Abstract
Objective
To investigate the association of maternal race/ethnicity with risk factors for brachial plexus birth injury (BPBI) and quantify the proportion of excess BPBI risk due to these factors.
Study design
This retrospective cohort study of all livebirths occurring in California-licensed hospitals from 1996–2012 included 6,278,562 maternal-livebirth infant pairs with 7762 BPBI diagnoses. Multiple logistic regression and causal mediation analyses were used to evaluate the relationship of race/ethnicity and BPBI risk factors.
Results
Black and Hispanic birthing-individuals were at increased risk of obesity, diabetes, and limited prenatal care utilization but decreased risk of many BPBI risk factors (shoulder dystocia, macrosomia, prolonged second stage of labor, and vaginal delivery).
Conclusions
Black and Hispanic birthing-individuals were at lower risk of many strongly associated risk factors for BPBI, and these factors mediate only a small proportion of their excess BPBI risk, underscoring the importance of identifying alternative risk factors, especially drivers of demographic disparities.
Similar content being viewed by others
Introduction
Brachial plexus birth injury (BPBI) is a traumatic injury to the nerve roots of the brachial plexus sustained by a newborn during labor and delivery believed to result from expulsive or traction forces on the brachial plexus nerve roots [1]. It presents as upper extremity weakness or paralysis and occurs in approximately 1.5 per 1000 livebirths [2,3,4]. Several risk factors for BPBI have been identified, including maternal factors (obesity, diabetes, gestational diabetes), infant factors (birthweight, macrosomia, post-date gestational age) and intrapartum factors (shoulder dystocia, instrumented delivery, vaginal delivery, prolonged labor, precipitous labor) [5].
Up to 30% of infants with BPBI have permanent nerve injuries [6,7,8,9,10], which result not only in persistent impairments in upper extremity motor and sensory function, but also the long term consequences of chronic denervation during skeletal immaturity, including impaired upper limb growth, joint contractures, and skeletal dysplasia [11, 12]. Many affected individuals experience lifelong disabilities in upper extremity and psychosocial function [13].
Demographic disparities in BPBI risk exist, with Black and Hispanic birthing individuals at increased risk of delivering an affected infant [3, 4, 14,15,16,17,18,19]. Compared to a population level incidence of 1.28 BPBI per 1000 livebirths, increased incidences of BPBI have been reported in Black and Hispanic infant deliveries, with 1.78 BPBI per 1000 livebirth among Black infants and 1.34 per 1000 per livebirth among Hispanic infants [4]. Moreover, Black and Hispanic birthing individuals mothers have an 88% and 35% increased odds of delivering an affected infant, respectively, when adjusting for known associations with BPBI, including shoulder dystocia, macrosomia, delivery method and year of birth [4]; because multiple studies have demonstrated decreasing incidence of BPBI in the late 1990s to early 2000s and relatively stable incidence thereafter [2,3,4, 20], it is important to adjust for year of birth in subsequent analyses. These racial and ethnic disparities have been replicated in populations with different demographic proportions [20] and alternative healthcare systems, including countries with nationalized healthcare systems [19], supporting the reproducibility of this disparity. However, the reasons for these demographic disparities are not well understood. In particular, the hypothesis that this disparity is due to increased risk of the known BPBI risk factors in these populations has not been confirmed. The purpose of this investigation was to evaluate if Black or Hispanic birthing individuals are at increased risk of the previously identified risk factors for BPBI, and to quantify how much of the excess risk of delivering an infant with BPBI is due to these factors.
Methods
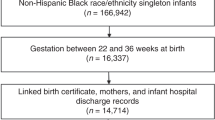
We obtained approval from the University of California Davis Institutional Review Board and the California Committee for the Protection of Human Subjects for this retrospective cohort study of all livebirth deliveries occurring in California-licensed hospitals from 1996–2012, the time period for which linked maternal-infant data is available. As described in previous work [4], the study cohort was assembled from the state of California’s Department of Health Care Access and Information (HCAI) Linked Birth Files, which includes linked maternal and infant demographic and health information for 9 months prior to and 12 months post-delivery for all infants born in a California-licensed hospital from 1991–2012; after 2012, the state of California was unable to continue performing this linkage. This accounts for 98% of California births during this time period [21]. The data are compiled by HCAI from the California Inpatient Discharge Dataset, Birth Certificate Dataset, and Vital Statistics Birth Cohort File. The dataset was created to facilitate research on pregnancy outcomes [21,22,23,24,25,26,27], and previous studies report its accuracy for maternal factors, intrapartum events, and obstetric complications [28,29,30].
All maternal-infant pairs with an infant ICD-9 code indicating “livebirth” during an inpatient admission (V30, V31, V33, V34, V36, V37, V39) were included. Single and multiple gestation births were included, as were cesarean and vaginal deliveries. Unlinked mothers or infants, stillbirth infants, and mothers under 13 and older than 50 years were excluded for reasons of biological implausibility. Maternal and infant demographic factors as reported on the discharge record and birth certificate: maternal age, infant sex, and race and ethnicity for both mother and infant. Missing maternal age at a given birth was imputed using the age at previous or subsequent births and the date of birth of the infant. Maternal age classified as young ( ≤ 19 years), reference (–20,34 years), or advanced ( ≥ 35 years). Missing or unknown ethnicity was imputed as ‘Non-Hispanic’ for both the mother and infant. We restricted the cohort to deliveries occurring from 1996-2012 because the coding of race and ethnicity changed in 1995 to permit more detailed demographic characterization and was not consistently applied until 1996.
Our primary cohorts of interest were maternal race (Black vs non-Black) and ethnicity (Hispanic vs non-Hispanic). The outcome variable for this study was infant diagnosis of BPBI, identified using ICD-9 codes (767.6 or 953.4). The mediators of interest included factors that have previously been associated with BPBI, all of which were available as variables in the dataset or using ICD-9 codes, including: maternal obesity, diabetes mellitus, gestational diabetes; Infant macrosomia (birthweight >4000 g), post-term delivery ( > 40 weeks 6 days gestational age); shoulder dystocia, vaginal delivery, precipitous labor, and prolonged second stage of labor. We evaluated 2 additional potential risk factors: prenatal care utilization and insurance status. Prenatal care utilization was determined using the Adequacy of Prenatal Care Utilization (APNCU) Index [31], which classifies prenatal care utilization (PNC) as Inadequate, Intermediate, Adequate or Adequate Plus. This variable is calculated using gestational age at birth, number of prenatal care visits, and month prenatal care began, which were available in the HCAI data. We defined limited prenatal care utilization (Limited PCU) as Inadequate or Intermediate prenatal care utilization according to the APNCU Index, and adequate prenatal care utilization (Adequate PCU) as adequate or adequate plus prenatal care utilization. The multiple insurance types in our dataset were also categorized into two groups, Adequately Insured or Under Insured. The adequately insured category included Private insurance, Medi-Cal (state insurance program), and Medi-Care, while the underinsured category was defined as Self-pay, Worker’s Compensation, Indigent Programs or Other).
Statistical analysis
Descriptive statistics were calculated for maternal and infant demographic factors and the known and suspected risk factors described above, including maternal obesity, diabetes, gestational diabetes, shoulder dystocia, macrosomia, vaginal delivery, post-term delivery, prolonged second stage of labor, precipitous labor, limited PCU, and underinsured. Multivariable logistic regression was used to determine the associations of BPBI with Black race and Hispanic ethnicity, controlling for maternal age, parity and year of infant birth; we controlled for these factors because they have been previously associated with BPBI [32] and therefore are important covariates to include in subsequent analyses to parse the effect of demographic factors on BPBI. In the race model, we additionally controlled for ethnicity, and in the ethnicity model we additionally controlled for race. Multivariable logistic regression was also used to determine the associations of Black race and Hispanic ethnicity with known or suspected risk factors for BPBI, controlling for maternal age, parity, year of infant birth, and either ethnicity or race as appropriate. Factors that increased the risk of BPBI and for which Blacks or Hispanics were at increased risk were considered potential mediators of the BPBI-race/ethnicity relationship and included in the causal mediation analysis of excess risk. Factors for which Black or Hispanic birthing individuals were at decreased risk were considered suppressors, as adjusting for these factors would increase the adjusted BPBI race/ethnicity disparity [33].
Causal mediation analysis [34, 35] was used to quantify the proportion of excess BPBI risk in Black and Hispanic birthing individuals that is explained by each of the potential mediators (factors for which Black and Hispanic birthing individuals were at increased risk). The mediators were coded so that the reference category was the “low-risk” category for each factor.
Causal mediation analysis provides estimates of the excess risk that is mediated or eliminated by each of the mediators. Percent excess BPBI risk mediated (“percent mediated”) by a particular factor is the proportion of the excess BPBI risk attributable to that factor; in essence, how important a particular mediator is in explaining the effect of the exposure (race/ethnicity) on the outcome (BPBI). Percent excess BPBI risk eliminated (“percent eliminated”) is the proportion of excess risk that would be resolved if an intervention made the effect of the mediator the same in each group and between-group differences in the effect of the risk factor were eliminated; in essence, if the effect of the factor was the same for Black and non-Black, or Hispanic and non-Hispanic individuals [36]. For simplicity of interpretation of the “percent mediated” effect sizes used to quantify our causal mediation analysis, we did not evaluate suppressors, as eliminating the effect of a suppressor would not reduce a disparity but instead increase it [33].
All statistical analysis was performed using SAS® software version 9.4 for Windows® (SAS Institute Inc, Cary, NC). Statistical code is available upon request. Significance was established at p < 0.05. While this data set contains multiple births to the same individual, the intra-cluster correlation was low and hence ignored [4].
Results
Our study population included 6,286,324 infants born to 4,104,825 individuals. 1,334,954 individuals contributed a single birth to the cohort and 2,769,871 contributed more than one birth. The mean number of infants per individual was 1.53 ± 0.83. BPBI was diagnosed in 7762 infants (1.23 BPBI per 1000 livebirths). Maternal and infant demographic characteristics are included in Table 1; the association of these demographic characteristics with BPBI has been published previously [4]. The distribution of known and suspected risk factors, stratified by race and ethnicity, is included in Table 2.
Association of race/ethnicity, and risk factors with BPBI (Table 3)
After adjusting for maternal age, parity, and infant year of birth, Black and Hispanic birthing individuals had a 53.9% (aOR = 1.539, 95% CI: 1.408, 1.682), and 19.5% (aOR = 1.195, 95% CI: 1.140, 1.252) increased odds of delivering a BPBI infant, respectively. All the examined factors, except underinsured, were significantly associated with BPBI .
Association of race and ethnicity with potential risk factors for BPBI (Table 4)
Compared to non-Black individuals, Black individuals had significantly increased odds of obesity and diabetes but decreased odds of many factors associated with BPBI, including gestational diabetes, shoulder dystocia, macrosomia, vaginal delivery, post-term delivery, prolonged second stage of labor, and precipitous labor. Black birthing individuals also had increased odds of limited PCU and being underinsured.
Hispanic individuals had significantly increased odds of obesity, diabetes, gestational diabetes, and post-term gestational age, but significantly decreased odds of shoulder dystocia, macrosomia, vaginal delivery, prolonged second stage of labor and precipitous labor. Compared to non-Hispanic individuals, Hispanic mothers had increased odds of limited PCU and being under insured .
Mediation analysis (Table 5)
In Black birthing individuals, the percent excess BPBI risk that is mediated by obesity, diabetes, and limited PCU is 8.77% (95% CI: 6.72, 10.83), 2.63% (95% CI: 1.92, 3.35), and 1.60% (95% CI: 0.89, 2.31), respectively. Among Hispanic birthing individuals, the percent excess BPBI risk mediated by obesity is 3.69% (95% CI: 2.61, 4.77), by diabetes is 5.18% (95% CI: 3.61, 6.75), by gestational diabetes is 7.69% (95% CI: 5.56, 9.81), by post-term delivery is 0.20% (95% CI: 0.09, 0.31), and by limited PCU is 4.80% (95% CI: 2.51, 7.10).
Discussion
Despite the well-documented racial and ethnic disparities in BPBI risk, a finding that has been reproduced across populations and healthcare systems [3, 4, 14,15,16,17,18,19], the factors contributing to these differences are not well understood. A first step in addressing these inequalities is to evaluate if the established risk factors for BPBI account for the increased risk in these populations. If so, we could target these factors for prevention efforts in high-risk populations and reduce demographic disparities. In this study we found that Black and Hispanic individuals were at lower risk of many of the strongest risk factors for BPBI, including shoulder dystocia, macrosomia, vaginal delivery, prolonged second stage of labor and precipitous labor.
The fact that Black and Hispanic individuals are at lower risk of many of the most strongly associated factors associated with BPBI indicates that the observed increased risk of BPBI in Black and Hispanic individuals is often an underestimation of the adjusted disparity. When included in multivariable regression analyses, factors that are less likely in Black and Hispanic individuals exert a suppression effect on the race-BPBI or ethnicity-BPBI relationship. Far from explaining the causes of the disparities, the association of race/ethnicity with BPBI is actually more pronounced than previously understood. Consequently, interventions such as simulation training in the management of shoulder dystocia, which are effective at reducing the incidence of shoulder dystocia and BPBI overall [37, 38], are unlikely to resolve disparities by race or ethnicity in BPBI risk. This finding demonstrates the need to identify alternative risk factors for BPBI contributing to these disparities.
Another notable finding of this study is that Black and Hispanic individuals were at higher risk of obesity and diabetes or gestational diabetes, but not shoulder dystocia or macrosomia. Traditionally, obesity and gestational diabetes are thought to increase the risk of BPBI via their association with macrosomia and subsequent shoulder dystocia, especially in the setting of fetopelvic disproportion. However, our finding, combined with other studies demonstrating BPBI in the absence of shoulder dystocia [39,40,41,42], suggests an alternative pathway for BPBI. Several previous investigations have proposed an in utero injury [39,40,41,42] or fetal malposition [43] as alternative mechanisms contributing to BPBI. Alternately, there may be a direct effect of hyperglycemia or other metabolic derangements on the brachial plexus’s development or susceptibility to injury, as has been shown in the central nervous system [44].
Our third finding is that limited prenatal care utilization (PCU) is associated with a 14% increased odds of BPBI, and that Black and Hispanic birthing individuals were 26% and 40% more likely to have limited PCU, a finding consistent with other studies [45, 46]. PCU is both identifiable prenatally and potentially modifiable, and therefore an ideal risk factor for BPBI, as this may be a more actionable risk factor than many intrapartum factors, such as shoulder dystocia. Although we did not have the ability to evaluate which components of prenatal care utilization are associated with decreased BPBI risk (e.g. diabetes management, fetal weight monitoring), this will be important to investigate in future studies.
Collectively, the above findings underscore the importance of identifying alternative risk factors for BPBI, especially those driving disparities. Although few studies have investigated the underlying causes of racial and ethnic disparities in BPBI risk, many studies have evaluated the factors contributing to demographic disparities in other adverse perinatal outcomes, including severe maternal morbidity, maternal mortality, maternal hemorrhage, neonatal morbidity and mortality, prematurity, low and very-low birth weight, intraventricular hemorrhage or necrotizing enterocolitis [47,48,49,50,51,52,53,54,55,56]. Factors associated with racial and ethnic disparities in these conditions include: hospital characteristics (obstetric volume [57,58,59], NICU level and volume [50], urban vs rural location, teaching status [51], racial diversity of work force [60]) [48, 50, 51, 53, 54, 56,57,58,59, 61,62,63], provider factors (provider delivery volume [64], racial concordance [65]), social determinants of health (insurance status, maternal education) [52, 66], and structural racism [67]. Interestingly, there is a tendency for higher risk racial and ethnic groups to deliver at poorer performing hospitals with higher risk-adjusted morbidity and mortality rates, conferring additional systems-level disadvantage, in addition to individual level risk factors [51, 53,54,55]. In addition to pregnancy and obstetric related factors discussed earlier, social determinants of health, provider level factors, and systems level factors such as hospital characteristics and healthcare workforce factors should be investigated for their association with BPBI, and may be viable targets for prevention at the individual, systems, or healthcare policy level. Because observed racial and ethnic disparities are likely reflective of historic social, cultural, and economic inequities, rather than differences in physiology and biology, it is possible that potential solutions for observed inequities lie in the social, culture, economic, and healthcare system domains, rather than exclusively in the biologic domain at the individual level.
Limitations of this study include the retrospective study design and limitations intrinsic to administrative datasets, including unmeasured confounding variables, missingness, and that the source files were created for medical billing and resource allocation. Some variables potentially relevant to BPBI risk (e.g. maternal weight gain, body mass index, medical comorbidities and estimated fetal weight) were not available. Other clinically relevant prenatal information, such as fetal ultrasound measurements or other biomarkers (e.g. hemoglobin A1c), were also not present in the dataset and, therefore, unable to be analyzed. Furthermore, the dataset lacked important social determinants of health, including socioeconomic status, that precluded analysis of these potential covariates. Our cohort included only infants diagnosed with BPBI at birth; infants with mild BPBI injuries not diagnosed at birth may not have been included. However, we believe the accuracy for this diagnosis in the dataset is likely very high, given that BPBI is most commonly diagnosed at birth, is not readily mistaken for another diagnoses, does not require confirmatory testing, and has unique ICD-9 codes. Another limitation is that our data set ends in 2012 because the state of California no longer performed the linkages between birthing individuals and infants needed for these analyses; however, analyses of more contemporary datasets, albeit with infant only data, indicate similar longitudinal trends in BPBI incidence beyond 2012 as those observed in this dataset [3, 4, 20].
Strengths of this study include the large size of the dataset, the diversity of maternal-infant pairs, its continuous coverage over a 17-year period, and demonstrated accuracy for obstetric complications and birth diagnoses [28,29,30]. The use of linked maternal-infant data improves upon studies using infant-only or maternal-only data which often do not provide sufficient information to evaluate the effect of maternal history or factors on infant conditions [68, 69]. Additionally, this dataset compiles data from several sources, which allows cross-checking accuracy among overlapping variables and broader coverage from non-overlapping variables.
In this study we found that despite being at increased risk of delivering an infant with BPBI, Black and Hispanic birthing individuals are at decreased risk of many of the strongest and most common risk factors for BPBI. Factors for which they are at increased risk account for a small proportion of the excess risk. To address the observed disparities, it is imperative to identify the factors driving these inequities and develop prevention strategies aimed at these factors. Given that race and ethnicity are constructs influenced by historic social, culture and economic factors, potential drivers of the observed disparities in BPBI include social, cultural, economic, and healthcare systems factors at both the individual and societal level that have been implicated in racial and ethnic inequalities observed in other adverse perinatal outcomes.
Data availability
The data that support the findings of this study are available from the California Department of Health Care Access and Information, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of California Department of Health Care Access and Information.
References
Obstetricians AC of, Gy. Neonatal Brachial Plexus Palsy. American College of Obstetricians and Gynecologists, Women’s Health Care Physicians; 2014. https://books.google.com/books?id=wbX9nwEACAAJ
Foad SL, Mehlman CT, Ying J. The epidemiology of neonatal brachial plexus palsy in the United States. J Bone Joint Surg Am. 2008;90:1258–64. https://doi.org/10.2106/JBJS.G.00853
DeFrancesco CJ, Shah DK, Rogers BH, Shah AS. The Epidemiology of Brachial Plexus Birth Palsy in the United States: Declining Incidence and Evolving Risk Factors. J Pediatr Orthop. 2019;39:e134–e140. https://doi.org/10.1097/BPO.0000000000001089
Manske MCB, Wilson MD, Wise BL, Melnikow J, Hedriana HL, James MA, et al. Maternal Epidemiology of Brachial Plexus Birth Injuries in California: 1996-2012. Am J Perinatol. Published online May 22, 2023. https://doi.org/10.1055/a-2097-1358
Gilbert WM, Nesbitt TS, Danielsen B. Associated factors in 1611 cases of brachial plexus injury. Obstet Gynecol. 1999;93:536–40. https://doi.org/10.1016/s0029-7844(98)00484-0
Hoeksma AF, ter Steeg AM, Nelissen RGHH, van Ouwerkerk WJR, Lankhorst GJ, de Jong BA. Neurological recovery in obstetric brachial plexus injuries: an historical cohort study. Dev Med Child Neurol. 2004;46:76–83. https://doi.org/10.1017/s0012162204000179
Pondaag W, Malessy MJA, van Dijk JG, Thomeer RTWM. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol. 2004;46:138–44. https://doi.org/10.1017/s0012162204000258
Foad SL, Mehlman CT, Foad MB, Lippert WC. Prognosis following neonatal brachial plexus palsy: an evidence-based review. J Child Orthop. 2009;3:459–63. https://doi.org/10.1007/s11832-009-0208-3
Annika J, Paul U, Anna-Lena L. Obstetric brachial plexus palsy - A prospective, population-based study of incidence, recovery and long-term residual impairment at 10 to 12 years of age. Eur J Paediatr Neurol EJPN J Eur Paediatr Neurol Soc. 2019;23:87–93. https://doi.org/10.1016/j.ejpn.2018.06.006
Lagerkvist AL, Johansson U, Johansson A, Bager B, Uvebrant P. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol. 2010;52:529–34. https://doi.org/10.1111/j.1469-8749.2009.03479.x
Hogendoorn S, van Overvest KLJ, Watt I, Duijsens AHB, Nelissen RGHH. Structural changes in muscle and glenohumeral joint deformity in neonatal brachial plexus palsy. J Bone Joint Surg Am. 2010;92:935–42. https://doi.org/10.2106/JBJS.I.00193
McDaid PJ, Kozin SH, Thoder JJ, Porter ST. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop. 2002;22:364–6.
Dorich JM, Whiting J, Plano Clark VL, Ittenbach RF, Cornwall R Impact of brachial plexus birth injury on health-related quality of life in adulthood: a mixed methods survey study. Disabil Rehabil. Published online May 18, 2023:1-14. https://doi.org/10.1080/09638288.2023.2212917
Merrison H, Mangtani A, Quick T. The shifting demographics of birth-related brachial plexus injury: The impact of socio-economic status and ethnic groups. J Plast Reconstr Aesthetic Surg JPRAS. 2021;74:560–8. https://doi.org/10.1016/j.bjps.2020.08.091
Cheng YW, Norwitz ER, Caughey AB. The relationship of fetal position and ethnicity with shoulder dystocia and birth injury. Am J Obstet Gynecol. 2006;195:856–62. https://doi.org/10.1016/j.ajog.2006.06.017
Lalka A, Gralla J, Sibbel SE Brachial Plexus Birth Injury: Epidemiology and Birth Weight Impact on Risk Factors. J Pediatr Orthop. Published online August 30, 2019. https://doi.org/10.1097/BPO.0000000000001447
Freeman MD, Goodyear SM, Leith WM. A multistate population-based analysis of linked maternal and neonatal discharge records to identify risk factors for neonatal brachial plexus injury. Int J Gynecol Obstet. 2017;136:331–6. https://doi.org/10.1002/ijgo.12059
Volpe KA, Snowden JM, Cheng YW, Caughey AB. Risk factors for brachial plexus injury in a large cohort with shoulder dystocia. Arch Gynecol Obstet. 2016;294:925–9. https://doi.org/10.1007/s00404-016-4067-0
Grahn P, Gissler M, Nietosvaara Y, Kaijomaa M. Ethnic background as a risk factor for permanent brachial plexus birth injury: A population-based study. Acta Obstet Gynecol Scand. 2024;103:1201–9. https://doi.org/10.1111/aogs.14817
DeFrancesco CJ, Mahon SJ, Desai VM, Pehnke M, Manske MC, Shah AS. Epidemiology of Brachial Plexus Birth Injury and the Impact of Cesarean Section on Its Incidence. J Pediatr Orthop. 2024. https://doi.org/10.1097/BPO.0000000000002800.
Danielsen BH, Carmichael SL, Gould JB, Lee HC. Linked birth cohort files for perinatal health research: California as a model for methodology and implementation. Ann Epidemiol. 2023;79:10–18. https://doi.org/10.1016/j.annepidem.2022.12.014
Gilbert WM, Danielsen B. Pregnancy outcomes associated with intrauterine growth restriction. Am J Obstet Gynecol. 2003;188:1596–9. https://doi.org/10.1067/mob.2003.384.
Glass HC, Pham TN, Danielsen B, Towner D, Glidden D, Wu YW. Antenatal and intrapartum risk factors for seizures in term newborns: a population-based study, California 1998-2002. J Pediatr. 2009;154:24–28.e1. https://doi.org/10.1016/j.jpeds.2008.07.008
Steurer MA, Jelliffe-Pawlowski LL, Baer RJ, Partridge JC, Rogers EE, Keller RL Persistent Pulmonary Hypertension of the Newborn in Late Preterm and Term Infants in California. Pediatrics. 2017;139. https://doi.org/10.1542/peds.2016-1165
Huang H, Woodruff TJ, Baer RJ, Bangia K, August KL, Jellife-Palowski LJ, et al. Investigation of association between environmental and socioeconomic factors and preterm birth in California. Environ Int. 2018;121:1066–78. https://doi.org/10.1016/j.envint.2018.07.027
Acosta CD, Knight M, Lee HC, Kurinczuk JJ, Gould JB, Lyndon A. The continuum of maternal sepsis severity: incidence and risk factors in a population-based cohort study. PloS One. 2013;8:e67175. https://doi.org/10.1371/journal.pone.0067175
Calthorpe LM, Baer RJ, Chambers BD, Steurer MA, Shannon MT, Oltman SP, et al. The association between preterm birth and postpartum mental healthcare utilization among California birthing people. Am J Obstet Gynecol MFM. 2021;3:100380 https://doi.org/10.1016/j.ajogmf.2021.100380
Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 2006;194:992–1001. https://doi.org/10.1016/j.ajog.2005.08.058
Romano PS, Yasmeen S, Schembri ME, Keyzer JM, Gilbert WM. Coding of perineal lacerations and other complications of obstetric care in hospital discharge data. Obstet Gynecol. 2005;106:717–25. https://doi.org/10.1097/01.AOG.0000179552.36108.6d
Tawfik DS, Gould JB, Profit J. Perinatal Risk Factors and Outcome Coding in Clinical and Administrative Databases. Pediatrics. 2019;143:e20181487 https://doi.org/10.1542/peds.2018-1487
Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994;84:1414–20.
Manske MC, Wilson MD, Wise BL, James MA, Melnikow J, Hedriana HL, et al. Association of Parity and Previous Birth Outcome With Brachial Plexus Birth Injury Risk. Obstet Gynecol. 2023;142:1217–25. https://doi.org/10.1097/AOG.0000000000005394
MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the Mediation, Confounding and Suppression Effect. Prev Sci J Soc Prev Res. 2000;1:173.
VanderWeele TJ. Mediation Analysis: A Practitioner’s Guide. Annu Rev Public Health. 2016;37:17–32. https://doi.org/10.1146/annurev-publhealth-032315-021402
VanderWeele T. Explanation in Causal Inference: Methods for Mediation and Interaction. Oxford University Press; 2015
VanderWeele TJ. Policy-relevant proportions for direct effects. Epidemiol Camb Mass. 2013;24:175–6. https://doi.org/10.1097/EDE.0b013e3182781410
Kaijomaa M, Gissler M, Äyräs O, Sten A, Grahn P. Impact of simulation training on the management of shoulder dystocia and incidence of permanent brachial plexus birth injury: An observational study. BJOG Int J Obstet Gynaecol. 2023;130:70–77. https://doi.org/10.1111/1471-0528.17278
Sienas LE, Hedriana HL, Wiesner S, Pelletreau B, Wilson MD, Shields LE. Decreased rates of shoulder dystocia and brachial plexus injury via an evidence-based practice bundle. Int J Gynaecol Obstet Organ Int Fed Gynaecol Obstet. 2017;136:162–7. https://doi.org/10.1002/ijgo.12034
Doumouchtsis SK, Arulkumaran S. Are all brachial plexus injuries caused by shoulder dystocia? Obstet Gynecol Surv. 2009;64:615–23. https://doi.org/10.1097/OGX.0b013e3181b27a3a
Allen RH, Gurewitsch ED. Temporary Erb-Duchenne Palsy Without Shoulder Dystocia or Traction to the Fetal Head. Obstet Gynecol. 2005;105:1210–2. https://doi.org/10.1097/01.AOG.0000141635.94905.21
Gherman RB, Goodwin TM, Ouzounian JG, Miller DA, Paul RH. Brachial plexus palsy associated with cesarean section: An in utero injury? Am J Obstet Gynecol. 1997;177:1162–4. https://doi.org/10.1016/S0002-9378(97)70034-6
Ouzounian JG, Korst LM, Phelan JP. Permanent Erb palsy: A traction-related injury? Obstet Gynecol. 1997;89:139–41. https://doi.org/10.1016/S0029-7844(96)00312-2
Louden E, Marcotte M, Mehlman C, Lippert W, Huang B, Paulson A Risk Factors for Brachial Plexus Birth Injury. Child Basel Switz. 2018;5. https://doi.org/10.3390/children5040046
Ornoy A, Ratzon N, Greenbaum C, Wolf A, Dulitzky M. School-age children born to diabetic mothers and to mothers with gestational diabetes exhibit a high rate of inattention and fine and gross motor impairment. J Pediatr Endocrinol Metab JPEM. 2001;14:681–9. https://doi.org/10.1515/jpem.2001.14.s1.681.
da Silva PHA, Aiquoc KM, da Silva Nunes AD, Medeiros WR, de Souza TA, Jerez-Roig J, et al. Prevalence of Access to Prenatal Care in the First Trimester of Pregnancy Among Black Women Compared to Other Races/Ethnicities: A Systematic Review and Meta-Analysis. Public Health Rev. 2022;43:1604400 https://doi.org/10.3389/phrs.2022.1604400.
Green TL. Unpacking Racial/Ethnic Disparities in Prenatal Care Use: The Role of Individual-, Household-, and Area-Level Characteristics. J Womens Health 2002. 2018;27:1124–34. https://doi.org/10.1089/jwh.2017.6807.
Mujahid MS, Kan P, Leonard SA, Hailu EM, Wall-Wieler E, Abrams B, et al. Birth hospital and racial and ethnic differences in severe maternal morbidity in the state of California. Am J Obstet Gynecol. 2021;224:219.e1–219.e15. https://doi.org/10.1016/j.ajog.2020.08.017
Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215:143–52. https://doi.org/10.1016/j.ajog.2016.05.007
Howell EA, Egorova NN, Janevic T, Brodman M, Balbierz A, Zeitlin J, et al. Race and Ethnicity, Medical Insurance, and Within-Hospital Severe Maternal Morbidity Disparities. Obstet Gynecol. 2020;135:285–93. https://doi.org/10.1097/AOG.0000000000003667
Jensen EA, Lorch SA. Effects of a Birth Hospital’s Neonatal Intensive Care Unit Level and Annual Volume of Very Low-Birth-Weight Infant Deliveries on Morbidity and Mortality. JAMA Pediatr. 2015;169:e151906 https://doi.org/10.1001/jamapediatrics.2015.1906
Burris HH, Passarella M, Handley SC, Srinivas SK, Lorch SA. Black-White disparities in maternal in-hospital mortality according to teaching and Black-serving hospital status. Am J Obstet Gynecol. 2021;225:83.e1–83.e9. https://doi.org/10.1016/j.ajog.2021.01.004
Lorch SA, Enlow E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr Res. 2016;79:141–7. https://doi.org/10.1038/pr.2015.199
Glazer KB, Zeitlin J, Egorova NN, Janevic T, Balbierz A, Hebert PL, et al. Hospital Quality of Care and Racial and Ethnic Disparities in Unexpected Newborn Complications. Pediatrics. 2021;148:e2020024091 https://doi.org/10.1542/peds.2020-024091
Howell EA, Janevic T, Blum J, Zeitlin J, Egorova NN, Balbierz A, et al. Double Disadvantage in Delivery Hospital for Black and Hispanic Women and High-Risk Infants. Matern Child Health J. 2020;24:687–93. https://doi.org/10.1007/s10995-020-02911-9
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in Morbidity and Mortality Rates in Black, White, and Hispanic Very Preterm Infants Among New York City Hospitals. JAMA Pediatr. 2018;172:269–77. https://doi.org/10.1001/jamapediatrics.2017.4402
Howell EA, Zeitlin J, Hebert PL, Balbierz A, Egorova N. Association between hospital-level obstetric quality indicators and maternal and neonatal morbidity. JAMA. 2014;312:1531–41. https://doi.org/10.1001/jama.2014.13381
Kozhimannil KB, Leonard SA, Handley SC, Passarella M, Main EK, Lorch SA, et al. Obstetric Volume and Severe Maternal Morbidity Among Low-Risk and Higher-Risk Patients Giving Birth at Rural and Urban US Hospitals. JAMA Health Forum. 2023;4:e232110 https://doi.org/10.1001/jamahealthforum.2023.2110
Walther F, Kuester D, Bieber A, Malzahn J, Rüdiger M, Schmitt J. Are birth outcomes in low risk birth cohorts related to hospital birth volumes? A systematic review. BMC Pregnancy Childbirth. 2021;21:531 https://doi.org/10.1186/s12884-021-03988-y
Snowden JM, Cheng YW, Kontgis CP, Caughey AB. The association between hospital obstetric volume and perinatal outcomes in California. Am J Obstet Gynecol. 2012;207:478.e1–7. https://doi.org/10.1016/j.ajog.2012.09.029
Guglielminotti J, Samari G, Friedman AM, Lee A, Landau R, Li G. Nurse workforce diversity and reduced risk of severe adverse maternal outcomes. Am J Obstet Gynecol MFM. 2022;4:100689 https://doi.org/10.1016/j.ajogmf.2022.100689
Campbell KH, Illuzzi JL, Lee HC, Lin H, Lipkind HS, Lundsberg LS, et al. Optimal maternal and neonatal outcomes and associated hospital characteristics. Birth Berkeley Calif. 2019;46:289–99. https://doi.org/10.1111/birt.12400
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N. Engl J Med. 2007;356:2165–75. https://doi.org/10.1056/NEJMsa065029
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8. https://doi.org/10.1542/peds.2011-2820
Janakiraman V, Lazar J, Joynt KE, Jha AK. Hospital volume, provider volume, and complications after childbirth in U.S. hospitals. Obstet Gynecol. 2011;118:521–7. https://doi.org/10.1097/AOG.0b013e31822a65e4
Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci USA. 2020;117:21194–21200. https://doi.org/10.1073/pnas.1913405117
Su D, Samson K, Hanson C, Anderson Berry AL, Li Y, Shi L, et al. Racial and ethnic disparities in birth Outcomes: A decomposition analysis of contributing factors. Prev Med Rep. 2021;23:101456 https://doi.org/10.1016/j.pmedr.2021.101456
Hailu EM, Maddali SR, Snowden JM, Carmichael SL, Mujahid MS. Structural racism and adverse maternal health outcomes: A systematic review. Health Place. 2022;78:102923 https://doi.org/10.1016/j.healthplace.2022.102923
Devlin HM, Desai J, Walaszek A. Reviewing performance of birth certificate and hospital discharge data to identify births complicated by maternal diabetes. Matern Child Health J. 2009;13:660–6. https://doi.org/10.1007/s10995-008-0390-9
Salemi JL, Tanner JP, Bailey M, Mbah AK, Salihu HM. Creation and evaluation of a multi-layered maternal and child health database for comparative effectiveness research. J Regist Manag. 2013;40:14–28.
Acknowledgements
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
MCM conceived the study idea, contributed to the study design and interpretation of the analyses, and wrote the manuscript. MDW and DJT contributed to the study idea, developed the study design, conducted the analyses, contributed to the interpretation of the results and reviewed and contributed to the manuscript. BLW contributed to the study idea, interpretation of the results and the manuscript. HLH and JM reviewed and contributed to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The University of California Davis Institutional Review Board determined that this study was not human subjects research. The study protocol was approved by the State of California Committee for the Protection of Human Subjects (Project Number 2018-167). The analysis of existing data was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manske, M.C., Wilson, M.D., Wise, B.L. et al. Are racial and ethnic disparities in brachial plexus birth injuries explained by known risk factors?. J Perinatol 45, 790–796 (2025). https://doi.org/10.1038/s41372-025-02239-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02239-8