Abstract
Platelet transfusions are life-saving treatments for specific populations of neonates. However, recent evidence indicates that liberal prophylactic platelet transfusion practices cause harm to premature neonates. New efforts to better balance benefits and risks are leading to the adoption of more restrictive platelet transfusion guidelines in neonatal intensive care units (NICU). Although restrictive guidelines have the potential to improve outcomes, implementation barriers exist. We postulate that as neonatologists become more familiar with the data on the harm of liberal platelet transfusions, enthusiasm for restrictive guidelines will increase and barriers to implementation will decrease. Thus, we focused this educational review on; (1) the adverse effects of platelet transfusions to neonates, (2) awareness of platelet transfusion “refractoriness” in thrombocytopenic neonates and its association with poor outcomes, and (3) the impetus to find alternatives to transfusing platelets from adult donors to NICU patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380:242–51.
Fustolo-Gunnink SF, Fijnvandraat K, van Klaveren D, Stanworth SJ, Curley A, Onland W, et al. Preterm neonates benefit from low prophylactic platelet transfusion threshold despite varying risk of bleeding or death. Blood. 2019;134:2354–60.
Fustolo-Gunnink SF, Roehr CC, Lieberman L, Christensen RD, Van Der Bom JG, Dame C, et al. Platelet and red cell transfusions for neonates: lifesavers or Trojan horses? Expert Rev Hematol. 2019;12:797–800.
Moore CM, D’Amore A, Fustolo-Gunnink S, Hudson C, Newton A, Santamaria BL, et al. Two-year outcomes following a randomized platelet transfusion trial in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2023;108:452–7.
Rubin R. It takes an average of 17 years for evidence to change practice - the burgeoning field of implementation science seeks to speed things up. JAMA. 2023;329:1333–16.
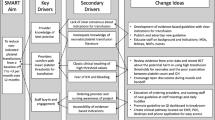
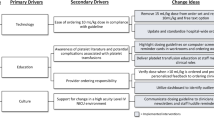
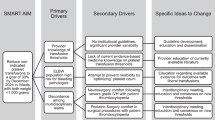
Davenport PE, Chan Yuen J, Briere J, Feldman HA, Sola-Visner MC, Leeman KT. Implementation of a neonatal platelet transfusion guideline to reduce non-indicated transfusions using a quality improvement framework. J Perinatol. 2021;41:1487–94.
Bahr TM, Christensen TR, Henry E, Astin M, Ilstrup SJ, Ohls RK, et al. Platelet transfusions in a multi-neonatal intensive care unit health care organization before and after publication of the PlaNeT-2 clinical trial. J Pediatr. 2023;257:113388.
Del Vecchio A, Sola MC, Theriaque DW, Hutson AD, Kao KJ, Wright D, et al. Platelet transfusions in the neonatal intensive care unit: factors predicting which patients will require multiple transfusions. Transfusion. 2001;41:803–8.
Baer VL, Lambert DK, Henry E, Snow GL, Sola-Visner MC, Christensen RD. Do platelet transfusions in the NICU adversely affect survival? Analysis of 1600 thrombocytopenic neonates in a multihospital healthcare system. J Perinatol. 2007;27:790–6.
Baer VL, Lambert DK, Henry E, Christensen RD. Severe thrombocytopenia in the NICU. Pediatrics. 2009;124:e1095–100.
Garcia MG, Duenas E, Sola MC, Hutson AD, Theriaque D, Christensen RD. Epidemiologic and outcome studies of patients who received platelet transfusions in the neonatal intensive care unit. J Perinatol. 2001;21:415–20.
Davenport PE, Wood TR, Heagerty PJ, Sola-Visner MC, Juul SE, Patel RM. Platelet transfusion and death or neurodevelopmental impairment in children born extremely preterm. JAMA Netw Open. 2024;7:e2352394.
Dohner ML, Wiedmeier SE, Stoddard RA, Null D Jr, Lambert DK, Burnett J, et al. Very high users of platelet transfusions in the neonatal intensive care unit. Transfusion 2009;49:869–72.
Bahr TM, Ohls RK, Ilstrup SJ, Christensen RD Neonatal intensive care unit patients receiving more than 25 platelet transfusions. Am J Perinatol. 2023. https://doi.org/10.1055/a-2073-3848
Sola-Visner MC. Platelet transfusions in neonates - less is more. N Engl J Med. 2019;380:287–8.
Hasan R, Saifee NH. Benefits of lower neonatal platelet transfusion thresholds. Transfusion. 2021;61:1672–5.
Davenport P, Sola-Visner M. Platelets in the neonate: Not just a small adult. Res Pr Thromb Haemost. 2022;6:e12719.
Maouia A, Rebetz J, Kapur R, Semple JW. The immune nature of platelets revisited. Transfus Med Rev. 2020;34:209–20.
Thom CS, Davenport P, Fazelinia H, Soule-Albridge E, Liu ZJ, Zhang H, et al. Quantitative label-free mass spectrometry reveals content and signaling differences between neonatal and adult platelets. J Thromb Haemost. 2024;22:1447–62.
Maurya P, Ture SK, Li C, Scheible KM, McGrath KE, Palsi J, et al. Transfusion of adult, but not neonatal, platelets promotes monocyte trafficking in neonatal mice. Arter Thrombo Vasc Biol. 2023;43:873–85.
Delaney C, Davizon-Castillo P, Allawzi A, Posey J, Gandjeva A, Neeves K, et al. Platelet activation contributes to hypoxia-induced inflammation. Am J Physiol Lung Cell Mol Physiol. 2021;320:L413–L421.
Bahr TM, Snow GL, Christensen TR, Davenport P, Henry E, Tweddell SM, et al. Can red blood cell and platelet transfusions have a pathogenic role in bronchopulmonary dysplasia? J Pediatr. 2024;265:113836.
Christensen RD, Bahr TM, Davenport P, Sola-Visner MC, Kelley WE, Ilstrup SJ, et al. Neonatal thrombocytopenia: factors associated with the platelet count increment following platelet transfusion. J Pediatr. 2023;263:113666 https://doi.org/10.1016/j.jpeds.2023.113666
Chen X, Zhao Y, Lv Y, Xie J. Immunological platelet transfusion refractoriness: current insights from mechanisms to therapeutics. Platelets. 2024;35:2306983.
Collection of platelets by automated methods. Guidance for industry and FDA review staff. US Department of Health and Human Services. Center for Biologics Evaluation and Research. December 2007; page 10.
Reese JA, Nguyen LP, Buchanan GR, Curtis BR, Terrell DR, Vesely SK, et al. Drug-induced thrombocytopenia in children. Pediatr Blood Cancer. 2013;60:1975–81.
George JN, Aster RH. Drug-induced thrombocytopenia: pathogenesis, evaluation, and management. Hematology Am Soc Hematol Educ Program. 2009:153-8. https://doi.org/10.1182/asheducation-2009.1.153
Sola-Visner M. Platelets in the neonatal period: developmental differences in platelet production, function, and hemostasis and the potential impact of therapies. Hematol Am Soc Hematol Educ Program. 2012;2012:506–11.
Ferrer-Marin F, Stanworth S, Josephson C, Sola-Visner M Distinct differences in platelet production and function between neonates and adults: implications for platelet transfusion practice. Transfusion. 2013;53:2814-21; quiz 2813.
Sparger KA, Assmann SF, Granger S, Winston A, Christensen RD, Widness JA, et al. Platelet transfusion practices among very-low-birth-weight infants. JAMA Pediatr. 2016;170:687–94.
Cremer M, Paetzold J, Schmalisch G, Hammer H, Loui A, Dame C, et al. Immature platelet fraction as novel laboratory parameter predicting the course of neonatal thrombocytopenia. Br J Haematol. 2009;144:619–21.
Cremer M, Weimann A, Schmalisch G, Hammer H, Bührer C, Dame C. Immature platelet values indicate impaired megakaryopoietic activity in neonatal early-onset thrombocytopenia. Thromb Haemost. 2010;103:1016–21.
MacQueen BC, Christensen RD, Henry E, Romrell AM, Pysher TJ, Bennett ST, et al. The immature platelet fraction: creating neonatal reference intervals and using these to categorize neonatal thrombocytopenias. J Perinatol. 2017;37:834–38.
Garofoli F, Ciardelli L, Angelini M, Gentile R, Mazzucchelli I, Tinelli C, et al. The role of immature platelet fraction (IPF%) in full-term and preterm infants: Italian data of a promising clinical biomarker in neonates. Int J Lab Hematol. 2020;42:e10–e13.
Takeshita S, Kakita H, Asai S, Asai T, Mori M, Ueda H, et al. Thrombocytopenia and insufficient thrombopoietin production in human small-for-gestational-age infants. Pediatr Res. 2023;93:619–24.
Arad ID, Alpan G, Sznajderman SD, Eldor A. The mean platelet volume (MPV) in the neonatal period. Am J Perinatol. 1986;3:1–3.
Patrick CH, Lazarchick J, Stubbs T, Pittard WB. Mean platelet volume and platelet distribution width in the neonate. Am J Pediatr Hematol Oncol. 1987;9:130–2.
Wiedmeier SE, Henry E, Sola-Visner MC, Christensen RD. Platelet reference ranges for neonates, defined using data from over 47,000 patients in a multihospital healthcare system. J Perinatol. 2009;29:130–6.
Catal F, Tayman C, Tonbul A, Akça H, Kara S, Tatli MM, et al. Mean platelet volume (MPV) may simply predict the severity of sepsis in preterm infants. Clin Lab. 2014;60:1193–200.
Wang J, Wang Z, Zhang M, Lou Z, Deng J, Li Q. Diagnostic value of mean platelet volume for neonatal sepsis: a systematic review and meta-analysis. Med (Baltim). 2020;99:e21649.
Ferrer-Marín F, Sola-Visner M. Neonatal platelet physiology and implications for transfusion. Platelets. 2022;33:14–22.
Andrew M, Castle V, Mitchell L, Paes B. Modified bleeding time in the infant. Am J Hematol. 1989;30:190–1.
Sola MC, del Vecchio A, Edwards TJ, Suttner D, Hutson AD, Christensen RD. The relationship between hematocrit and bleeding time in very low birth weight infants during the first week of life. J Perinatol. 2001;21:368–71.
Del Vecchio A, Latini G, Henry E, Christensen RD. Template bleeding times of 240 neonates born at 24 to 41 weeks gestation. J Perinatol. 2008;28:427–31.
Sheffield MJ, Schmutz N, Lambert DK, Henry E, Christensen RD. Ibuprofen lysine administration to neonates with a patent ductus arteriosus: effect on platelet plug formation assessed by in vivo and in vitro measurements. J Perinatol. 2009;29:39–43.
Sheffield MJ, Lambert DK, Henry E, Christensen RD. Effect of ampicillin on the bleeding time of neonatal intensive care unit patients. J Perinatol. 2010;30:527–30.
Saxonhouse MA, Garner R, Mammel L, Li Q, Muller KE, Greywoode J, et al. Closure times measured by the platelet function analyzer PFA-100 are longer in neonatal blood compared to cord blood samples. Neonatology. 2010;97:242–9.
Christensen RD, Sheffield MJ, Lambert DK, Baer VL. Effect of therapeutic hypothermia in neonates with hypoxic-ischemic encephalopathy on platelet function. Neonatology. 2012;101:91–4.
Deschmann E, Sola-Visner M, Saxonhouse MA. Primary hemostasis in neonates with thrombocytopenia. J Pediatr. 2014;164:167–72.
Valsami S, Kollia M, Mougiou V, Sokou R, Isaakidou E, Boutsikou M, et al. Evaluation of PFA-100 closure times in cord blood samples of healthy term and preterm neonates. Clin Chem Lab Med. 2020;58:e113–e6.
Deschmann E, Saxonhouse MA, Feldman HA, Norman M, Barbian M, Sola-Visner M. Association of bleeding scores and platelet transfusions with platelet counts and closure times in Response to adenosine diphosphate (CT-ADPs) among preterm neonates with thrombocytopenia. JAMA Netw Open. 2020;3:e203394.
Kollia M, Iacovidou N, Iliodromiti Z, Pouliakis A, Sokou R, Mougiou V, et al. Primary hemostasis in fetal growth restricted neonates studied via PFA-100 in cord blood samples. Front Pediatr. 2022;10:946932.
Rebulla P, Querol S, Pupella S, Prati D, Delgadillo J, De Angelis V. Recycling apparent waste into biologicals: the case of umbilical cord blood in Italy and Spain. Front Cell Dev Biol. 2022;9:812038.
Samarkanova D, Rodríguez L, Vives J, Coll R, Tahull E, Azqueta C, et al. Cord blood-derived platelet concentrates as starting material for new therapeutic blood components prepared in a public cord blood bank: from product development to clinical application. Blood Transfus. 2020;18:20816.
Rebulla P, Pupella S, Santodirocco M, Greppi N, Villanova I, Buzzi M, et al. Italian Cord Blood Platelet Gel Study Group. Multicentre standardisation of a clinical grade procedure for the preparation of allogeneic platelet concentrates from umbilical cord blood. Blood Transfus. 2016;14:73–9.
Samarkanova D, Codinach M, Montemurro T, Mykhailova L, Tancredi G, Gallerano P, et al. MultiCord12 Study Group. Multi-component cord blood banking: a proof-of-concept international exercise. Blood Transfus. 2023;21:526–37.
Christensen RD, Bahr TM, Christensen TR, Ohls RK, Krong J, Carlton LC, et al. Banked term umbilical cord blood to meet the packed red blood cell transfusion needs of extremely-low-gestational-age neonates: a feasibility analysis. J Perinatol. 2023. https://doi.org/10.1038/s41372-023-01833-y
Cortesi V, Cavallaro G, Raffaeli G, Ghirardello S, Mosca F, Klei TRL, et al. Why might cord blood be a better source of platelets for transfusion to neonates? Blood Transfus. 2024. https://doi.org/10.2450/BloodTransfus.566
Sim X, Poncz M, Gadue P, French DL. Understanding platelet generation from megakaryocytes: implications for in vitro-derived platelets. Blood. 2016;127:1227–33.
Di Buduo CA, Kaplan DL, Balduini A. In vitro generation of platelets: where do we stand? Transfus Clin Biol. 2017;24:273–6.
Strassel C, Gachet C, Lanza F. On the way to in vitro platelet production. Front Med (Lausanne). 2018;5:239.
Martínez-Botía P, Acebes-Huerta A, Seghatchian J, Gutiérrez L. On the quest for in vitro platelet production by re-tailoring the concepts of megakaryocyte differentiation. Med (Kaunas). 2020;56:671.
Liu H, Liu J, Wang L, Zhu F. In vitro generation of megakaryocytes and platelets. Front Cell Dev Biol. 2021;9:713434.
Kweon S, Kim S, Choi HS, Jo K, Park JM, Baek EJ. Current status of platelet manufacturing in 3D or bioreactors. Biotechnol Prog. 2023;39:e3364.
Izady E, Saltanatpour Z, Liu LP, Alizadeh A, Hamidieh AA. Toward in vitro production of platelets from induced pluripotent stem cells. Stem Cell Rev Rep. 2022;18:2376–87.
Tang A, Mendelson A. Recent lessons learned for ex-vivo platelet production. Curr Opin Hematol. 2021;28:424–30.
Thachil J, Salter I, George JN. Complete remission of refractory immune thrombocytopenia (ITP) with a short course of Romiplostim. Eur J Haematol. 2013;91:376–7.
Sparger KA, Ramsey H, Lorenz V, Liu ZJ, Feldman HA, Li N, et al. Developmental differences between newborn and adult mice in response to romiplostim. Platelets. 2018;29:365–72.
Neunert CE, Rose MJ. Romiplostim for the management of pediatric immune thrombocytopenia: drug development and current practice. Blood Adv. 2019;3:1907–191.
Mahat U, Talati R, Kodish E. Comment on: use of thrombopoietin receptor agonist (romiplostim) in neonatal autoimmune thrombocytopenia due to maternal immune thrombocytopenia. Pediatr Blood Cancer. 2019;66:e27706.
Kamitsuka MD, Patel S, Lee RT, Christensen RD. Romiplostim administration to a preterm neonate with severe prolonged acquired thrombocytopenia. Neonatol Today. 2021;16:10.
Rottenstreich A, Bussel JB. Treatment of immune thrombocytopenia during pregnancy with thrombopoietin receptor agonists. Br J Haematol. 2023;203:872–85.
Acknowledgements
We thank Jeni Walker, Division of Neonatology, University of Utah, for the illustration.
Author information
Authors and Affiliations
Contributions
RDC, TMB, PD, MCS-V, RKO, SJI and WEK; conception and design, assembly of data, manuscript writing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christensen, R.D., Bahr, T.M., Davenport, P. et al. Implementing evidence-based restrictive neonatal intensive care unit platelet transfusion guidelines. J Perinatol 44, 1394–1401 (2024). https://doi.org/10.1038/s41372-024-02050-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02050-x
This article is cited by
-
Three studies needed to inform the design of the U-BET (umbilical cord blood for extremely low-gestational-age transfusions) clinical trial
Journal of Perinatology (2026)
-
Using a lower platelet transfusion threshold: translating evidence into practice
Journal of Perinatology (2025)
-
Identifying barriers to complying with new restrictive NICU transfusion guidelines
Journal of Perinatology (2025)