correlation between patient age/sex and the occurrence of OM is controversial.1
Treatment-related factors
RT mainly includes the following: transillumination site, irradiation dose, irradiation volume, fractionated RT and radiation types.10,11,24,25,26,27,28,29,30,31,32,33,34 For example, more than 90% of patients treated with systemic RT experience OM, and at least 33% of patients undergoing local RT for head and neck cancer (HNC) developed oral mucositis.27,28,29 In addition, the mode of radiation also affects OM occurrence. The lowest incidence of OM is 16.9% in patients treated with intensity-modulated radiotherapy (IMRT).30,31,32 The incidence of OM with proton beam radiotherapy (PBRT) is comparable to that of conventional RT for the head and neck region, which is 33.4%.32 However, the incidence of OM in patients undergoing hyperfractionated RT and accelerated fractionation treatment remains high, at approximately 94% and 71.4%–93.1%, respectively.28,29,33 It is generally believed that when the oral cavity is exposed to high doses of RT ((58.8 ± 2.2) Gy), the incidence of severe mucositis of grade 3 or above (mucosal patchy ulcers with significant bleeding and severe pain, affecting eating, and even facing life-threatening risks requiring urgent treatment) can reach 45.8%.34
CT mainly includes categories, dosages, regimens and other factors;11,24 concurrent RT; high-dose CT or RT administered prior to HSCT; and targeted therapy drugs in combination with radiochemotherapy.11,35 The incidence of OM in individuals receiving traditional TAC (docetaxel, adriamycin, cyclophosphamide) regimens can reach 60%, whereas dose-intensive regimens reduce the incidence to 30%.24 The incidence of severe mucositis at grade 3 or higher in chemoradiotherapy regimens is as high as 45%; however, this can be reduced to 26% by using IMRT.36 The incidence of OM varies when targeted therapy is employed. Specifically, mammalian target of rapamycin (mTOR) and human epidermal growth factor receptor (HER) inhibitors, such as everolimus and afatinib, are associated with occurrence rates ranging from 24%–64% and 25%–72.1%, respectively.35,37,38 The morbidity rate of epidermal growth factor receptor (EGFR) inhibitors varies significantly, with dacomitinib reaching values of 37%–41%.39,40 Cetuximab potentially reaches a maximum of 37%,41 whereas erlotinib has the lowest morbidity, which is typically controlled within 1%.42 In comparison, angiogenesis inhibitors, anaplastic lymphoma kinase (ALK) inhibitors, and tyrosine kinase inhibitors all maintain lower OM rates of approximately 29% and rates of severe mucositis of grade 3 or higher of 4%.43,44,45 The incidence of OM with bevacizumab is only 4%, and there have been no reported cases of severe mucositis of grade 3 or higher.46
Considering patients’ own factors and treatment-related factors, clinicians can assess the risk of developing OM before tumor treatment based on 3 risk classes: high, medium and low (Fig. 1). Depending on different risk scales, various prevention and treatment strategies can be employed.
Pathology and pathogenesis
OM can be divided into acute and chronic forms. The acute phase manifests as tissue edema, capillary dilatation, necrosis and rupture of epithelial cells, and exudation of fibrin and blood cells. Sonis et al. summarized the developmental pathological process of mucositis based on the following five stages: the initiation stage, initial damage response stage, signal amplification stage, ulceration stage, and repair stage.47
Initiation stage
Mucosal tissues quickly enter the initial phase after exposure to RT or CT. At this point, DNA damage is commonly observed in epithelial basal cells and submucosal cells, and DNA double-strand breaks are noted in endothelial cells.48 Non-DNA damage occurs simultaneously and often manifests as a dramatic increase in the levels of reactive oxygen species (ROS) associated with cellular damage, leading to oxidative stress within cells.48,49 Lymphocyte activation is mediated by the innate immune response of an organism. The initiation phase is the basis for mucositis development, and effective interventions targeting this phase can prevent further mucosal tissue damage.
Initial damage response stage
Elevated ROS levels activate transcription factors such as P53, Wnt and NF-κB50,51 and induce changes in the expression of inflammatory mediators, such as tumor necrosis factor (TNF-α), interleukins (ILs), cyclo-oxygenase 2 (COX-2), and cell adhesion molecule (CAMs).52,53 In addition, c-Jun and c-Jun N-terminal kinase (JNK) expression is upregulated,54 activating other transcription factors, such as nuclear factor erythroid 2-related factor 2 (NRF2). The accumulation of TNF-α, IL-6 and IL-1β in the mucosal epithelium and connective tissues leads to increased oxidative stress, basal cell death, and tissue destruction. The Toll-like receptor (TLR) signaling pathway and various kinase pathways, such as the mitogen-activated protein kinase (MAPK) pathway, play a role in this process.55 Broken DNA strands caused by radiochemotherapy can directly activate the intracellular ceramide pathway, leading to apoptosis as well as increased permeability of cell membranes.56 Moreover, elevated ROS levels activate sphingomyelinase or ceramide synthetase, which hydrolyses the cell membrane lipid sphingomyelin, leading to increased intracellular ceramide levels. Fibroblasts secrete matrix metalloproteinase (MMP) family proteins, such as MMP1 and MMP3, which disrupt the epithelial basement membrane, hydrolyze the subepithelial collagenous matrix, and promote the spread of inflammatory factors to deeper layers of mucosal tissue.
Signal amplification stage
The persistent damage to mucosal tissue caused by radiochemotherapy manifests as positive feedback regulation and creates a vicious cycle of inflammatory factors affecting proinflammatory signaling pathways. This prompts entry into the signal amplification phase of OM. For example, exposure to cytotoxic rays or drugs leads to NF-κB signaling pathway activation. The expression of the proinflammatory cytokines TNF-α and IL-1β increases, and these factors are released extracellularly, triggering NF-κB pathway activation in adjacent cells. This results in the upregulation of MAPK, COX2, and tyrosine kinase expression. TNF-α also contributes to the upregulation of ceramides through sphingomyelinase activation, leading to cell apoptosis. Postapoptotic debris and pathogenic microorganisms infiltrating loose intercellular adhesion channels activate the immune system and further activate the NF-κB pathway.57,58 Patients at this pathological stage have not yet exhibited significant clinical signs; however, in severe cases, mucosal erythema may be observed.
Ulceration stage
Continuous secretion of inflammatory factors leads to severe mucosal tissue damage, loss of epithelial integrity, and ulcer formation. Owing to the presence of exposed nerve endings, patients experience significant pain, which results in a decreased ability for self-oral hygiene management. Many pathogenic microorganisms colonize the ulcer surface, and their toxic factors, such as cell wall components, penetrate into deeper submucosal tissues through the ulcer surface. This prompts lymphocytes, macrophages, and neutrophils to infiltrate and aggregate in this area, where they continuously secrete large amounts of proinflammatory and proapoptotic factors, leading to more extensive cell apoptosis and tissue disintegration.59 In severe cases, it can lead to systemic infection.
Repair stage
At the end of radiochemotherapy, damaged mucosal tissue has the potential to promote wound healing and self-repair. Epithelial cell proliferation and migration led by the submucosal matrix and mesenchymal-related signals repair mucosal epithelium continuity, maintain redox balance, and remodel the oral microbial ecology. This process is related to the regimen, use of concurrent CT, dosage and duration of radiochemotherapy. However, the genome of the newly produced mucosal epithelium differs from that of the original mucosal epithelium, perhaps resulting in a lower tissue tolerance threshold to radiochemotherapy.
Clinical Manifestations
When patients with radiotherapy-induced oral mucositis (RIOM) receive a cumulative dose of 10 Gy, they often experience a burning sensation and eating irritation. When the cumulative dose reaches 30 Gy, they may suffer from severe pain, xerostomia, halitosis, and difficulty eating. In severe cases, they may endure dysgeusia and restricted opening of the mouth. A few patients may experience alopecia, pigmentation and fibrosis in the irradiated field. In the acute stage, congestion, edema, erosion, ulceration, and pseudomembrane formation may occur in the oral mucosa of patients with RIOM, and the lesions gradually subside and heal when RT ends (Fig. 2). In severe cases, these signs and symptoms may last up to 2 or 5–7 weeks after RT ends.1 Chronic RIOM may also develop up to two years after the completion of radiotherapy and is characterized by secondary damage resulting from extensive atrophy of the salivary glands. Primary clinical manifestations include xerostomia and dysgeusia, with cardinal physical signs presenting as widespread atrophy, thinning, and congestion of the oral mucosa. Chronic RIOM is frequently complicated by concurrent Candida infections. Patients typically exhibit dermatological alterations in irradiated skin areas, including dryness, desquamation, hyperpigmentation, and subcutaneous fibrosis.
Radiotherapy-induced oral mucositis. Female, 3 months after surgery and radiotherapy for the breast tumor. Painful oral erosions appeared during radiotherapy and persisted for a long time, accompanied by dry mouth. Large areas of congestion and scattered erosions were observed in the cheeks, with fine white lines around the cheeks. White lines with a few scales were observed on the lips. a Left cheek; b upper right cheek; c lower right cheek; d lips
Chemotherapy-induced oral mucositis (CIOM) usually begins with a sense of local burning or stinging in the mucosa approximately 4 to 5 days after the initiation of CT, with pain symptoms worsening after 7 to 10 days and culminating approximately 2 weeks later.11 The signs are similar to those in the acute phase of RIOM, which mainly manifests as erosion, ulceration, pseudomembranes, or crust (Fig. 3). If the lesion is not infected, it normally resolves within three weeks following treatment. When accompanied by a secondary infection, the oral mucosa shows clinical symptoms of diseases such as Candida albicans infection and herpes simplex virus infection.
Chemotherapy-induced oral mucositis. Male, postoperative liver cancer and were taking chemotherapy drugs for 9 months, large erosions and ulcers were observed on both the cheeks and the back of the tongue, and thicker blood crusts were observed on the lower lip. a Left cheek; b right cheek; c dorsum of the tongue; d lips
The clinical manifestations of OM induced by molecular targeted drugs are related to the drug category. For example, mucosal ulceration occurs 10 days after mTOR inhibitor dosing but generally resolves within 1 week.35,60 EGFR inhibitors are associated with the development of ulcers 2–3 weeks after dosing, and some patients may experience pain, dysphagia, and dysgeusia.35,61 Vascular endothelial growth factor (VEGF) inhibitors cause diffuse oral mucosal sensory abnormalities, mucosal congestion, or ulceration within the first week of dosing.62,63 In the context of PD-1/PD-L1 immune checkpoint inhibitors such as navulizumab, OM typically occurs 3 months after the initiation of treatment and is characterized by a mossy lesion with symmetrically distributed white reticulation, which may be accompanied by mild erythema and/or ulceration.64,65,66
OM is graded according to the signs and symptoms of patients. Currently, the commonly used grading criteria for OM include the World Health Organization (WHO) Oral Toxicity Scale, the Radiation Therapy Oncology Group (RTOG) scoring criteria for acute RIOM, and the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI-CTCAE) (Fig. 4). The WHO grading standard focuses more on the assessment of eating conditions, whereas the RTOG and NCI-CTCAE criteria emphasize the evaluation of oral pathological and physiological conditions. RTOG classifies toxicity into acute (within 1–3 months) and late (after 3 months) phases, which are generally used for patients undergoing RT alone. NCI-CTCAE is generally used for patients undergoing comprehensive treatments such as concurrent chemoradiotherapy. Although only the WHO and RTOG criteria have been formally adopted through expert voting, the NCI-CTCAE criteria remain included in this consensus according to the recommendations of oncology and radiology experts owing to their critical importance in clinical application. These three criteria are collectively presented to serve as a comprehensive reference framework for guiding clinical practice and research implementation. To date, no evidence is available to suggest which grading criteria are superior. Multiple grading standards are recommended for comprehensive assessment.
Diagnosis and Differential Diagnosis
The diagnostic criteria for OM include a history of radiochemotherapy, a history of targeted drug therapy or radiation exposure, an association between the onset timing of oral mucosal damage and radiochemotherapy regimens, and typical clinical signs and symptoms of oral mucosal damage. Differential diagnosis is required mainly for acute episodes of erosive ulcerative lesions, especially those that may appear widely distributed, such as herpetiform recurrent aphthous ulcers, primary herpetic gingivostomatitis, allergic stomatitis, erythema multiforme, oral lichen planus (erosive type), and coccigenic stomatitis. The early erythematous phase of OM should be differentiated from oral candidiasis.1,67,68
Notably, patients receiving RT often experience a decline in immune function. When OM presents with erosions, ulcers, and other lesions, it is often associated with microbial infections. If necessary, a complete blood count and cultures for bacteria, fungi, and other pathogens can be performed to identify the type of infection and administer targeted medication, thereby improving clinical efficacy.1,11 However, owing to differences in economic levels and medical technical levels among institutions in different regions, performing bacterial/fungal cultures and antibiotic susceptibility tests as necessary prerequisites for the use of antimicrobial drugs to treat OM would significantly increase the cost of medical treatment and the complexity of clinical diagnosis and treatment for patients. Therefore, for those who experience poor anti-infective effects according to empirical routines, antibiotic susceptibility tests should be performed in a timely manner to guide the clinical use of drugs. For example, in the case of IMRT for nasopharyngeal carcinoma, in which the incidence of RIOM is 100% and accompanied infections are common, performing a throat swab culture for bacteria can guide the selection of antibiotics, and the infection control effect is superior to that of empirical medication.69 The necessity of viral testing is controversial, and it is not the first choice for auxiliary diagnostic methods.
Several emerging technologies, including molecular diagnostics and artificial intelligence, play significant roles in the diagnosis and prediction of OM. For example, various inflammatory biomarkers, such as TNF-α, IL-1β, and IL-6, are significantly elevated in the saliva of patients undergoing chemoradiotherapy and are positively correlated with OM severity. These biomarkers can serve as auxiliary diagnostic tools or facilitate early identification of high-risk patients.70 Furthermore, machine learning methods have demonstrated effectiveness in predicting OM occurrence among patients receiving radiotherapy,71,72 chemotherapy73 and hematopoietic stem cell transplantation.74
Disease Management Measures
Disease prevention plan
Effective prevention measures can reduce the incidence and severity of OM, delay lesion onset, alleviate pain, and significantly improve patients’ quality of life. Clinicians can assess the risk level of patients about to undergo radiochemotherapy on the basis of the OM risk assessment (Fig. 1), categorize patients into high-risk, medium-risk, and low-risk groups, and then formulate and implement different preventive measures accordingly.
Oral health promotion and management
Patients who were well versed in oral health care and understood the adverse effects of RT and CT had a lower incidence, severity, and duration of OM following their initial treatment. This finding could be attributed to patients’ conscious efforts to keep their oral mucosa moist, maintain oral health and hygiene, and effectively control their oral flora.75,76 When OM progresses to a severe stage, patients may encounter a range of biopsychosocial issues, including difficulty eating, nutritional imbalances, social barriers, and painful discomfort, all of which contribute to a loss in an individual’s quality of life. Good oral hygiene education and patient management can significantly reduce the adverse effects and complications of OM, such as reduced salivation, dysphagia, and dysgeusia, and improve quality of life scores (QoLSs).77 As OM causes symptoms such as pain, bleeding and limited mouth opening, it can lead to a reduction in patients’ ability to take care of their own oral health. Oral health education enables patients to be aware of the importance of oral health and hygiene care in relieving OM symptoms and improving patients’ self-oral management ability and adherence.78 The content of oral health education may include nutritional advice for preventing OM, suggestions for preventing and improving dry mouth, advice on issues such as taste and smell changes, techniques for using toothbrushes and dental floss, and daily self-assessment of their oral mucosa.
Patients who actively and continuously manage their oral health before, during, and after radiochemotherapy and control oral pathogen infections can effectively delay the onset of OM and prevent OM progression to severe stages. Kartin et al. proposed comprehensive self-oral care measures and nutritional plans for patients undergoing radiochemotherapy, which can effectively reduce the severity of OM pain, improve patient malnutrition, and enhance their QoLS.79 Brushing teeth, rinsing the mouth, using dental floss and interdental brushes, keeping the oral mucosa moist, and maintaining a low temperature are all measures used to strengthen self-oral management.80
For patients who are about to undergo radiochemotherapy, the timing of implementing self-oral management is equally important. Basic oral management measures, including tooth brushing and water rinsing, should begin one week before the start of radiochemotherapy. This can effectively delay OM onset in nasopharyngeal cancer patients undergoing radiochemotherapy, reduce its severity, and result in higher oral health assessment scores. Implementing oral health management measures only the day before starting radiochemotherapy is unlikely to have a significant effect on alleviating oral mucositis.81 The frequency of daily oral care (such as the number of rinses) and the selection of products/medications for patients should be adjusted to the various OM grading stages.75,79
Before patients undergo radiochemotherapy, a comprehensive and professional oral health examination and assessment by dentists to preemptively identify and eliminate potential risk factors for OM could facilitate the smooth progression of radiochemotherapy and effectively control hematogenous infections.82 OM risk can be effectively reduced by weekly professional oral examinations and treatments, including scaling and brushing, nutritional intake counseling, and lifestyle guidance, in breast cancer patients undergoing CT.83 A randomized controlled phase III trial revealed that regular professional oral care, such as teeth cleaning, reduces the incidence and severity of OM in breast cancer patients treated with everolimus and exemestane while also improving patients’ tolerance and compliance in managing CT-induced complications.84 Professional oral assessment and treatment should include the following six aspects:85,86 (1) comprehensive assessment of OM susceptibility factors (oral hygiene, caries, metal restorative materials, and dentures); (2) controlling the susceptibility factors that can cause mucosal or periodontal infections and prevent the development of localized infections and systemic spread of infection (periodontal scaling, removal of residual roots/crowns/affected teeth, conversion of metal to nonmetal fillings, removal of poorly restored restorations, maintenance of oral hygiene); (3) reducing oral discomfort and pain; (4) maintaining basic oral function to support nutritional intake and speech function; (5) managing oral complications from RT and drug-targeted therapies; and (6) enhancing individual quality of life.
Topical drug prevention
Despite available evidence that patients receiving professional oral management practices can help prevent OM, approximately 75% of patients still present with adverse signs on the oral mucosa following RT.84 For low- and median-risk patients, a combination of oral specialty prophylaxis, such as anti-inflammatory and analgesic agents, healing promotion and coinfection control, is needed.
Anti-infective drugs
Chlorhexidine rinses have been shown to play a significant role in antimicrobial therapy for periodontal tissues, as these drugs inhibit bacterial, fungal and viral colonization. As a risk factor for OM, intraoral microbial colonization of pathogenic organisms in combination with cytotoxic therapy plays a significant role in contributing to OM development. Meta-analysis has shown that local application of chlorhexidine rinses effectively prevent CIOM.87,88 However, chlorhexidine does not have significant preventive effects on RIOM. Patients in the CT group receiving 0.12% chlorhexidine gargle solution three times a day at 15 mL/dose presented a decreased incidence, faster remission, and reduced severity of OM, whereas those in the RT group had no significant preventive effect. Intraoral microflora colonization was reduced in both groups.89 Two additional randomized controlled trials further validated that local application of chlorhexidine does not effectively prevent RIOM90 and may even cause more severe OM, as well as more noticeable adverse effects (taste alternation and tooth staining).91 Therefore, the local application of chlorhexidine rinses is only recommended for the prevention or mitigation of CIOM, not RIOM.
Sodium bicarbonate removes detached cellular debris from the surface of the oral mucosa, increases the pH, and inhibits acidophilic bacteria. Sodium bicarbonate mouthwash has prophylactic effects against OM and postpones the onset of CIOM in patients undergoing CT for acute leukemia.92 However, it is less effective than oral rinsing with benzydamine in preventing RIOM.93 It is recommended that 10 g of sodium bicarbonate powder be dissolved in 1 L of sterile water or physiological saline and used at 15 mL/2 min/4 times/day, starting from the day before RT and continuing for two weeks after treatment is completed.
Pro-healing drugs
Granulocyte-macrophage colony-stimulating factor (GM-CSF) promotes the aggregation of lymphocytes and myeloid cells, such as macrophages and Langerhans cells, inducing local tissue inflammatory responses and stimulating macrophages to secrete pro-healing molecules. Additionally, GM-CSF stimulates the growth of keratinocytes and fibroblasts, promoting ulcer surface repair and wound healing.94 The use of GM-CSF for oral administration or gargling has a definite effect on preventing RIOM, effectively delaying the progression of RIOM to severe stages.95,96,97 A GM-CSF oral rinse (150 g GM-CSF in 100 mL of 0.9% NaCl solution) was prepared and gargled 4 times a day from the pretreatment date (25 mL per wash >3 min) and swallowed in small amounts after gargling. However, the effectiveness of subcutaneous GM-CSF injections in preventing RIOM is controversial.98,99,100,101,102
Topical application of Kangfuxin liquid significantly reduces the incidence and severity of RIOM.22 Kangfuxin liquid can increase the function and quantity of neutrophils in wounds while promoting the secretion and deposition of the extracellular matrix, expediting the healing process. Starting from the day of RT, 10 mL Kangfuxin liquid is gargled for 3 minutes, and the mixture is then swallowed slowly, three times a day, until the end of RT. When needed, Kangfuxin liquid ice cubes can be used for buccal administration.23
Anti-inflammatory and analgesic drugs
As nonsteroidal anti-inflammatory drugs, benzydamine inhibits the secretion of TNF-α and IL-1 from local mucosal tissues, acting as anti-inflammatory, antibacterial and local analgesic agents.103,104 For head and neck squamous cell carcinoma (HNSCC) patients receiving moderate doses of RT (a total radiation dose of up to 50 Gy, with a daily radiation dose less than 2.2 Gy), the use of benzydamine oral rinses could reduce the incidence of erythema and ulcers by approximately 30%, relieve patients’ pain, and prevent RIOM effectively and safely.105,106 For patients receiving concurrent chemoradiotherapy, a benzydamine oral rinse is also useful for preventing OM and controlling oral mucosal infections.93,107,108 The recommended usage is as follows. For patients receiving moderate radiation doses (<50 Gy) or CT, a 0.15% benzydamine oral rinse (15 mL/2 min/dose) should be used 4-8 times per day starting on the day of treatment. The oral rinse can be diluted proportionally if the solution is too thick.
Rebamipide inhibits the production of reactive oxygen species by inflammatory cells and scavenges hydroxyl radicals.109,110 The use of oral rinses with rebamipide may prolong the onset and reduce the severity of OM in RT patients.111 The recommended concentration for patients receiving radiation for HNC is 4%.112 It can be started three days before radiochemotherapy, with a dosage of 5 mL for 30 s per rinse, six times a day. The rinse should be continued for three months.
Systemic drug prevention
For high-risk patients with tumors prone to OM, in addition to necessary oral hygiene management and local treatment, systemic pro-healing and anti-inflammatory agents are recommended to prevent the occurrence of moderate or severe OM.
Intravenous keratinocyte growth factor-1 (KGF-1) is effective in preventing OM. However, its outpatient application is limited, and it is mostly used in hospitalized patients. Intravenous injection of KGF-1 can reduce the incidence of moderate to severe OM in patients receiving head and neck radiochemotherapy, prevent the occurrence of OM, and delay the onset of severe OM.113,114 For acute leukemia patients who require CT, KGF-1 can also play a role in preventing the exacerbation of OM.115 Currently, a consensus on the dosage and frequency of KGF-1 usage is not available. However, a common dose used in clinical trials is 360 μg/kg, and the number of intravenous injections is often six. It can be administered once daily from 3 days before to 3 days after radiochemotherapy initiation or once a week starting one week before radiochemotherapy and continuing weekly thereafter.9
Glutamine can alleviate the oxidative damage caused by ionizing radiation by inhibiting the secretion of proinflammatory factors. It activates collagen synthesis, provides the necessary energy for cell proliferation, and promotes mucosal wound healing.116 For patients with HNC undergoing RT, oral glutamine (10 g/1 000 mL, taken 2 h before RT) can effectively prevent and remedy RIOM, significantly alleviate the severity of OM, reduce opioid analgesic use and decrease the likelihood of nasogastric tube feeding and treatment interruptions.117,118 In patients with solid tumors during CT, treatment with an oral glutamine suspension has also been shown to be effective in relieving moderate to severe OM and reducing patient pain (2 g/M2, twice a day).119,120
Pilocarpine has effects similar to those of acetylcholine, stimulating the secretion of saliva and sweat and preventing xerostomia caused by RIOM. Studies have shown that oral administration of pilocarpine significantly reduces the incidence of severe RIOM (grade ≥3) in HNC patients.13,121 However, pilocarpine does not have significant effects on patients with oral squamous cell carcinoma receiving concurrent chemoradiotherapy.13 Pilocarpine can significantly reduce the severity of OM in patients with solid tumors and acute leukemia undergoing chemotherapy,122 but it does not provide benefits for patients undergoing pretransplant conditioning for HSCT.123 It can be administered orally at 5 mg/dose 3 times/day prior to treatment and reduced to 2.5 mg/dose 4 times/day if the patient sweats significantly.
As traditional Chinese medicines, Shuanghua Baihe tablets contain berberine as a Coptis Rhizoma component and have been proven to have antibacterial, antifungal, antioxidant, and anti-inflammatory properties. For patients undergoing RT in the head and neck region, Shuanghua Baihe tablets can be used to reduce the incidence of OM, alleviate the degree of pain, and shorten the healing time.19,20 The tablets can be taken orally from the first day of treatment (4 tablets/dose, 3 times/day).
Photobiotherapy prevention
Low-level laser therapy (LLLT) can directly act on cellular mitochondria, maintain cellular homeostasis, promote cell proliferation and collagen synthesis, increase cellular metabolism, accelerate wound healing and tissue repair, induce angiogenesis, enhance leucocyte activity, reduce damage caused by radiochemotherapy to tissues, and have analgesic effects.124 For pediatric patients undergoing HSCT, high-dose radiochemotherapy or radiochemotherapy for head and neck tumors, a low-level laser (620–750 nm) is beneficial for preventing and controlling severe OM (grade ≥3).125,126,127 For patients with head and neck tumors undergoing chemoradiotherapy, LLLT has also been proposed to have a role in preventing OM.128 Owing to the lack of well-designed and large-scale clinical trials, the parameters for LLLT mostly depend on the experience of clinical physicians. For patients with HNC undergoing chemoradiotherapy, the parameters for preventing OM in multiple clinical trials of LLLT include a wavelength ranging from 632.8 to 660 nm, an energy density ranging from 2.5 to 4 J/cm2, and power ranging from 10 to 100 mW.129 Notably, individual studies reported that LTTT was not effective in preventing radiochemotherapy-induced OM,130 but most studies support its effectiveness. In addition, some experimental studies suggest that photobiomodulation has a carcinogenic effect,131,132,133 but current clinical evidence shows that photobiomodulation has good safety.134,135 Nonetheless, clinicians should inform patients of the potential risks of photobiomodulation therapy before its use.
Additionally, the use of cryotherapy136 and standard oral care137,138 in conjunction with LLLT are advisable for OM prevention.
Others
Saline solution can serve as a mild mouthwash, helping patients maintain oral health and hygiene, as well as improving their comfort level.139 It has been suggested that topical application of sucralfate mouthwash or oral administration of sucralfate in patients can be effective in preventing OM;140,141,142,143 however, some studies report the opposite conclusion.144,145 Cryotherapy refers to chewing ice chips before and after CT to reduce the temperature of the oral mucosa. This can constrict mucosal blood vessels and decrease blood flow, thereby reducing the effects of CT drugs on the oral mucosa and preventing OM occurrence.146,147,148,149,150 However, although cryotherapy has the advantages of low cost and ease of implementation, its preventative efficacy is limited by the drug’s half-life, and it cannot replace the important role of patient oral care education and monitoring in the prevention of OM. Additionally, patients with nasopharyngeal carcinoma who undergo RT can wear personalized oral stents to reduce the radiation dose received by the oral mucosa; this can help to preserve healthy oral mucosa and potentially avoid RIOM.151
Disease control plan
Oral health management
On the basis of sufficient evidence available,83,84,152,153 professional oral management by dental specialists during RT for tumors is conducive to monitoring the health condition of the oral mucosa, relieving symptoms and promoting healing. Specific measures include (1) conducting a comprehensive oral examination weekly during the treatment period to closely monitor oral conditions, with particular attention given to the second week after CT, which is a high-incidence period for OM; (2) taking appropriate management measures based on oral assessment, such as periodontal scaling, crown surface polishing, tongue microbiome control, and the use of antimicrobial mouthwashes or corticosteroid ointments; and (3) instructing and checking the patient’s tooth brushing method by a doctor or nurse, advising patients to brush their teeth gently once in the morning and once before bed, brushing gently and avoiding abrasing soft tissues. In addition, if patients have a tendency for severe gum or mucosal bleeding, using cotton swabs to remove deposits from the surface of teeth and mucosa.
For special populations such as pediatric patients, owing to their weaker ability to control their own oral hygiene, it is more important to emphasize the role of guardians in helping children achieve self-oral hygiene management. Additionally, to closely monitor any oral complications that arise in children receiving CT/RT and facilitate antitumor treatment, a variety of oral management strategies should be used.154,155 Specific measures include (1) long-term professional oral management by dental specialists; (2) oral health education for patients and their guardians; (3) daily assessment of oral hygiene in hospitalized patients; and (4) the use of various oral management measures, such as compound mouthwashes (antimicrobial + analgesic + glucocorticoid + vitamin B + fluoride-containing), in conjunction with photobiomodulation therapy.
Medication
Anti-inflammatory drugs, analgesics and antidepressants
Burning, irritation, and pain are common clinical symptoms in patients with OM, resulting in eating, swallowing, and speech disorders, as well as a lower quality of life. Topical applications of doxepin, lidocaine, and tetracaine can effectively alleviate pain symptoms associated with OM.
Doxepin is a tricyclic antidepressant that works by blocking sodium ion channels156 and preventing stimulus conduction in cutaneous and mucosal nociceptors. It has sedative and analgesic effects when used topically. Several studies have shown that using doxepin oral rinses can provide rapid analgesia when radiochemotherapy patients experience mucosal pain, and the analgesic effect can last for more than 2 hours.157,158,159,160 The drug may have side effects such as taste disturbances and drowsiness after use, and patients can use it as a sleep aid. Doxepin oral rinse (5 mg/mL) can be used for 1 min; this should be followed by coughing and spitting it out 3–6 times/day.
Lidocaine can also be used to alleviate OM-related pain, which is characterized by rapid onset. In contrast, the analgesic effect lasts for a shorter duration than doxepin (approximately 30 min to 1 h), which may lead to an increased frequency of drug administration.157,161 Patients can rinse with a lidocaine solution and then spit it out or apply viscous lidocaine + 1% cocaine directly to painful mucosal areas.162
A clinical trial proposed that the use of 1.5% tetracaine gel can safely and effectively reduce RIOM-related pain in a significant proportion of HNC patients.163 However, larger randomized controlled trials are needed to investigate the effects of tetracaine compared with those of other topical analgesics.
Topical glucocorticoids are often applied clinically to relieve RIOM symptoms. It has been reported that topical dexamethasone ointment reduces the incidence of severe OM in patients treated with RT for OSCC; however, no substantial efficacy has been observed in patients treated with concurrent chemoradiotherapy.13 Triamcinolone acetonide mucoadhesive films have also been shown to be effective in reducing pain in RIOM patients.12
When stimulated by radiochemotherapy, mucosal tissues release large amounts of inflammatory factors, free radicals, and oxidative stress, leading to rapid destruction of epithelial tissue. A oral rinse containing 0.2% vitamin E (antioxidant), 0.1% triamcinolone acetonide (anti-inflammatory agent) and 0.2% hyaluronic acid (topical reductant to reduce stimulation of reactive oxygen on mucosal tissues) can achieve good therapeutic effects on OM.164 The usage was gargling 2 mL/min, 3 times/day, and not eating or drinking for 15 min afterward.
Protective oral gel is a bioadhesive material that can adhere to mucosal ulcers, quickly forming a protective barrier that provides wound protection and analgesia. Several clinical trials have demonstrated that protective oral gel can adhere to red, swollen and ulcerated oral mucosa of head and neck CT/HSCT patients and provide analgesic effects for a long period of time (6–8 h), effectively relieving regional pain.165,166,167
Antimicrobials
Mucosal tissues of patients undergoing radiochemotherapy are prone to damage and disintegration, providing channels for oral bacteria and fungi to invade deeper tissues. Patients often suffer from pain and other antitumor therapy complications, resulting in poor self-cleaning. This can cause residual food debris in the oral cavity, providing sustenance for pathogenic microorganisms. The cell wall and other toxic substances can cause more severe cellular phagocytosis and tissue inflammatory responses. Using chlorhexidine and sodium bicarbonate oral rinses, miconazole mucoadhesive buccal tablets to control the number and activity of bacteria and fungi in the oral cavity can be effective in relieving OM symptoms.
Studies have shown that 0.12% or 0.2% chlorhexidine mouthwash can reduce the duration and severity of OM in patients undergoing chemotherapy.89,168 Five percent sodium bicarbonate mouthwash can effectively treat and alleviate OM severity, accelerate lesion healing, and subsequently improve the QoL of cancer patients during CT.169,170 Miconazole has strong inhibitory activity against most strains of Candida, especially fluconazole-resistant strains.171 Miconazole mucoadhesive buccal tablets have been used for oropharyngeal candidiasis in HIV patients172 and in patients with HNC undergoing CT.173 It is also an effective alternative to oral amphotericin B suspension in patients undergoing high-dose therapy/autologous stem cell transplantation (HDT/ASCT), reducing complications caused by excessively high levels of antifungal agents in blood.174
Pro-healing drugs
IL-11 promotes peripheral platelet production, stimulates hematopoietic stem cell proliferation, and facilitates ulcer healing. It regulates macrophage function, promotes the secretion of epidermal growth factor, shortens the cell growth cycle, and accelerates tissue repair. IL-11 oral rinses can effectively reduce OM clinical grade, shorten healing tim,175,176 and promote a decrease in serum C-reactive protein levels, alleviating pain.177 The use of an IL-11 oral rinse (1.5 mg/100 mL) after brushing and rinsing is recommended, and 10 mL should be gargled for 10 min per wash, 4 times/day.
Recombinant bovine basic fibroblast growth factor (rb-bFGF) is effective in reducing the healing time of RIOM lesions.16 When used in combination with Kouyanqing granules14 or sodium bicarbonate mouthwash,15 it has a good therapeutic effect on RIOM in patients undergoing RT for HNC. Notably, given the cell growth-promoting effects of rb-bFGF, clinicians should consider its advantages and disadvantages and make comprehensive decisions regarding its use in patients with oral malignant tumors receiving radiochemotherapy.
Kangfuxin liquids and Shuanghua Baihe tablets are potentially effective in both the prevention and treatment of OM. In patients receiving RT in the head and neck region, Kangfuxin liquid has been shown to significantly reduce OM duration and severity.21,22 A randomized controlled trial with a larger sample size also revealed that oral administration of Shuanghua Baihe tablets effectively relieves OM.19,20 The usage is consistent with that previously described.
On the basis of the overwhelming evidence available,117,119,178,179 oral glutamine is effective in prevention and treatment of OM. The use of 10 g/dose oral glutamine suspension 3 times/day for patients receiving RT and 2.5 g/5 mL/dose glutamine suspension 3 times/day for patients with solid tumors receiving CT can effectively reduce moderate to severe OM.
Diet and nutrition
An elemental diet is a chemically refined meal that contains all the easily digestible and absorbable nutrients needed by the body, including amino acids, carbohydrates, vitamins, inorganic salts, trace minerals, and minimal fats. This diet can effectively aid in the early recovery and symptom relief of OM. Oral administration of an elemental diet (containing 79.3% carbohydrates, 17.6% amino acids, 0.6% soybean oil, 2.0% minerals, and 0.5% vitamins) may promote early recovery from OM damage induced by pretreatment of HSCT patients, thereby reducing hospital stays.18 Elemental diets can also effectively improve OM in OSCC patients and increase the radiochemotherapy completion rate.17
Photobiotherapy
LLLT is not only significantly effective in preventing OM but also widely recognized for its ability to relieve OM symptoms. Despite the evident benefits of LLLT, different parameter settings may lead to varying treatment outcomes and poor reproducibility.7,180 A systematic review and meta-analysis181 reported that LLLT (wavelength of 632.8–685 nm, energy density of 1.3–6.2 J/cm2, and power of 5–100 mW) has good clinical outcomes for HNC patients undergoing radiochemotherapy, reducing patient pain and the risk of developing severe OM. Another meta-analysis suggested that182 the most commonly used laser parameters for OM treatment include a wavelength of 660 nm, an energy density of 4 J/cm2, a power density of 1 W/cm2, an energy of 0.16 J, a power of 40 mW, and a spot size of 0.04 cm2.
Currently, most clinical trials of LLLT are conducted using intraoral irradiation. Some scholars have proposed that extraoral LLLT can be equivalent to intraoral transillumination in reducing OM clinical grade and pain levels and accelerating the healing time of mucosal damage.183 In addition, extraoral LLLT has the benefits of shortening the treatment period (approximately 4 min), improving the cooperation of pediatric patients,184 and demonstrating efficacy in the treatment of mucositis of the lips and esophagus.
Others
Topical morphine oral rinse is beneficial in relieving OM pain,185,186,187 but its use has limitations. Moreover, studies have shown that morphine can lead to a reduction in cell migration, which in turn inhibits wound healing.188,189
Honey and propolis are considered natural antioxidants that effectively block the production of free radicals and act as anti-inflammatory and pro-healing agents. Some studies have suggested that honey/propolis may reduce the progression of OM to severe OM and have abirritation and weight maintenance effects for patients,190,191,192 whereas some clinical trials have reported that the therapeutic effect of honey/propolis does not differ from that of placebo group.193,194,195
In summary, clinicians can conduct risk assessments for patients undergoing oncological treatment and choose from the above OM control measures according to the patient’s actual situation based on comprehensive consideration. The clinical guidelines for the prevention and treatment of OM are shown in Fig. 5. If the therapeutic effect is good and recovery is satisfactory, standard treatment and visitation procedures should be followed without the need for additional follow-ups or interventions. If the effect is poor and the patient’s condition worsens, the patient should communicate with an attending physician to consider discontinuing or reducing the intensity of antitumor treatment. After the OM has subsided, the plan should be adjusted to complete subsequent antitumor therapy. Importantly, from the pretreatment phase of radiochemotherapy until one month after anticancer treatment completion, dental specialists should provide continuous oral care for patients and educate patients on self-examination and self-management once every 1–2 weeks. Individuals who have had RT to the head and neck region should be monitored throughout a patient’s life to prevent and treat the occurrence and development of chronic OM over time.
Indicators of efficacy
The effectiveness of OM clinical preventive and therapeutic measures can be assessed in terms of OM lesion severity and degree of oral pain; additionally, assessments can be supplemented by examining the incidence, duration and safety evaluation of severe oral mucositis (grade 3 or higher).106,196,197 The severity of OM lesions can be determined according to clinical grading criteria such as the WHO, RTOG or NCI-CTCAE; the degree of oral pain can be assessed using the visual analog scale (VAS) (0–10), and the pain affect faces scale (PAFS) (0–10). Safety assessments mainly include records of adverse reactions and adverse events.
Conclusion and Expectation
Oral mucositis is one of the most common and severe complications induced by antitumor therapy and can cause redness, swelling and pain in the oral mucosa of patients, leading to speech and eating difficulties and reducing the quality of life of individuals. In severe cases, it can force interruption of radiochemotherapy plans, interfere with antitumor treatment progression, and extend a patient’s hospital stay. Therefore, clinicians should pay attention to patients with tumors and HSCT who are susceptible to the risk of OM, monitor and manage their oral hygiene and health, provide oral health information and education to them and their families to prevent the occurrence of OM, prevent and control coinfections, alleviate pain, control symptom deterioration and promote the healing process through pharmacological and nonpharmacological means.
This consensus acknowledges several inherent limitations. First, the evidence selection process may carry potential biases due to the possible subjectivity in prioritizing certain research. Second, expert opinions, although valuable, might reflect individual specialty backgrounds or clinical experiences that could influence recommendation alignment. Third, significant knowledge gaps persist in specific clinical areas, potentially limiting the generalizability of recommendations across diverse health care systems. Finally, the incorporation of recommendations involving traditional Chinese medicine into international practice currently faces implementation challenges.
Notably, current clinical research on OM intervention strategies predominantly presents a low evidence hierarchy, underscoring the imperative need for future high-quality randomized controlled trials to establish robust guidance for the clinical management of OM. Furthermore, the implementation of preventive and therapeutic measures should be judiciously tailored to regional economic disparities and variations in health care infrastructure across medical institutions. This adaptive approach ensures optimal patient benefit through context-sensitive application of medical interventions while maintaining rigorous adherence to evidence-based practice standards.
References
Elad, S., Yarom, N., Zadik, Y., Kuten-Shorrer, M. & Sonis, S. T. The broadening scope of oral mucositis and oral ulcerative mucosal toxicities of anticancer therapies. Ca. Cancer J. Clin. 72, 57–77 (2022).
Sonis, S. T. Oral mucositis. Anticancer. Drugs 22, 607–612 (2011).
Sonis, S. T. et al. Oral Mucositis and the Clinical and Economic Outcomes of Hematopoietic Stem-Cell Transplantation. J. Clin. Oncol. 19, 2201–2205 (2001).
Rubenstein, E. B. et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer 100, 2026–2046 (2004).
Keefe, D. M. et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer 109, 820–831 (2007).
Lalla, R. V. et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 120, 1453–1461 (2014).
Elad, S. et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126, 4423–4431 (2020).
Peterson, D. E., Bensadoun, R.-J. & Roila, F. Management of oral and gastrointestinal mucositis: ESMO Clinical Practice Guidelines. Ann. Oncol. 22, vi78–vi84 (2011).
Riley, P. et al. Interventions for preventing oral mucositis in patients with cancer receiving treatment: cytokines and growth factors. Cochrane Database Syst. Rev. 11, CD011990 (2017).
Chinese Society of Radiation Oncology of Chinese Medical Association Expert consensus on prevention and control strategy of radiotherapy⁃induced oral mucositis (2019). Chin. J. Radiat. Oncol. 28, 641–647 (2019).
ASMC in CSCO, SCRC. Expert consensus on diagnosis and prevention of acute oral mucositis caused by antitumor therapy. Chin. Clin. Oncol. 26, 449–459 (2021).
Ghalayani, P., Emami, H., Pakravan, F. & Nasr Isfahani, M. Comparison of triamcinolone acetonide mucoadhesive film with licorice mucoadhesive film on radiotherapy-induced oral mucositis: A randomized double-blinded clinical trial. Asia Pac. J. Clin. Oncol. 13, e48–e56 (2017).
Kawashita, Y. et al. Effectiveness of a comprehensive oral management protocol for the prevention of severe oral mucositis in patients receiving radiotherapy with or without chemotherapy for oral cancer: a multicentre, phase II, randomized controlled trial. Int. J. Oral. Maxillofac. Surg. 48, 857–864 (2019).
Yingming, Z., Li, H. & Jiaxia, W. Clinical effect of Kouyanqing granules combined with recombinant bovine basic fibroblast growth factor on acute radiation stomatitis. Chin. Tradit. Pat. Med. 41, 478–480 (2019).
Li, S. H., Jing, N. D. & Lu, H. Curative effect observation of Beifuji for radiation mucositis. Chin. J. Geriatr. Dent. 7, 262–264 (2009).
Li, J. & Kai, Z. Clinical observation of recombinant bovine basic fibroblast growth factor in the prevention and treatment of radiation stomatitis. J. Baotou Med. Coll. 28, 30 (2018).
Harada, K. et al. Efficacy of elemental diet on prevention for chemoradiotherapy-induced oral mucositis in patients with oral squamous cell carcinoma. Support. Care Cancer 24, 953–959 (2016).
Morishita, T. et al. The Efficacy of an Oral Elemental Diet in Patients Undergoing Hematopoietic Stem Cell Transplantation. Intern. Med. 55, 3561–3569 (2016).
Zheng, B. et al. Randomized, Double-Blind, Placebo-Controlled Trial of Shuanghua Baihe Tablets to Prevent Oral Mucositis in Patients With Nasopharyngeal Cancer Undergoing Chemoradiation Therapy. Int. J. Radiat. Oncol. 100, 418–426 (2018).
Jun, C. et al. Clinical Analysis of Effect of Colchester Browns Lily on the Oral Mucositis of Patients with Head and Neck Neoplasm Caused by the Radiology Therapy. Syst. Med. 131–133 https://doi.org/10.19368/j.cnki.2096-1782.2017.17.131. (2017)
Dong, K., Zhang, M., Liang, Y., Zhang, M. & Fei, X. Effects of Kangfuxin Solution on treatment of Severe Oral Mucositis in Patients with after Radiotherapy of Head and Neck Cancer and Its Protection Effect on Salivary Glands. World J. Integr. Tradit. West. Med. 16, 123–127 (2021).
Luo, Y. et al. Effect of Kangfuxin Solution on Chemo/Radiotherapy-Induced Mucositis in Nasopharyngeal Carcinoma Patients: A Multicenter, Prospective Randomized Phase III Clinical Study. Evid. Based Complement. Alternat. Med. 2016, 1–7 (2016).
Cai, Y., Zhu, L. & Lin, J. Effect of Kangfuxin ice cube on prevention and treatment of radioactive oral mucositis of nasopharyngeal carcinoma. J. Nurs. Rehabil. 20, 68–71 (2021).
Jones, J. A. et al. Epidemiology of treatment-associated mucosal injury after treatment with newer regimens for lymphoma, breast, lung, or colorectal cancer. Support. Care Cancer 14, 505–515 (2006).
Sonis, S. T. et al. Perspectives on cancer therapy-induced mucosal injury: Pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100, 1995–2025 (2004).
Haverman, T. M. et al. Oral Complications in Hematopoietic Stem Cell Recipients: The Role of Inflammation. Mediators Inflamm. 2014, 1–18 (2014).
De Sanctis, V. et al. Mucositis in head and neck cancer patients treated with radiotherapy and systemic therapies: Literature review and consensus statements. Crit. Rev. Oncol. Hematol. 100, 147–166 (2016).
Trotti, A. et al. Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systematic literature review. Radiother. Oncol. 66, 253–262 (2003).
Fu, K. K. et al. A radiation therapy oncology group (RTOG) phase III randomized study to compare hyperfractionation and two variants of accelerated fractionation to standard fractionation radiotherapy for head and neck squamous cell carcinomas: first report of RTOG 9003. Int. J. Radiat. Oncol. 48, 7–16 (2000).
Duarte, V. M. et al. Comparison of Dental Health of Patients with Head and Neck Cancer Receiving IMRT vs Conventional Radiation. Otolaryngol. Neck Surg. 150, 81–86 (2014).
Hoffmann, M. et al. Long term results of postoperative Intensity-Modulated Radiation Therapy (IMRT) in the treatment of Squamous Cell Carcinoma (SCC) located in the oropharynx or oral cavity. Radiat. Oncol. 10, 251 (2015).
Romesser, P. B. et al. Proton beam radiation therapy results in significantly reduced toxicity compared with intensity-modulated radiation therapy for head and neck tumors that require ipsilateral radiation. Radiother. Oncol. 118, 286–292 (2016).
Bourhis, J. et al. Phase III Randomized Trial of Very Accelerated Radiation Therapy Compared With Conventional Radiation Therapy in Squamous Cell Head and Neck Cancer: A GORTEC Trial. J. Clin. Oncol. 24, 2873–2878 (2006).
Wang, Z. et al. Protecting the oral mucosa in patients with oral tongue squamous cell carcinoma treated postoperatively with intensity-modulated radiotherapy: A randomized study. Laryngoscope 122, 291–298 (2012).
Vigarios, E., Epstein, J. B. & Sibaud, V. Oral mucosal changes induced by anticancer targeted therapies and immune checkpoint inhibitors. Support. Care Cancer 25, 1713–1739 (2017).
Wardley, A. M. et al. Prospective evaluation of oral mucositis in patients receiving myeloablative conditioning regimens and haemopoietic progenitor rescue. Br. J. Haematol. 110, 292–299 (2000).
Choueiri, T. K. et al. Cabozantinib versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 373, 1814–1823 (2015).
Yao, J. C. et al. Everolimus for Advanced Pancreatic Neuroendocrine Tumors. N. Engl. J. Med. 364, 514–523 (2011).
Ellis, P. M. et al. Dacomitinib compared with placebo in pretreated patients with advanced or metastatic non-small-cell lung cancer (NCIC CTG BR.26): a double-blind, randomised, phase 3 trial. Lancet Oncol. 15, 1379–1388 (2014).
Ramalingam, S. S. et al. Dacomitinib versus erlotinib in patients with advanced-stage, previously treated non-small-cell lung cancer (ARCHER 1009): a randomised, double-blind, phase 3 trial. Lancet Oncol. 15, 1369–1378 (2014).
Lordick, F. et al. Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. Lancet Oncol. 14, 490–499 (2013).
Ciuleanu, T. et al. Efficacy and safety of erlotinib versus chemotherapy in second-line treatment of patients with advanced, non-small-cell lung cancer with poor prognosis (TITAN): a randomised multicentre, open-label, phase 3 study. Lancet Oncol. 13, 300–308 (2012).
O’Brien, S. G. et al. Imatinib Compared with Interferon and Low-Dose Cytarabine for Newly Diagnosed Chronic-Phase Chronic Myeloid Leukemia. N. Engl. J. Med. 348, 994–1004 (2003).
First-Line Crizotinib versus Chemotherapy in ALK -Positive Lung Cancer. N. Engl. J. Med. 373, 1582–1582 (2015).
Hutson, T. E. et al. Randomized Phase III Trial of Temsirolimus Versus Sorafenib As Second-Line Therapy After Sunitinib in Patients With Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 32, 760–767 (2014).
Tournigand, C. et al. Bevacizumab with or without erlotinib as maintenance therapy in patients with metastatic colorectal cancer (GERCOR DREAM; OPTIMOX3): a randomised, open-label, phase 3 trial. Lancet Oncol. 16, 1493–1505 (2015).
Sonis, S. T. The pathobiology of mucositis. Nat. Rev. Cancer 4, 277–284 (2004).
Criswell, T., Leskov, K., Miyamoto, S., Luo, G. & Boothman, D. A. Transcription factors activated in mammalian cells after clinically relevant doses of ionizing radiation. Oncogene 22, 5813–5827 (2003).
Denham, J. W. & Hauer-Jensen, M. The radiotherapeutic injury – a complex ‘wound’. Radiother. Oncol. 63, 129–145 (2002).
Man̆áková, Š, Puttonen, K. A., Raasmaja, A. & Männistö, P. T. Ara-C induces apoptosis in monkey fibroblast cells. Toxicol. Vitr. 17, 367–373 (2003).
Sonis, S. T. The biologic role for nuclear factor-kappaB in disease and its potential involvement in mucosal injury associated with anti-neoplastic therapy. Crit. Rev. Oral. Biol. Med. Publ. Am. Assoc. Oral. Biol. 13, 380–389 (2002).
Hall, P. D., Benko, H., Hogan, K. R. & Stuart, R. K. The influence of serum tumor necrosis factor-alpha and interleukin-6 concentrations on nonhematologic toxicity and hematologic recovery in patients with acute myelogenous leukemia. Exp. Hematol. 23, 1256–1260 (1995).
Kitada, S., Krajewski, S., Miyashita, T., Krajewska, M. & Reed, J. C. Gamma-radiation induces upregulation of Bax protein and apoptosis in radiosensitive cells in vivo. Oncogene 12, 187–192 (1996).
De Sousa, S. O. M., Mesquita, R. A., Pinto, D. S. & Gutkind, S. Immunolocalization of c-Fos and c-Jun in human oral mucosa and in oral squamous cell carcinoma. J. Oral. Pathol. Med. 31, 78–81 (2002).
Davis, R. J. Signal Transduction by the JNK Group of MAP Kinases. Cell 103, 239–252 (2000).
Billis, W., Fuks, Z. & Kolesnick, R. Signaling in and regulation of ionizing radiation-induced apoptosis in endothelial cells. Recent Prog. Horm. Res. 53, 85–92 (1998).
Bamba, S. et al. Matrix metalloproteinase-3 secretion from human colonic subepithelial myofibroblasts: role of interleukin-17. J. Gastroenterol. 38, 548–554 (2003).
Sasaki, M. et al. Differential regulation of metalloproteinase production, proliferation and chemotaxis of human lung fibroblasts by PDGF, Interleukin-1β and TNF-α. Mediators Inflamm. 9, 155–160 (2000).
Alikhani, M. et al. Lipopolysaccharides Indirectly Stimulate Apoptosis and Global Induction of Apoptotic Genes in Fibroblasts. J. Biol. Chem. 278, 52901–52908 (2003).
Sonis, S., Treister, N., Chawla, S., Demetri, G. & Haluska, F. Preliminary characterization of oral lesions associated with inhibitors of mammalian target of rapamycin in cancer patients. Cancer 116, 210–215 (2010).
Singer, S. et al. Cutaneous eruptions from ibrutinib resembling epidermal growth factor receptor inhibitor–induced dermatologic adverse events. J. Am. Acad. Dermatol. 88, 1271–1281 (2023).
Boers-Doets, C. B. et al. Oral Adverse Events Associated with Tyrosine Kinase and Mammalian Target of Rapamycin Inhibitors in Renal Cell Carcinoma: A Structured Literature Review. Oncologist 17, 135–144 (2012).
Yuan, A. et al. Oral adverse events in cancer patients treated with VEGFR-directed multitargeted tyrosine kinase inhibitors. Oral. Oncol. 51, 1026–1033 (2015).
Sibaud, V. et al. Dermatologic complications of anti-PD-1/PD-L1 immune checkpoint antibodies. Curr. Opin. Oncol. 28, 254–263 (2016).
Hofmann, L. et al. Cutaneous, gastrointestinal, hepatic, endocrine, and renal side-effects of anti-PD-1 therapy. Eur. J. Cancer 60, 190–209 (2016).
Schaberg, K. B. et al. Immunohistochemical analysis of lichenoid reactions in patients treated with anti-PD-L1 and anti-PD-1 therapy. J. Cutan. Pathol. 43, 339–346 (2016).
Maria, O. M., Eliopoulos, N. & Muanza, T. Radiation-Induced Oral Mucositis. Front. Oncol. 7, 89 (2017).
Scully, C., Epstein, J. & Sonis, S. Oral mucositis: A challenging complication of radiotherapy, chemotherapy, and radiochemotherapy. Part 2: Diagnosis and management of mucositis. Head. Neck 26, 77–84 (2004).
Li, N. et al. Clinical study of pharyngeal swab culture intervention in the treatment of radioactive oral mucositis induced by intensity-modulated radiotherapy for nasopharyngeal carcinoma. Chin J Clin. Ration. Drug. Use. 13, 29–32 (2020).
Bossi, P. et al. Salivary Cytokine Levels and Oral Mucositis in Head and Neck Cancer Patients Treated With Chemotherapy and Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 96, 959–966 (2016).
Kauark-Fontes, E. et al. Machine learning prediction model for oral mucositis risk in head and neck radiotherapy: a preliminary study. Support Care Cancer J. Multinatl. Assoc. Support Care Cancer 33, 96 (2025).
Dean, J. A. et al. Normal tissue complication probability (NTCP) modelling using spatial dose metrics and machine learning methods for severe acute oral mucositis resulting from head and neck radiotherapy. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 120, 21–27 (2016).
Satheeshkumar, P. S., El-Dallal, M. & Mohan, M. P. Feature selection and predicting chemotherapy-induced ulcerative mucositis using machine learning methods. Int. J. Med. Inf. 154, 104563 (2021).
Taheriyan, M., Safaee Nodehi, S., Niakan Kalhori, S. R. & Mohammadzadeh, N. A systematic review of the predicted outcomes related to hematopoietic stem cell transplantation: focus on applied machine learning methods’ performance. Expert Rev. Hematol. 15, 137–156 (2022).
Leppla, L., De Geest, S., Fierz, K., Deschler-Baier, B. & Koller, A. An oral care self-management support protocol (OrCaSS) to reduce oral mucositis in hospitalized patients with acute myeloid leukemia and allogeneic hematopoietic stem cell transplantation: a randomized controlled pilot study. Support. Care Cancer 24, 773–782 (2016).
Bezerra, P. M. M. et al. The effectiveness of an oral health education and prevention program on the incidence and severity of oral mucositis in pediatric cancer patients: a non-randomized controlled study. Support. Care Cancer 29, 7877–7885 (2021).
Yüce, U. Ö & Yurtsever, S. Effect of Education About Oral Mucositis Given to the Cancer Patients Having Chemotherapy on Life Quality. J. Cancer Educ. 34, 35–40 (2019).
On behalf of the Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society for Oral Oncology (MASCC/ISOO) et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support. Care Cancer 27, 3949–3967 (2019).
Kartin, P. T., Tasci, S., Soyuer, S. & Elmali, F. Effect of an Oral Mucositis Protocol on Quality of Life of Patients With Head and Neck Cancer Treated With Radiation Therapy. Clin. J. Oncol. Nurs. 18, E118–E125 (2014).
Legert, K. G., Remberger, M., Ringdén, O., Heimdahl, A. & Dahllöf, G. Reduced intensity conditioning and oral care measures prevent oral mucositis and reduces days of hospitalization in allogeneic stem cell transplantation recipients. Support. Care Cancer 22, 2133–2140 (2014).
Shieh, S. H., Wang, S. T., Tsai, S. T. & Tseng, C. C. Mouth care for nasopharyngeal cancer patients undergoing radiotherapy. Oral. Oncol. 33, 36–41 (1997).
Bos-den Braber, J., Potting, C. M. J., Bronkhorst, E. M., Huysmans, M.-C. D. N. J. M. & Blijlevens, N. M. A. Oral complaints and dental care of haematopoietic stem cell transplant patients: a qualitative survey of patients and their dentists. Support. Care Cancer 23, 13–19 (2015).
Saito, H. et al. Effects of professional oral health care on reducing the risk of chemotherapy-induced oral mucositis. Support. Care Cancer 22, 2935–2940 (2014).
Niikura, N. et al. Oral Care Evaluation to Prevent Oral Mucositis in Estrogen Receptor-Positive Metastatic Breast Cancer Patients Treated with Everolimus (Oral Care-BC): A Randomized Controlled Phase III Trial. Oncologist 25, e223–e230 (2020).
Elad, S. et al. Basic oral care for hematology–oncology patients and hematopoietic stem cell transplantation recipients: a position paper from the joint task force of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) and the European Society for Blood and Marrow Transplantation (EBMT). Support. Care Cancer 23, 223–236 (2015).
Cheng, B., Li, C. & Xia, J. Diagnosis and Treatment of Radiotherapy-Induced Oral Mucositis. Chin. J. Pract. Stomatol. 1, 513–516 (2008).
Yu, Y. et al. Effects of 9 oral care solutions on the prevention of oral mucositis: a network meta-analysis of randomized controlled trials. Med. (Baltim.) 99, e19661 (2020).
Cardona, A., Balouch, A., Abdul, M. M., Sedghizadeh, P. P. & Enciso, R. Efficacy of chlorhexidine for the prevention and treatment of oral mucositis in cancer patients: a systematic review with meta-analyses. J. Oral. Pathol. Med. 46, 680–688 (2017).
Ferretti, G. A. et al. Chlorhexidine prophylaxis for chemotherapy-and radiotherapy-induced stomatitis: A randomized double-blind trial. Oral. Surg. Oral. Med. Oral. Pathol. 69, 331–338 (1990).
Madan Kumar, P., Sequeira, P., Shenoy, K. & Shetty, J. The effect of three mouthwashes on radiation-induced oral mucositis in patients with head and neck malignancies: A randomized control trial. J. Cancer Res. Ther. 4, 3 (2008).
Foote, R. L. et al. Randomized trial of a chlorhexidine mouthwash for alleviation of radiation-induced mucositis. J. Clin. Oncol. 12, 2630–2633 (1994).
Choi, S.-E. & Kim, H.-S. Sodium Bicarbonate Solution versus Chlorhexidine Mouthwash in Oral Care of Acute Leukemia Patients Undergoing Induction Chemotherapy: A Randomized Controlled Trial. Asian Nurs. Res. 6, 60–66 (2012).
Chitapanarux, I. et al. Randomized control trial of benzydamine HCl versus sodium bicarbonate for prophylaxis of concurrent chemoradiation-induced oral mucositis. Support. Care Cancer 26, 879–886 (2018).
Braunstein, S. et al. GM-CSF Activates Regenerative Epidermal Growth and Stimulates Keratinocyte Proliferation in Human Skin In Vivo. J. Invest. Dermatol. 103, 601–604 (1994).
Yu, M., Yang, Z., Chen, F., Zhou, P. & Zhao, Y. Effect of granulocyte-macrophage colony-stimulating factor gargle and deglutition to prevent oral mucositis in patients after conditioning of hematopoietic stem cell transplantation. Chin J Inj. Repair Wound Heal. Electron. Ed. 13, 215–219 (2018).
Lin, F. & Xu, L. Clinical effect of Gm-CSF gargling on acute radiation oral mucositis of nasopharyngeal carcinoma. Chin. J. Clin. Ration. Drug. Use. 11, 77–78 (2018).
Saarilahti, K., Kajanti, M., Joensuu, T., Kouri, M. & Joensuu, H. Comparison of granulocyte-macrophage colony-stimulating factor and sucralfate mouthwashes in the prevention of radiation-induced mucositis: a double-blind prospective randomized phase III study. Int. J. Radiat. Oncol. 54, 479–485 (2002).
Makkonen, T. A. et al. Granulocyte macrophage-colony stimulating factor (GM-CSF) and sucralfate in prevention of radiation-induced mucositis: a prospective randomized study. Int. J. Radiat. Oncol. 46, 525–534 (2000).
Ryu, J. K. et al. The impact of concurrent granulocyte macrophage-colony stimulating factor on radiation-induced mucositis in head and neck cancer patients: A double-blind placebo-controlled prospective Phase III study by Radiation Therapy Oncology Group 9901. Int. J. Radiat. Oncol. 67, 643–650 (2007).
Hoffman, K. E. et al. The impact of concurrent granulocyte–macrophage colony-stimulating factor on quality of life in head and neck cancer patients: results of the randomized, placebo-controlled Radiation Therapy Oncology Group 9901 trial. Qual. Life Res. 23, 1841–1858 (2014).
Sparano, J. A. et al. Phase I Trial of Infusional Cyclophosphamide, Doxorubicin, and Etoposide plus Granulocyte-Macrophage Colony Stimulating Factor (GM-CSF) in Non-Hodgkin’s Lymphoma. Med. Oncol. 22, 257–268 (2005).
McAleese, J. J., Bishop, K. M., A’Hern, R. & Henk, J. M. Randomized phase II study of GM-CSF to reduce mucositis caused by accelerated radiotherapy of laryngeal cancer. Br. J. Radiol. 79, 608–613 (2006).
Sironi, M. et al. Benzydamine inhibits the release of tumor necrosis factor-alpha and monocyte chemotactic protein-1 by Candida albicans-stimulated human peripheral blood cells. Int. J. Clin. Lab. Res. 27, 118–122 (1997).
Schubert, M. M. & Newton, R. E. The use of benzydamine HCl for the management of cancer therapy-induced mucositis: preliminary report of a multicentre study. Int. J. Tissue React. 9, 99–103 (1987).
Epstein, J. B. et al. Benzydamine HCl for prophylaxis of radiation-induced oral mucositis: Results from a multicenter, randomized, double-blind, placebo-controlled clinical trial. Cancer 92, 875–885 (2001).
Rastogi, M. et al. Role of benzydamine hydrochloride in the prevention of oral mucositis in head and neck cancer patients treated with radiotherapy (>50 Gy) with or without chemotherapy. Support. Care Cancer 25, 1439–1443 (2017).
Zhang, X. et al. Comparative prevention potential of 10 mouthwashes on intolerable oral mucositis in cancer patients: A Bayesian network analysis. Oral. Oncol. 107, 104751 (2020).
Yu, Y. et al. Efficacy of nine mouthwashes for the prevention of oral mucositis in cancer patients: a network Meta-analysis. Chin. Nurs. Manag. 19, 350–358 (2019).
Ogino, K. et al. Antiulcer mechanism of action of rebamipide, a novel antiulcer compound, on diethyldithiocarbamate-induced antral gastric ulcers in rats. Eur. J. Pharmacol. 212, 9–13 (1992).
Naito, Y. et al. Hydroxyl radical scavenging by rebamipide and related compounds: Electron paramagnetic resonance study. Free Radic. Biol. Med. 18, 117–123 (1995).
Chaitanya, B., Pai, K. M., Yathiraj, P. H., Fernandes, D. & Chhaparwal, Y. Rebamipide gargle in preventive management of chemo-radiotherapy induced oral mucositis. Oral. Oncol. 72, 179–182 (2017).
Yokota, T. et al. Efficacy and safety of rebamipide liquid for chemoradiotherapy-induced oral mucositis in patients with head and neck cancer: a multicenter, randomized, double-blind, placebo-controlled, parallel-group phase II study. BMC Cancer 17, 314 (2017).
Le, Q.-T. et al. Palifermin Reduces Severe Mucositis in Definitive Chemoradiotherapy of Locally Advanced Head and Neck Cancer: A Randomized, Placebo-Controlled Study. J. Clin. Oncol. 29, 2808–2814 (2011).
Henke, M. et al. Palifermin Decreases Severe Oral Mucositis of Patients Undergoing Postoperative Radiochemotherapy for Head and Neck Cancer: A Randomized, Placebo-Controlled Trial. J. Clin. Oncol. 29, 2815–2820 (2011).
Bradstock, K. F. et al. A randomized trial of prophylactic palifermin on gastrointestinal toxicity after intensive induction therapy for acute myeloid leukaemia. Br. J. Haematol. 167, 618–625 (2014).
Wilmore, D. W. & Shabert, J. K. Role of glutamine in immunologic responses. Nutrition 14, 618–626 (1998).
Alsubaie, H. M. et al. Glutamine for prevention and alleviation of radiation-induced oral mucositis in patients with head and neck squamous cell cancer: Systematic review and meta-analysis of controlled trials. Head. Neck 43, 3199–3213 (2021).
Chattopadhyay, S., Saha, A., Azam, M., Mukherjee, A. & Sur, P. K. Role of oral glutamine in alleviation and prevention of radiation-induced oral mucositis: A prospective randomized study. South Asian J. Cancer 03, 008–012 (2014).
Peterson, D. E., Jones, J. B. & Petit, R. G. Randomized, placebo-controlled trial of Saforis for prevention and treatment of oral mucositis in breast cancer patients receiving anthracycline-based chemotherapy. Cancer 109, 322–331 (2007).
Anderson, P. M., Schroeder, G. & Skubitz, K. M. Oral glutamine reduces the duration and severity of stomatitis after cytotoxic cancer chemotherapy. Cancer 83, 1433–1439 (1998).
Soutome, S. et al. Risk factors for severe radiation-induced oral mucositis in patients with oral cancer. J. Dent. Sci. 16, 1241–1246 (2021).
Awidi, A. et al. Double-blind, placebo-controlled cross-over study of oral pilocarpine for the prevention of chemotherapy-induced oral mucositis in adult patients with cancer. Eur. J. Cancer 37, 2010–2014 (2001).
Lockhart, P. B. et al. Randomized controlled trial of pilocarpine hydrochloride for the moderation of oral mucositis during autologous blood stem cell transplantation. Bone Marrow Transpl. 35, 713–720 (2005).
Chung, H. et al. The Nuts and Bolts of Low-level Laser (Light) Therapy. Ann. Biomed. Eng. 40, 516–533 (2012).
Nunes, L. F. M. et al. Prophylactic photobiomodulation therapy using 660 nm diode laser for oral mucositis in paediatric patients under chemotherapy: 5-year experience from a Brazilian referral service. Lasers Med. Sci. 35, 1857–1866 (2020).
Patel, P. et al. Clinical practice guideline for the prevention of oral and oropharyngeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update. Eur. J. Cancer 154, 92–101 (2021).
He, M., Zhang, B., Shen, N., Wu, N. & Sun, J. A systematic review and meta-analysis of the effect of low-level laser therapy (LLLT) on chemotherapy-induced oral mucositis in pediatric and young patients. Eur. J. Pediatr. 177, 7–17 (2018).
Peng, J. et al. Low-level laser therapy in the prevention and treatment of oral mucositis: a systematic review and meta-analysis. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 130, 387–397.e9 (2020).
De Lima, V. H. S., De Oliveira-Neto, O. B., Da Hora Sales, P. H., Da Silva Torres, T. & De Lima, F. J. C. Effectiveness of low-level laser therapy for oral mucositis prevention in patients undergoing chemoradiotherapy for the treatment of head and neck cancer: A systematic review and meta-analysis. Oral. Oncol. 102, 104524 (2020).
Dantas, J. B. et al. Evaluation of preventive laser photobiomodulation in patients with head and neck cancer undergoing radiochemotherapy: Laser in patients with head and neck cancer. Spec. Care Dent. Publ. Am. Assoc. Hosp. Dent. Acad. Dent. Handicap. Am. Soc. Geriatr. Dent. 40, 364–373 (2020).
Sperandio, F. F. et al. Low-level laser therapy can produce increased aggressiveness of dysplastic and oral cancer cell lines by modulation of Akt/mTOR signaling pathway. J. Biophotonics 6, 839–847 (2013).
Gomes Henriques, Á. C. et al. Low-level laser therapy promotes proliferation and invasion of oral squamous cell carcinoma cells. Lasers Med. Sci. https://doi.org/10.1007/s10103-014-1535-2 (2014).
Frigo, L. et al. The effect of low-level laser irradiation (In-Ga-Al-AsP - 660 nm) on melanoma in vitro and in vivo. BMC Cancer 9, 404 (2009).
Antunes, H. S. et al. Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis. Oral. Oncol. 71, 11–15 (2017).
Brandão, T. B. et al. Locally advanced oral squamous cell carcinoma patients treated with photobiomodulation for prevention of oral mucositis: retrospective outcomes and safety analyses. Support. Care Cancer 26, 2417–2423 (2018).
Lai, C.-C., Chen, S.-Y., Tu, Y.-K., Ding, Y.-W. & Lin, J.-J. Effectiveness of low level laser therapy versus cryotherapy in cancer patients with oral mucositis: Systematic review and network meta-analysis. Crit. Rev. Oncol. Hematol. 160, 103276 (2021).
Morais, M. O. et al. A prospective study on oral adverse effects in head and neck cancer patients submitted to a preventive oral care protocol. Support. Care Cancer J. Multinatl. Assoc. Support. Care Cancer 28, 4263–4273 (2020).
Peng, H. et al. A network meta-analysis in comparing prophylactic treatments of radiotherapy-induced oral mucositis for patients with head and neck cancers receiving radiotherapy. Oral. Oncol. 75, 89–94 (2017).
Vokurka, S. et al. The comparative effects of povidone-iodine and normal saline mouthwashes on oral mucositis in patients after high-dose chemotherapy and APBSCT—results of a randomized multicentre study. Support. Care Cancer 13, 554–558 (2005).
Etiz, D. et al. Clinical and histopathological evaluation of sucralfate in prevention of oral mucositis induced by radiation therapy in patients with head and neck malignancies. Oral. Oncol. 36, 116–120 (2000).
Castagna, L. et al. Prevention of mucositis in bone marrow transplantation: A double blind randomised controlled trial of sucralfate. Ann. Oncol. 12, 953–955 (2001).
Ala, S. et al. Efficacy of Sucralfate Mouth Wash in Prevention of 5-fluorouracil Induced Oral Mucositis: A Prospective, Randomized, Double-Blind, Controlled Trial. Nutr. Cancer 68, 456–463 (2016).
Wilairat, P. et al. Comparative efficacy and safety of interventions for preventing chemotherapy-induced oral mucositis in adult cancer patients: a systematic review and network meta-analysis. Eur. J. Hosp. Pharm. 27, 103–110 (2020).
Carter, D. L. et al. Double blind randomized trial of sucralfate vs placebo during radical radiotherapy for head and neck cancers. Head. Neck 21, 760–766 (1999).
Nottage, M. et al. Sucralfate mouthwash for prevention and treatment of 5-fluorouracil-induced mucositis: a randomized, placebo-controlled trial. Support. Care Cancer 11, 41–47 (2003).
Al-Rudayni, A. H. M., Gopinath, D., Maharajan, M. K., Veettil, S. K. & Menon, R. K. Efficacy of Oral Cryotherapy in the Prevention of Oral Mucositis Associated with Cancer Chemotherapy: Systematic Review with Meta-Analysis and Trial Sequential Analysis. Curr. Oncol. 28, 2852–2867 (2021).
Park, S. & Lee, H. S. Meta-analysis of oral cryotherapy in preventing oral mucositis associated with cancer therapy. Int. J. Nurs. Pract. 25, e12759 (2019).
Sung, L. et al. Guideline for the prevention of oral and oropharyngeal mucositis in children receiving treatment for cancer or undergoing haematopoietic stem cell transplantation. BMJ Support. Palliat. Care 7, 7–16 (2017).
Svanberg, A., Öhrn, K. & Birgegård, G. Oral cryotherapy reduces mucositis and improves nutrition – a randomised controlled trial. J. Clin. Nurs. 19, 2146–2151 (2010).
Sorensen, J. B., Skovsgaard, T., Bork, E., Damstrup, L. & Ingeberg, S. Double-blind, placebo-controlled, randomized study of chlorhexidine prophylaxis for 5-fluorouracil-based chemotherapy-induced oral mucositis with nonblinded randomized comparison to oral cooling (cryotherapy) in gastrointestinal malignancies. Cancer 112, 1600–1606 (2008).
Singh, A. et al. Intraoral radiation stents-Primer for clinical use in head and neck cancer therapy. Head. Neck 43, 4010–4017 (2021).
Yoneda, S. et al. Effects of oral care on development of oral mucositis and microorganisms in patients with esophageal cancer. Jpn. J. Infect. Dis. 60, 23–28 (2007).
Djuric, M., Hillier-Kolarov, V., Belic, A. & Jankovic, L. Mucositis prevention by improved dental care in acute leukemia patients. Support. Care Cancer 14, 137–146 (2006).
Ribeiro, I. L. A. et al. Integrated oral care contributes positively to the course of treatment of oncopediatric patients. Eur. J. Pediatr. 180, 2757–2764 (2021).
Rojas de Morales, T. et al. Oral-disease prevention in children with cancer: testing preventive protocol effectiveness. Med. Oral. Organo. Soc. Espanola Med. Oral. Acad. Iberoam. Patol. Med. Bucal 6, 326–334 (2001).
Sudoh, Y., Cahoon, E. E., Gerner, P. & Wang, G. K. Tricyclic antidepressants as long-acting local anesthetics. Pain 103, 49–55 (2003).
Sio, T. T. et al. Effect of Doxepin Mouthwash or Diphenhydramine-Lidocaine-Antacid Mouthwash vs Placebo on Radiotherapy-Related Oral Mucositis Pain: The Alliance A221304 Randomized Clinical Trial. JAMA 321, 1481 (2019).
Leenstra, J. L. et al. Doxepin Rinse Versus Placebo in the Treatment of Acute Oral Mucositis Pain in Patients Receiving Head and Neck Radiotherapy With or Without Chemotherapy: A Phase III, Randomized, Double-Blind Trial (NCCTG-N09C6 [Alliance]). J. Clin. Oncol. 32, 1571–1577 (2014).
Epstein, J. B., Epstein, J. D., Epstein, M. S., Oien, H. & Truelove, E. L. Doxepin rinse for management of mucositis pain in patients with cancer: one week follow-up of topical therapy. Spec. Care Dent. 28, 73–77 (2008).
Epstein, J. B. et al. Oral topical doxepin rinse: analgesic effect in patients with oral mucosal pain due to cancer or cancer therapy. Oral Oncol. (2001).
Barasch, A., Elad, S., Altman, A., Damato, K. & Epstein, J. Antimicrobials, mucosal coating agents, anesthetics, analgesics, and nutritional supplements for alimentary tract mucositis. Support. Care Cancer 14, 528–532 (2006).
Carnel, S. B., Blakeslee, D. B., Oswald, S. G. & Barnes, M. Treatment of Radiation- and Chemotherapy-Induced Stomatitis. Otolaryngol. Neck Surg. 102, 326–330 (1990).
Alterio, D. et al. Tetracaine oral gel in patients treated with radiotherapy for head-and-neck cancer: Final results of a phase II study. Int. J. Radiat. Oncol. 64, 392–395 (2006).
Agha-Hosseini, F., Pourpasha, M., Amanlou, M. & Moosavi, M.-S. Mouthwash Containing Vitamin E, Triamcinolon, and Hyaluronic Acid Compared to Triamcinolone Mouthwash Alone in Patients With Radiotherapy-Induced Oral Mucositis: Randomized Clinical Trial. Front. Oncol. 11, 614877 (2021).
Ueno, T., Yatsuoka, W., Ishiki, H., Miyano, K. & Uezono, Y. Effects of an oral mucosa protective formulation on chemotherapy- and/or radiotherapy-induced oral mucositis: a prospective study. BMC Cancer 22, 90 (2022).
Cheng, Y. et al. Local analgesic effect of a bioadhesive barrier-forming oral liquid in cancer patients with oral mucositis caused by chemotherapy and/or radiotherapy: a randomized multicenter, single-use, positive-controlled, open-label study. OncoTargets Ther. 11, 8555–8564 (2018).
Hadjieva, T., Cavallin-Ståhl, E., Linden, M. & Tiberg, F. Treatment of oral mucositis pain following radiation therapy for head-and-neck cancer using a bioadhesive barrier-forming lipid solution. Support. Care Cancer 22, 1557–1562 (2014).
Roopashri, G., Jayanthi, K. & Guruprasad, R. Efficacy of benzydamine hydrochloride, chlorhexidine, and povidone iodine in the treatment of oral mucositis among patients undergoing radiotherapy in head and neck malignancies: A drug trail. Contemp. Clin. Dent. 2, 8 (2011).
Cabrera-Jaime, S. et al. Efficacy of Plantago major, chlorhexidine 0.12% and sodium bicarbonate 5% solution in the treatment of oral mucositis in cancer patients with solid tumour: A feasibility randomised triple-blind phase III clinical trial. Eur. J. Oncol. Nurs. 32, 40–47 (2018).
Mohammadi, F. et al. Effectiveness of sodium bicarbonate and zinc chloride mouthwashes in the treatment of oral mucositis and quality of life in patients with cancer under chemotherapy. Nurs. Open 9, 1602–1611 (2022).
Isham, N. & Ghannoum, M. A. Antifungal activity of miconazole against recent Candida strains: Miconazole antifungal activity vs. Candida. Mycoses 53, 434–437 (2010).
Vazquez, J. A. & Sobel, J. D. Miconazole Mucoadhesive Tablets: A Novel Delivery System. Clin. Infect. Dis. 54, 1480–1484 (2012).
Bensadoun, R. et al. Comparison of the efficacy and safety of miconazole 50-mg mucoadhesive buccal tablets with miconazole 500-mg gel in the treatment of oropharyngeal candidiasis: A prospective, randomized, single-blind, multicenter, comparative, phase III trial in patients treated with radiotherapy for head and neck cancer. Cancer 112, 204–211 (2008).
Orvain, C. et al. Miconazole mucoadhesive buccal tablet in high-dose therapy with autologous stem cell transplantation (HDT/ASCT)-induced mucositis. Support. Care Cancer 23, 359–364 (2015).
Feng, Y. Clinical observation of recombinant human IL-11 adjuvant therapy for radioactive oral mucosa injury. Electron. J. Gen. Stomatol. 18, 19 (2018).
Zheng, S., Hu, X. & Xu, Z. Effect of IL-11 on stomatitis after high dose MTX chemotherapy in children with acute lymphoblastic leukemia. Zhejiang Pract. Med. 213, 214 (2018).
Pan, Y., Wu, H. & Li, Y. Effect of recombinant human interleukin-11 treatment on prognosis of patients with radiochemoradiotherapy in the treatment of nasopharyngeal carcinoma. J. Clin. Otorhinolaryngol. Head. Neck. Surg. China 31, 945–948 (2017).
García-Gozalbo, B. & Cabañas-Alite, L. A Narrative Review about Nutritional Management and Prevention of Oral Mucositis in Haematology and Oncology Cancer Patients Undergoing Antineoplastic Treatments. Nutrients 13, 4075 (2021).
Tsujimoto, T. et al. L-glutamine decreases the severity of mucositis induced by chemoradiotherapy in patients with locally advanced head and neck cancer: A double-blind, randomized, placebo-controlled trial. Oncol. Rep. 33, 33–39 (2015).
Tunér, J. & Jenkins, P. A. Parameter Reproducibility in Photobiomodulation. Photomed. Laser Surg. 34, 91–92 (2016).
Campos, T. M. et al. Photobiomodulation in oral mucositis in patients with head and neck cancer: a systematic review and meta-analysis followed by a cost-effectiveness analysis. Support. Care Cancer 28, 5649–5659 (2020).
Da Silva, B. M. et al. Most used photobiomodulation dosimetry parameters to treat oral mucositis after preconditioning for hematopoietic stem cell transplantation: systematic review and meta-analysis. Support. Care Cancer 30, 3721–3732 (2022).
Ramos-Pinto, M. B. et al. Intraoral versus extraoral photobiomodulation therapy in the prevention of oral mucositis in HSCT patients: a randomized, single-blind, controlled clinical trial. Support. Care Cancer 29, 6495–6503 (2021).
Treister, N. S. et al. A Feasibility Study Evaluating Extraoral Photobiomodulation Therapy for Prevention of Mucositis in Pediatric Hematopoietic Cell Transplantation. Photomed. Laser Surg. 34, 178–184 (2016).
Sarvizadeh, M. et al. Morphine mouthwash for the management of oral mucositis in patients with head and neck cancer. Adv. Biomed. Res. 4, 44 (2015).
Schaller, A. K. C. S., Peterson, A. & Bäckryd, E. Pain management in patients undergoing radiation therapy for head and neck cancer – a descriptive study. Scand. J. Pain. 21, 256–265 (2021).
Cerchietti, L. C. A. et al. Effect of topical morphine for mucositis-associated pain following concomitant chemoradiotherapy for head and neck carcinoma. Cancer 95, 2230–2236 (2002).
Martin, J. L. et al. Chronic Morphine Administration Delays Wound Healing by Inhibiting Immune Cell Recruitment to the Wound Site. Am. J. Pathol. 176, 786–799 (2010).
Rook, J. M., Hasan, W. & McCarson, K. E. Morphine-induced early delays in wound closure: Involvement of sensory neuropeptides and modification of neurokinin receptor expression. Biochem. Pharmacol. 77, 1747–1755 (2009).
AkhavanKarbassi, M. H., Yazdi, M. F., Ahadian, H. & SadrAbad, M. J. Randomized DoubleBlind PlaceboControlled Trial of Propolis for Oral Mucositis in Patients Receiving Chemotherapy for Head and Neck Cancer. Asian Pac. J. Cancer Prev. APJCP 17, 3611–3614 (2016).
An, W., Li, S. & Qin, L. Role of honey in preventing radiation-induced oral mucositis: a meta-analysis of randomized controlled trials. Food Funct. 12, 3352–3365 (2021).
Lima, I. C. G. D. S. et al. Clinical applicability of natural products for prevention and treatment of oral mucositis: a systematic review and meta-analysis. Clin. Oral. Investig. 25, 4115–4124 (2021).
Tomaževič, T. & Jazbec, J. A double blind randomised placebo controlled study of propolis (bee glue) effectiveness in the treatment of severe oral mucositis in chemotherapy treated children. Complement. Ther. Med. 21, 306–312 (2013).
Bardy, J. et al. A double-blind, placebo-controlled, randomised trial of active manuka honey and standard oral care for radiation-induced oral mucositis. Br. J. Oral. Maxillofac. Surg. 50, 221–226 (2012).
Hawley, P., Hovan, A., McGahan, C. E. & Saunders, D. A randomized placebo-controlled trial of manuka honey for radiation-induced oral mucositis. Support. Care Cancer 22, 751–761 (2014).
Lalla, R. V. et al. Efficacy and safety of Dentoxol® in the prevention of radiation-induced oral mucositis in head and neck cancer patients (ESDOM): a randomized, multicenter, double-blind, placebo-controlled, phase II trial. Support. Care Cancer 28, 5871–5879 (2020).
Lalla, R. V. et al. A randomized, double-blind, placebo-controlled trial of misoprostol for oral mucositis secondary to high-dose chemotherapy. Support. Care Cancer 20, 1797–1804 (2012).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (U23A20445) and the Science and Technology Program of Guangzhou (202206080009). The authors are grateful to the other experts in the specialist group and evidence-based medicine group for their contributions in the development of this consensus and their names are listed as follows. Fangchun Chen, Ruiyang Chen, Hongxia Dan, Gefei Du, Huabing Ge, Ying Han, Yun Hong, Lu Jiang, Mei Lin, Rui Lu, Xiaobo Luo, Xingchen Peng, Xiangmin Qi, Jing Shi, Hongying Sun, Yan Sun, Zheng Sun, Yaqin Tan, Yaling Tang, Hui Wang, Wanchun Wang, Xiaoping Wang, Yufeng Wang, Zhi Wang, Fanglong Wu, Zhimin Yan, Jing Zhang, Yuxing Zhang, Zengtong Zhou, Yu Zhou, Guopei Zhu. The authors also thank Weiyu Li for her assistance in preparing the consensus.
Author information
Authors and Affiliations
Contributions
Conceptualization & Investigation, B.C.; Supervision, B.C.; Original draft, J.X., X.T., and Q.H.; Review & Editing, W.L., X.T., G.Z., H.Z., H.H., G.T., T.W., Q.C., Y.F., X.G., H.L., C.H., Y.Z., X.S., L.W., X.Z., Q.L., R.T., Y.H., Y.C., W.W., Y.Z., Y.W., M.N., X.J., X.W., Y.N., and C.Y.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xia, J., Tao, X., Hu, Q. et al. Expert consensus on the prevention and treatment of radiochemotherapy-induced oral mucositis. Int J Oral Sci 17, 54 (2025). https://doi.org/10.1038/s41368-025-00382-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41368-025-00382-8
This article is cited by
-
Efficacy of acupuncture in managing radiotherapy/chemotherapy-induced oral mucositis: a systematic review and meta-analysis
Supportive Care in Cancer (2025)