Abstract
Objective
To determine the association between fertility treatment, socioeconomic status (SES), and neonatal and post-neonatal mortality.
Study design
Retrospective cohort study of all births (19,350,344) and infant deaths from 2014–2018 in the United States. The exposure was mode of conception—spontaneous vs fertility treatment. The outcome was neonatal (<28d), and post-neonatal (28d–1y) mortality. Multivariable logistic models were stratified by SES.
Result
The fertility treatment group had statistically significantly higher odds of neonatal mortality (high SES OR 1.59; CI [1.5, 1.68], low SES OR 2.11; CI [1.79, 2.48]) and lower odds of post-neonatal mortality (high SES OR 0.87, CI [0.76, 0.996], low SES OR 0.6, CI [0.38, 0.95]). SES significantly modified the effect of ART/NIFT on neonatal and post-neonatal mortality.
Conclusions
Fertility treatment is associated with higher neonatal and lower post-neonatal mortality and SES modifies this effect. Socioeconomic policies and support for vulnerable families may help reduce rates of infant mortality.
Similar content being viewed by others
Introduction
The use of assisted reproductive technology (ART), which includes all fertility treatments in which eggs or embryos are handled including in-vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), has increased dramatically over the past two decades. In 2018 alone, ART accounted for ~2% (>73,000) of live births [1]; the use of non-IVF fertility treatment (NIFT), which includes the use of ovarian stimulating drugs, accounts for ~3–7% of births [2].
The effect of fertility treatment (ART/NIFT) on infant outcomes remains under study. Adverse neonatal outcomes include increased incidence of preterm birth, low birth weight, and congenital anomalies [2,3,4,5,6,7,8]. Adverse infant and childhood outcomes include increased incidence of vascular and cardiac dysfunction [9,10,11,12,13,14]. However, data on the risk of infant, neonatal and post-neonatal mortality among babies born using ART/NIFT compared to spontaneously conceived babies are conflicting [15,16,17,18]. In the US, socioeconomic status (SES) has been shown to be associated with neonatal and post-neonatal outcomes [19, 20] but few studies have explored its effect on infant mortality among babies born through ART/NIFT.
We used a US population-based natality database to investigate infant, neonatal, and post-neonatal mortality following ART/NIFT. We focused on the incidence, timing, and etiology of infant mortality, and the impact of SES on mortality rates. We hypothesized that overall mortality would be increased in ART/NIFT, but mortality differences would be influenced by plurality, prematurity, and maternal socioeconomic status.
Methods
Population
We performed a retrospective, population-based cohort study of all live births in the US from 2014–2018. The Center for Disease Control and Prevention (CDC) provides annual cohort linked birth/infant death public use data files (https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm). These datasets contain all live births in the United States linked to death certificates during the first year of life. Detailed documentation of each item collected on birth and death certificates is available at https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm. We evaluated data files starting in 2014, as universal adoption of the revised birth certificate became mandatory for all states at that time.
Exposure variables
The primary predictor was mode of conception—spontaneous versus use of fertility treatment (ART/NIFT). The revised birth certificate data includes a question about receipt of any fertility treatment. Certificates with a “No” to this question were categorized in the spontaneous conception group. Certificates with a “Yes” answered a follow up question regarding the receipt of ART specifically. Certificates with a “Yes” to this second question were categorized in the ART group. Those with a “Yes” to the first question and “No” to the second question were categorized in the NIFT group. For most of our analyses, the ART and NIFT group were combined as the fertility treatment group. The spontaneous conception group served as the reference category for the analyses. Birth records with missing information about fertility treatment were excluded.
We also assessed the effect of maternal socioeconomic status on our outcome. We defined maternal socio-economic status using education and insurance variables from the birth certificate. Higher socio-economic status (SES) was defined as a maternal education level of community college or university degree, and private insurance. Lower SES was defined as a maternal education of a high school degree or less, and public insurance. Intermediate SES was comprised of all other records. However, our analysis compared only low to high SES.
Outcomes
The primary outcome was infant mortality (death within the first year of life). We further divided mortality into neonatal (0–28 days) and post-neonatal (29–365 days) mortality. Secondary outcomes were time to death and causes of neonatal and post-neonatal death.
We defined sudden unexpected infant death (SUID) as deaths with the following ICD-10 codes: sudden infant death syndrome (SIDS)—R95, deaths from other ill-defined or unknown causes - R99; and accidental strangulation or suffocation in bed - W75, as per the CDC [21] and prior studies [22].
Covariates
In addition to SES level, we identified the following covariates a priori as potential confounders in the relationship between mode of conception and infant death: maternal age, self-reported maternal race, body mass index (BMI), cigarette smoking, prematurity, intrauterine growth restriction (IUGR). The social construct of maternal race, as categorized and self-reported in the birth certificate, was included in the analysis as a descriptor of the study population and as a potential confounder, associated with both the exposure and outcome. Non-Hispanic American Indian or Alaskan Native (AIAN), Native Hawaiian or Other Pacific Islander (NHOPI) and those who selected more than one race were categorized together in the “Other” category since the numbers in these categories were small. We adjusted all multivariable models for these covariates. IUGR was defined as birth weight z-score less than −1.3 [23, 24], with z-score assigned based on gestational age and sex using the LMS method (lambda for the skew, mu for the median, and sigma for the generalized coefficient of variation) described by Fenton et al. [25, 26].
Statistical analysis
We used Chi square tests to compare count data and t-tests to compare means of different groups. We used multinomial logit models to assess the trend of births and a logistic model to assess the trend of mortality after fertility treatment.
We used multivariable logistic models to calculate odds ratios (OR) and 95% confidence intervals (95% CI) for infant, neonatal, and post-neonatal mortality among babies born after fertility treatment (ART/NIFT) compared to those born through spontaneous conception, adjusting for the above-mentioned covariates. We stratified our analysis by SES (high versus low) and assessed for interactions between SES and fertility treatment. We constructed survival curves for each conception group by SES and plurality to visually depict timing of death in each group. Finally, using the causes of death data, we identified the most common reasons for neonatal and post-neonatal deaths in each of the conception groups using descriptive statistics.
For supplementary analyses, we assessed ART and NIFT as separate predictors, stratified our results by plurality (single versus multiple gestation), and constructed sequential models, with and without prematurity, to evaluate its effect on infant mortality.
A p < 0.05 was considered statistically significant. All analyses were performed using Stata Statistical Software version 17.0 (StataCorp LLC, College Station, TX). No institutional reviewing board approval was necessary since the data used was publicly available and deidentified.
Results
A total of 19,632,665 live births were documented from 2014–18; 258,963 (1.32%) had missing information regarding mode of conception and were excluded from our study (Supplementary Fig. 1). Of 19,350,344 births, 191,941 (0.99%) followed ART and 118,941 (0.61%) followed NIFT. Compared to spontaneous pregnancies, babies conceived via fertility treatments (ART/NIFT) were more often multiple gestation (29.7% versus 3%), premature (26.45% versus 11.19%), had lower median birth weight z-scores (−0.2 versus −0.12) and had higher rates of congenital malformations (0.42% vs 0.27%) (Table 1). Mothers who received ART/NIFT were more likely to be in the high SES category (73.07% vs. 30.22%).
Birth of infants conceived using ART/NIFT increased from 2014–2018, with almost a 50% increase in ART births (p < 0.001) and a 10% increase in NIFT births (p < 0.001) (Supplementary Fig. 2a). Neonatal mortality among infants conceived using ART decreased by 32% over the study period (p < 0.001) (Supplementary Fig. 2b) while the reduction in neonatal mortality in the NIFT group was not statistically significant (p = 0.3). The decrease in post-neonatal mortality among ART/NIFT infants was modest and not significant. Neonatal and post-neonatal mortality among spontaneously conceived infants remained constant over the years (Supplementary Fig. 2b).
Over the 5-year period, overall infant mortality was 5.8 deaths per 1000 live births (0.58%). It was greater in the ART/NIFT group (1.16%) compared to spontaneously conceived infants (0.57%, p < 0.001) (Fig. 1). Neonatal mortality was 3.8 deaths per 1000 live births (0.38%), while post-neonatal mortality was 1.9 deaths per 1,000 live births (0.19%). Compared to the spontaneously conceived group, the ART/NIFT group had a higher neonatal mortality rate (1.03% vs 0.37%) but lower post-neonatal mortality rate (0.13% vs 0.19%) overall, and for singleton and multiple gestation births (Fig. 1, p < 0.001 for all comparisons).
After adjusting for confounders, neonates born through ART/NIFT had statistically significantly higher odds of mortality than those who were spontaneously conceived (OR = 1.61, CI 1.54, 1.68) (Table 2). Odds of post-neonatal mortality were lower in the ART/NIFT group (OR = 0.86, CI 0.77, 0.95) and this was statistically significant (Table 2). On stratification, SES was found to be a modifier of the effect of ART/NIFT on infant, neonatal and post-neonatal mortality. Infants in the low SES group had higher odds of neonatal mortality and lower odds of post-neonatal mortality than infants in the high SES group. In a test for interaction, the p-value for the interaction term between ART/NIFT and SES was 0.01 for both neonatal and post-neonatal mortality and 0.77 for infant mortality (Table 2). When ART and NIFT were treated as independent predictors, similar trends were seen in mortality outcomes (Supplementary Table 1).
Survival curves constructed for the first year of life, including the neonatal period (birth – 28 days) and post-neonatal period (29–365 days), crossed from higher to lower mortality rate following ART/NIFT compared to spontaneous conception at approximately 110–120 days of life for singletons and 50–60 days of life for multiple gestation births (Fig. 2A, B). This crossover effect disappeared after stratification into high and low SES categories, with persistence of lower survival following ART/NIFT in both high and low SES groups (Fig. 2C–F).
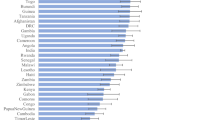
The three most common causes of neonatal death were conditions related to low birth weight or prematurity and other perinatal conditions (including cardiovascular, neurological etc) for both the spontaneously conceived and ART/NIFT groups (Fig. 3a). The single most common cause of post-neonatal death in both groups was SIDS (spontaneous, 17.55% versus ART/NIFT, 9.63%). SUID (including SIDS, other ill-defined or unknown causes and accidental suffocation or strangulation in bed) accounted for 42.28% of post-neonatal deaths among spontaneously conceived children, compared to 18.52% among infants conceived with ART/NIFT (p < 0.001) (Fig. 3b).
In supplementary analyses, after adjusting for prematurity, the increased odds of neonatal mortality following ART/NIFT decreased (OR 1.96 [CI 1.88, 2.05] excluding prematurity; OR 1.61 [CI 1.54, 1.68] including prematurity) and the decreased odds of post-neonatal mortality (OR 0.93, CI 0.83, 1.03) further decreased and became statistically significant (OR 0.86, CI 0.77, 0.95) (Supplementary Table 2). However, this confounding effect of prematurity was not seen once data were stratified by plurality. Stratification by plurality revealed an interaction between ART/NIFT and plurality (Supplementary Table 2) for both neonatal and post-neonatal death with higher increased odds of neonatal mortality (multiple gestation OR 1.98, CI 1.87, 2.10; single gestation OR 1.5, CI 1.4, 1.61) and lower decreased odds of post-neonatal mortality (multiple gestation OR 0.92, CI 0.78, 1.07; single gestation OR 0.81, CI 0.7, 0.95) among multiple gestation infants.
Discussion
We compared the risk of mortality and timing of death among infants conceived with fertility treatment (ART/NIFT) compared to those conceived spontaneously across the United States from 2014–2018. We found that although overall infant mortality following ART/NIFT decreased over the study period, it remained higher than mortality among spontaneously conceived infants, even after adjusting for important confounders. We demonstrated that higher infant mortality following ART/NIFT was driven by higher neonatal mortality, while post-neonatal mortality among ART/NIFT infants was lower. Finally, we demonstrated SES is a significant modifier of the effect of ART/NIFT on neonatal and post-neonatal mortality.
Prior studies of infant mortality following ART/NIFT have demonstrated inconsistent results [4, 6, 27,28,29,30,31]. In a Swedish cohort of singletons, overall infant mortality was higher among those born following ART, but adjusted models did not include gestational age [28]. Post-neonatal mortality was elevated in this cohort, although the effect was not statistically significant [28]. A US population-based study demonstrated higher neonatal mortality among sub-fertile women, but lower infant and neonatal mortality among IVF treated women [4]. The Massachusetts Outcome Study also demonstrated higher perinatal mortality among sub-fertile women compared to fertile women but no difference between fertile and ART treated women [6]. On the other hand, Chang et al found a decreased risk of perinatal death among babies born <28-weeks gestation in a separate US cohort of 3 states, that they attributed to earlier detection and management of adverse conditions of the mother and fetus [29]. Previously, our group demonstrated a two-fold increase in mortality following ART among infants diagnosed with pulmonary vascular disease in a US population-based study, but these differences became insignificant after controlling for gestational age [31]. In a separate single center study, we found a non-significant elevation in 1-year mortality for ART versus spontaneously conceived very preterm infants (<32 weeks) [32].
Although we also found that infant mortality is higher among infants conceived using ART/NIFT, this effect was driven specifically by higher neonatal mortality. The most common causes of neonatal mortality were related to prematurity and low birth weight. Prior studies have demonstrated higher rates of preterm birth, low birth weight and small-for-gestation birthweight in infants born after fertility treatment [4, 5]. Thus, the increased rates of these complications among ART/NIFT groups are likely the reason for higher neonatal mortality in our study population. Biological explanations for increased rates of adverse perinatal outcomes include suboptimal endometrial development and abnormal placentation, which may be precursors of fertility treatment [18]. Prior studies have demonstrated a direct effect of multiple gestation following ART/NIFT on increased rates of prematurity [33]. We found that multiple gestation modifies the effect of ART/NIFT on neonatal mortality. Thus, focus on mitigating these complications including restricting multiple gestation during ART/NIFT should be a focus of on-going efforts to reduce infant mortality, specifically neonatal mortality.
Prior studies have found an association between lower SES and higher rates of neonatal mortality [19, 20, 34,35,36,37]. Singh and Kogan demonstrated widening socioeconomic disparities in neonatal mortality in the United States from 1985–2001 [19]. Ratnasiri et al previously demonstrated a “prominent effect” of maternal socio-economic status measured by education, residence in rural areas, insurance and receipt of Supplemental Nutrition Program for Women, Infants and Children (WIC) on infant mortality in a cohort of births in California [34]. In our study, we also found an association between SES and neonatal mortality. The odds of neonatal mortality among ART/NIFT infants were increased in both the low and high SES groups and the increase in odds was greater in the low SES group. Thus, in addition to continued efforts to decrease multiple gestation, preterm birth rates and other complications [38, 39], dedicated socioeconomic resources for those most at risk of disparate neonatal outcomes (those with lower education and government insurance) is paramount to improving neonatal and therefore infant mortality outcomes among those receiving fertility treatment.
Interestingly, odds of post-neonatal mortality were lower in the ART/NIFT group compared to spontaneously conceived infants. In the low SES group, we found a 40% reduction in the odds of post-neonatal mortality, while in the high SES group, odds reduced by 13%. We hypothesize that this difference in the reduction of odds of post-neonatal mortality may be attributed to better access to pre- and post-natal care by mothers in the low SES group receiving fertility treatment compared to those who had spontaneous conception, while access to such care is similar regardless of mode of conception in the high SES group.
Our findings reinforce data from prior studies that have demonstrated an association between SES and post-neonatal mortality [19, 20, 40]. Singh et al showed substantial neighborhood and individual socioeconomic disparities in post-neonatal mortality in the United States [19, 20]. They found that while overall post-neonatal mortality had declined over time, the disparities in post-neonatal mortality had widened with rates declining fastest in the “least socially deprived group”. A similar trend was seen for maternal education level. Other investigators have studied the effect of social policies such as Paid Family Leave on infant outcomes and have found a reduction in post-neonatal mortality rates after implementation of such policies [41], further suggesting post-neonatal mortality is associated more with socioeconomic factors than biological factors. One difference between the above studies and ours is that our study population comprises of
Regarding the etiology of post-neonatal mortality, the most common cause was SIDS regardless of mode of conception. However, SUID comprised 42.28% of post-neonatal deaths in the spontaneously conceived infants but only 18.52% in the ART/NIFT group. Previous studies have suggested an association between SES and SUID. In a systematic review, Spencer and Logan found a significant dose-response association between SUID and measures of socioeconomic status at both the individual and area level, with an increased risk of infant death increasing with greater social adversity [42]. This effect was found to be independent of other variables such as maternal smoking or infant birth weight. In New Zealand, Mitchell et al found a significant association of individual level socioeconomic factors with sudden infant death [43] and Shipstone et al identified that socially vulnerable families had higher number of risk factors for SUDI [44]. Our study also suggests that SES is associated with post-neonatal mortality, but the protective effect is not entirely explained by SES. Further studies are needed to identify other maternal, infant and biological factors [45] that protect ART/NIFT infants from SUID, and therefore post-neonatal mortality.
To our knowledge, this is the largest study of infant outcomes after fertility treatment, and the only one using a nationally representative sample in the US. Despite its strengths, it has limitations. First, we used a database with limited availability of clinical data such as reasons for infertility, previous infertility, fresh vs frozen embryo transfer, or use of donor oocytes. Second, use of fertility treatment is self-reported in the birth certificate and is vulnerable to recall bias and misclassification bias. However, the number of ART/NIFT births from 2014–2018 are similar to those reported by the CDC using data from all fertility clinics in the US for the same years [1, 46,47,48,49]. Third, we combined ART and NIFT as the single exposure variable of “fertility treatment” to obtain a sufficient sample size to detect meaningful differences in outcomes. However, in a supplementary analysis, we present our outcomes using 3 separate exposure groups—spontaneous conception, ART and NIFT groups – and trends of the results were consistent. Lastly, we used education and insurance to define SES. However, this definition does not directly account for other crucial factors such as family and social support, or environmental factors such as exposure to second-hand smoke and pollutants that might affect infant outcomes. Such factors may explain some of the residual differences in post-neonatal mortality we found in our study.
In conclusion, infants conceived via fertility treatment from low SES families are at higher risk of neonatal mortality and lower risk of post-neonatal mortality than spontaneously conceived infants. While medical efforts focused on preventing preterm birth and multiple gestation can help improve neonatal outcomes in these infants, socioeconomic policies and support for the most vulnerable families may help reduce infant mortality even further. While further studies are warranted to identify other maternal and infant factors contributing to lower rates of post-neonatal mortality, it remains imperative that further educational and public health efforts are put forth to attenuate the concerning reality of health disparities secondary to socioeconomic differences.
Data availability
We used the public use files provided by the Centers for Disease Control and Prevention (CDC). All data can be accessed via the following link: https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm.
Code availability
For the STATA code used to analyze the data, please email corresponding author, Meesha Sharma.
References
Sunderam S, Kissin DM, Zhang Y, Jewett A, Boulet SL, Warner L, et al. Assisted reproductive technology surveillance—United States, 2018. MMWR Surveill Summ. 2022;71:1–19.
Legro RS, Diamond MP, Coutifaris C, Schlaff WD, Alvero R, Casson P, et al. Pregnancy registry: three-year follow-up of children conceived from letrozole, clomiphene, or gonadotropins. Fertil Steril. 2020;113:1005–13.
Sanders JN, Simonsen SE, Porucznik CA, Hammoud AO, Smith KR, Stanford JB. Fertility treatments and the risk of preterm birth among women with subfertility: a linked-data retrospective cohort study. Reprod Health. 2022;19:83.
Luke B, Brown MB, Wantman E, Seifer DB, Sparks AT, Lin PC, et al. Risk of prematurity and infant morbidity and mortality by maternal fertility status and plurality. J Assist Reprod Genet. 2019;36:121–38.
Wennerholm UB, Bergh C. Perinatal outcome in children born after assisted reproductive technologies. Ups J Med Sci. 2020;125:158–66.
Declercq E, Luke B, Belanoff C, Cabral H, Diop H, Gopal D, et al. Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Fertil Steril. 2015;103:888–95.
von Wolff M, Haaf T. In vitro fertilization technology and child health. Dtsch Ärztebl Int. 2020;117:23–30.
Qin J, Sheng X, Wang H, Liang D, Tan H, Xia J. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch Gynecol Obstet. 2015;292:777–98.
Scherrer U, Rexhaj E, Allemann Y, Sartori C, Rimoldi SF. Cardiovascular dysfunction in children conceived by assisted reproductive technologies. Eur Heart J. 2015;36:1583–9.
Lu Yhong, Wang N, Jin F. Long-term follow-up of children conceived through assisted reproductive technology. J Zhejiang Univ Sci B. 2013;14:359–71.
Scherrer U, Rimoldi SF, Rexhaj E, Stuber T, Duplain H, Garcin S, et al. Systemic and pulmonary vascular dysfunction in children conceived by assisted reproductive technologies. Circulation. 2012;125:1890–6.
Rimoldi SF, Sartori C, Rexhaj E, Cerny D, Arx RV, Soria R, et al. Vascular dysfunction in children conceived by assisted reproductive technologies: underlying mechanisms and future implications. Swiss Med Wkly. 2014;144:w13973–w13973.
von Arx R, Allemann Y, Sartori C, Rexhaj E, Cerny D, de Marchi SF, et al. Right ventricular dysfunction in children and adolescents conceived by assisted reproductive technologies. J Appl Physiol. 2015;118:1200–6.
Meister TA, Rimoldi SF, Soria R, von AR, Messerli FH, Sartori C, et al. Association of assisted reproductive technologies with arterial hypertension during adolescence. J Am Coll Cardiol. 2018;72:1267–74.
Henningsen AA, Wennerholm UB, Gissler M, Romundstad LB, Nygren KG, Tiitinen A, et al. Risk of stillbirth and infant deaths after assisted reproductive technology: a Nordic study from the CoNARTaS† group. Hum Reprod. 2014;29:1090–6.
Gissler M, Silverio MM, Hemminki E. In-vitro fertilization pregnancies and perinatal health in Finland 1991–1993. Hum Reprod. 1995;10:1856–61.
Chughtai AA, Wang AY, Hilder L, Li Z, Lui K, Farquhar C, et al. Gestational age-specific perinatal mortality rates for assisted reproductive technology (ART) and other births. Hum Reprod. 2018;33:320–7.
Chung K, Coutifaris C, Chalian R, Lin K, Ratcliffe SJ, Castelbaum AJ, et al. Factors influencing adverse perinatal outcomes in pregnancies achieved through use of in vitro fertilization. Fertil Steril. 2006;86:1634–41.
Singh GK, Kogan MD. Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969–2001. Pediatrics. 2007;119:e928–39.
Singh GK, Yu SM. Infant mortality in the United States, 1915–2017: large social inequalities have persisted for over a century. Int J Matern Child Health AIDS. 2019;8:19–31.
Data and Statistics for SIDS and SUID | CDC [Internet]. 2023 [cited 2023 May 31]. Available from: https://www.cdc.gov/sids/data.htm.
Lavista Ferres JM, Anderson TM, Johnston R, Ramirez JM, Mitchell EA. Distinct populations of sudden unexpected infant death based on age. Pediatrics. 2020;145:e20191637.
Steurer MA, Peyvandi S, Costello JM, Moon-Grady AJ, Habib RH, Hill KD, et al. Association between Z-score for birth weight and postoperative outcomes in neonates and infants with congenital heart disease. J Thorac Cardiovasc Surg. 2021;162:1838–1847.e4.
Steurer MA, Schuhmacher K, Savla JJ, Banerjee M, Chanani NK, Eckhauser A, et al. Fetal growth and gestational age improve outcome predictions in neonatal heart surgery. J Thorac Cardiovasc Surg. 2022;164:2003–2012.e1.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Fenton TR, Sauve RS. Using the LMS method to calculate z-scores for the Fenton preterm infant growth chart. Eur J Clin Nutr. 2007;61:1380–5.
Luke B, Gopal D, Cabral H, Stern JE, Diop H. Pregnancy, birth, and infant outcomes by maternal fertility status: the Massachusetts Outcomes Study of Assisted Reproductive Technology. Am J Obstet Gynecol. 2017;217:327.e1–327.e14.
Rodriguez-Wallberg KA, Lundberg FE, Ekberg S, Johansson ALV, Ludvigsson JF, Almqvist C, et al. Mortality from infancy to adolescence in singleton children conceived from assisted reproductive techniques versus naturally conceived singletons in Sweden. Fertil Steril. 2020;113:524–32.
Chang J, Zhang Y, Boulet SL, Crawford SB, Copeland GE, Bernson D, et al. Assisted reproductive technology and perinatal mortality: selected states (2006–2011). Am J Perinatol. 2023;40:953–59.
Lisonkova S, Ukah UV, John S, Yearwood L, Muraca GM, Razaz N, et al. Racial and ethnic disparities in the perinatal health of infants conceived by ART. Pediatrics. 2022;150:e2021055855.
Fineman DC, Baer RJ, Chambers CD, Rajagopal S, Maltepe E, Rinaudo PF, et al. Outcomes of pulmonary vascular disease in infants conceived with non-IVF fertility treatment and assisted reproductive technologies at 1 year of age. Pediatr Pulmonol. 2019;54:1844–52.
Fineman DC, Keller RL, Maltepe E, Rinaudo PF, Steurer MA. Outcomes of very preterm infants conceived with assisted reproductive technologies. J Pediatr. 2021;236:47–53.e1.
Fineman DC, Keller RL, Maltepe E, Rinaudo PF, Steurer MA. Fertility treatment increases the risk of preterm birth independent of multiple gestations. FS Rep. 2023;4:313–20.
Ratnasiri AWG, Lakshminrusimha S, Dieckmann RA, Lee HC, Gould JB, Parry SS, et al. Maternal and infant predictors of infant mortality in California, 2007–2015. PLoS One. 2020;15:e0236877.
Smith LK, Manktelow BN, Draper ES, Springett A, Field DJ. Nature of socioeconomic inequalities in neonatal mortality: population based study. BMJ. 2010;341:c6654.
Lorenz JM, Ananth CV, Polin RA, D’Alton ME. Infant mortality in the United States. J Perinatol. 2016;36:797–801.
Comstock GW, Shah FK, Meyer MB, Abbey H. Low birth weight and neonatal mortality rate related to maternal smoking and socioeconomic status. Am J Obstet Gynecol. 1971;111:53–9.
De Neubourg D, Gerris J, Van Royen E, Mangelschots K, Vercruyssen M. Impact of a restriction in the number of embryos transferred on the multiple pregnancy rate. Eur J Obstet Gynecol Reprod Biol. 2006;124:212–5.
Li J, Shen J, Zhang X, Peng Y, Zhang Q, Hu L, et al. Risk factors associated with preterm birth after IVF/ICSI. Sci Rep. 2022;12:7944.
Joseph KS, Liston RM, Dodds L, Dahlgren L, Allen AC. Socioeconomic status and perinatal outcomes in a setting with universal access to essential health care services. Can Med Assoc J. 2007;177:583–90.
Montoya-Williams D, Passarella M, Lorch SA. The impact of paid family leave in the United States on birth outcomes and mortality in the first year of life. Health Serv Res. 2020;55:807–14.
Spencer N. Sudden unexpected death in infancy and socioeconomic status: a systematic review. J Epidemiol Community Health. 2004;58:366–73.
Mitchell EA, Stewart AW, Crampton P, Salmond C. Deprivation and sudden infant death syndrome. Soc Sci Med. 2000;51:147–50.
Shipstone RA, Young J, Kearney L, Thompson JMD. Applying a social exclusion framework to explore the relationship between sudden unexpected deaths in infancy (SUDI) and social vulnerability. Front Public Health. 2020;8:563573.
Kinney HC, Haynes RL. The serotonin brainstem hypothesis for the sudden infant death syndrome. J Neuropathol Exp Neurol. 2019;78:765–79.
Sunderam S. Assisted Reproductive Technology Surveillance—United States, 2014. MMWR Surveill Summ [Internet]. [cited 2023 May 21]. Available from: 66, 2017. https://www.cdc.gov/mmwr/volumes/66/ss/ss6606a1.htm.
Sunderam S. Assisted Reproductive Technology Surveillance — United States, 2015. MMWR Surveill Summ [Internet]. [cited 2023 May 21]. Available from:67, 2018. https://www.cdc.gov/mmwr/volumes/67/ss/ss6703a1.htm.
Sunderam S. Assisted Reproductive Technology Surveillance — United States, 2016. MMWR Surveill Summ [Internet]. [cited 2023 May 21]. Available from: 68, 2019. https://www.cdc.gov/mmwr/volumes/68/ss/ss6804a1.htm.
Sunderam S. Assisted Reproductive Technology Surveillance—United States, 2017. MMWR Surveill Summ [Internet]. [cited 2023 May 21]. Available from: 69, 2020. https://www.cdc.gov/mmwr/volumes/69/ss/ss6909a1.htm.
Acknowledgements
This work has not been previously published other than as an abstract for the Pediatric Academic Society 2023. The publicly available data used for this study was previously used by Fineman et al to study fertility treatment and preterm birth.
Author information
Authors and Affiliations
Contributions
MS designed the study, performed the analysis, interpreted the data, and wrote the manuscript. MAS designed the study, obtained the data, and drafted the manuscript. DCF drafted the manuscript and approved the final version. RLK interpreted the data, helped present the data, and drafted the manuscript. EM and PFR interpreted the data, drafted the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41372_2024_1866_MOESM2_ESM.docx
Supplementary Table 1: Crude and Adjusted Odds Ratios (aOR) of Mortality Among Infants Conceived by ART and NIFT Compared to Spontaneous Conception Stratified by SES
41372_2024_1866_MOESM3_ESM.docx
Supplementary Table 2: Crude and Adjusted Odds Ratios (aOR) of Mortality Among Infants Conceived with Fertility Treatment (ART/NIFT) Compared to Spontaneous Conception Stratified by Plurality
41372_2024_1866_MOESM4_ESM.pdf
Supplementary Fig. 1. Flow Diagram of Study Population Inclusion and Exclusion using CDC linked birth and death data files for 2014 – 2018
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharma, M., Fineman, D.C., Keller, R.L. et al. The effect of fertility treatment and socioeconomic status on neonatal and post-neonatal mortality in the United States. J Perinatol 44, 187–194 (2024). https://doi.org/10.1038/s41372-024-01866-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-01866-x