Abstract
Objective
Assess the efficacy of routine ETCOc for all newborns in managing neonatal hyperbilirubinemia.
Study design
Retrospective chart review of 1029 consecutive well-baby nursery admissions following the 2022 AAP hyperbilirubinemia guidelines. Only ETCOc, not type, Rh, and DAT, was used to determine if significant hemolysis was present in sufficient degree to affect bilirubin management. A cost-benefit analysis comparing the two methods was conducted.
Result
2.8% of infants required phototherapy, and 1.1% were readmitted for hyperbilirubinemia. The closer an infant’s bilirubin level was to the phototherapy threshold, the higher the ETCOc. 12 of 29 DAT negative infants with ETCOc ≥ 2.5 PPM who received phototherapy would have gone home with significant hemolysis at risk for readmission or kernicterus if not for the use of ETCOc.
Conclusion
ETCOc is preferable for assessing significant hemolysis in the newborn, can be used to safely manage newborn hyperbilirubinemia, and results in cost savings.
Similar content being viewed by others
Introduction
Hyperbilirubinemia is a common condition in newborns [1]. Hemolysis has been recognized as a risk factor for severe hyperbilirubinemia since at least 1932 [2], and algorithms adjusting phototherapy levels based on the presence of hemolysis have been in use since at least 1970 [3]. The American Academy of Pediatrics (AAP) has recognized significant hemolysis to be a risk factor for bilirubin induced neurological damage, and has provided specific recommendations for lowering the threshold for initiating phototherapy if significant hemolysis is present starting in 2004 [4].
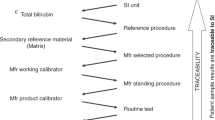
End tidal carbon monoxide corrected for ambient carbon monoxide (ETCOc) has been recommended as a method to determine degree of hemolysis since 2004 [4]. Until recently, however, that method was not easily performed in a clinical setting. In its place, direct antibody test (DAT) screening has been widely used to assess the presence of hemolysis, primarily due to its universal availability and rapid turn-around time. However, multiple studies have shown that DAT+ is often not associated with significant hemolysis and did not predict the severity of neonatal hyperbilirubinemia [5,6,7]. ETCOc is a much more specific measure of hemolysis, and it can now be easily and non-invasively measured via Capnia’s CoSense ETCO monitor (CoSense, Capnia, Redwood City, CA, USA) on an infant’s exhaled breath.
Our unit first began using ETCOc to determine hemolysis as part of a large, multi-center study evaluating the Capnia CoSense monitor [8]. Following that study, we continued to test infants who were either DAT+ or in the high-intermediate risk or high-risk zone of the Bhutani nomogram [9]. With the initiation of the 2022 AAP guidelines [10], and having seen that significant hemolysis was usually not present in supposedly high risk infants [9], we decided to evaluate a cohort of consecutive admissions to the well-baby nursery for the presence of significant hemolysis using ETCOc and compare their need for phototherapy and readmission with the common risk factor of DAT + .
Subjects and methods
Data was collected from 1094 consecutive admissions to the well-baby nursery of Einstein Medical Center Philadelphia from 8/9/2023 to 3/21/2024. Based on standard unit protocols, blood type, Rh, and DAT testing was performed on cord blood collected on all babies whose mothers were either type O or Rh negative. A CBC and reticulocyte count was performed on all infants with A/B/O incompatibility. An ETCOc level was collected on each infant, usually in the mother’s post-partum room, at the time of the infant’s hearing screening. The device used was the Capnia CoSense monitor. The device was approved by the FDA in 2014, and multiple studies since have shown it to meet the standards required to detect hemolysis in infants [11]. Although the device might not be able to obtain a level at times due to a rapid respiratory rate or elevated H+ level [12], ultimately, we were able to obtain an ETCOc level on all infants in the study. An ETCOc level ≥ 2.5 PPM was considered evidence of significant hemolysis, as this was the 95% for infants from our unit in a previous multi-center study [8]. In the current study, criteria for bilirubin management were based on the AAP guidelines in place at the time of the infants’ birth [10], and an ETCOc level ≥ 2.5 PPM was used as the criterion for significant hemolysis as opposed to DAT + . Follow-up for hyperbilirubinemia after discharge was based on the findings of Kuzniewicz et al. [13]. Infants who required admission to the neonatal intensive care unit either before or after admission to the well-baby nursery, except only for the provision of phototherapy, were removed, leaving a total of 1029 infants to be part of the study.
Demographic data was collected, and an analysis of the need for phototherapy using either DAT or ETCOc as the criterion for hemolysis was conducted. A cost-benefit analysis comparing the two methods was also performed. This study was approved by the institutional review board (Approval # 2023-1055).
Results
The demographics of the study population are noted in Table 1. Of the 1094 infants initially admitted to the nursery, 65 were removed from the final results as they had spent a portion of their birth hospitalization in the neonatal intensive care unit (NICU) for various reasons. Of the remaining 1029 infants, 29 underwent phototherapy in the NICU, had no other indications for NICU admission, and are the subject of this report. A total of 1000 infants remained in the well-baby nursery for the entirety of their birth hospitalization (Fig. 1). Of the 1029 infants studied, 29 (2.8%) required phototherapy during their initial birth hospitalization, and 11 of 1029 (1.1%) required readmission for phototherapy after their initial discharge. Only one infant who required phototherapy during their birth hospitalization was subsequently readmitted for phototherapy. The breakdown of the group by sex, gestational age, and race or ethnicity is presented in Table 1. A total of 30 (2.9%) infants were DAT positive. A total of 48 (4.7%) were G6PD positive based on their state mandated newborn screen. Since the newborn screen results were generally not available until approximately one week after birth, the G6PD results were not used as a criterion for significant hemolysis. The average age at ETCOc collection was 32.5 ± 8.7 h (Table 2). Table 2 also presents ETCOc levels stratified by the need for phototherapy or readmission, race or ethnicity, mg/dL below phototherapy of the discharge bilirubin, and relationship of DAT positive to ETCOc. A cost/benefit analysis is presented in Table 3. A total of 7 fewer infants received phototherapy using ETCOc as opposed to DAT+ as a marker of significant hemolysis, and 5 fewer infants were readmitted for phototherapy by using ETCOc instead of DAT + . The costs for laboratory studies were provided by the hospital’s lab supervisor, and the room and board costs were provided by the hospital’s financial department. We assumed a 2-day increased length of stay for either phototherapy during the initial birth hospitalization or readmission. We also assumed two serum bilirubin tests for each additional day. The mothers of 447 infants were O+ and 116 infants had A/B/O incompatibility with their mothers. The analysis revealed a savings of $13,123.00 for the entire group by using ETCOc instead of DAT+ to determine significant hemolysis.
Discussion
Recently, Christensen et al. [11] published a paper describing ETCOc as the gold standard for determining hemolysis in newborns. Multiple studies have found that many DAT+ infants are in fact not hemolyzing when assessed by either ETCOc or carboxyhemoglobin levels [5,6,7]. A total of 30 (2.9%) infants in this study were DAT+ (Table 2E), and only 7 (23.3%) showed evidence of significant hemolysis. This incidence of significant hemolysis is similar to prior cohorts from our institution when either ETCOc [7] or COHbg [6] were used as a measure of hemolysis. More concerning is the fact that 84/999 (8.4%) infants in this study who were either DAT negative, or did not have their DAT evaluated, in fact had significant hemolysis with ETCOc levels ≥2.5 PPM (Table 2E).
ETCOc is a simple, non-invasive test that can be used to safely manage newborn hyperbilirubinemia with no additional staff time required. In this study, ETCOc levels were measured by unit staff during performance of the hearing screen. While waiting for the hearing screening device to complete a test, there was plenty of time to determine the infant’s ETCOc level. ETCOc levels have been shown to be relatively stable during the first three days of an infant’s life [14], so each post-partum unit can determine how best to fit the test into their routine.
In this study, using the 2022 AAP guidelines and ETCOc as a measure of hemolysis, 2.8% of the infants required phototherapy, and only 1.1% of the cohort were readmitted. This is substantially better than the levels found by Cahill, et al. [15] when they compared their incidence of phototherapy and readmission using the 2004 and 2022 AAP guidelines, and similar to the results of Sarathy et al. [16] who also used the 2022 guidelines. ETCOc levels were identical between those in our entire group and those who were neither readmitted nor underwent phototherapy (1.7 ± 0.5 PPM vs. 1.7 ± 0.5 PPM, respectively). It was higher for those infants requiring phototherapy as compared to those who did not, and, not surprisingly, the closer an infant’s bilirubin level was to their phototherapy level, the higher their ETCOc (Table 2A and 2D, respectively). Infants who were readmitted had ETCOc levels intermediate between those who required phototherapy and the cohort of all infants (Table 2A).
The ETCO levels among the different races and ethnicities in our cohort were quite similar ranging from 1.7 ± 0.5–1.8 ± 0.5 PPM, with 2 standard deviations above the mean ranging from 2.7–2.8 PPM. Different mean ETCOc levels have been found among various cohorts of infants. In a group of Chinese infants [14], 95% was found to be 2.2 PPM. Christensen et al. [17] found the 95% to be 1.7 PPM in a primarily Caucasian population. Similarly, there are various recommendations regarding what level to use as significant hemolysis. While we used 2.5 PPM, Bilitool (Bilitool.org) uses a cutoff of 1.7 PPM which is the 75% noted by Bao et al. [14]. Since each site will have a population with somewhat different ETCOc values, a trial period to determine mean ETCOc levels, and at which percentile the unit feels comfortable determining significant hemolysis, should be implemented before beginning to use ETCOc as the marker of hemolysis.
In 2021 Kuzniewicz et al. [13] reviewed close to 150,000 infants born in the Northern California Kaiser Permanente system. They determined how many mg/dl their discharge bilirubin was below the appropriate phototherapy level and then determined the rate of readmission for each 1 mg cohort. They recommended 24-h follow up for a discharge bilirubin 0–2 mg/dL below the phototherapy level, follow-up in 48 h for a bilirubin level 2–3 mg below the phototherapy level, and clinical follow-up alone for a discharge bilirubin more than 3 mg/dL below the phototherapy level. They reviewed their data again after publication of the 2022 AAP guidelines and found their recommendations still held [18]. In order to be conservative, infants in this study had routine follow-up at 24 h after discharge for a bilirubin less than 3 mg/dL below phototherapy levels, 48-h follow-up for a bilirubin 3–5 mg/dL below phototherapy level, and clinical follow-up alone for a bilirubin more than 5 mg/dL below phototherapy levels. Of the 1000 infants who did not require phototherapy, 21 (2.1%) had a discharge bilirubin <3 mg/dL below the phototherapy level, and 118 (11.8%) had a discharge bilirubin between 3 and 5 mg/dL below their phototherapy level. Thus only 13.9% of our infants required follow-up after discharge which is similar to Kuzniewicz et al. [13] and substantially fewer than the 60% of infants requiring some reevaluation using the Bhutani nomogram [9]. Unsurprisingly, ETCOc levels were higher the closer the discharge bilirubin level was to the phototherapy level (Table 2D). Using their nomogram, Kuzniewicz et al. [13] had a readmission rate of 0.3% for infants whose discharge bilirubin was more than 5.5 mg/dL below phototherapy level. In our study, 2 of 1029 infants were readmitted with a discharge bilirubin >5 mg/dL below phototherapy (0.2%) which is comparable to the results of Kuzniewicz et al. [13].
As noted above (Table 3), by using ETCOc instead of DAT+ to determine the presence of significant hemolysis, a total of $13 123.00 could be saved for this group of 1029 newborns. The major source of savings was the ability to eliminate the type, RH, and DAT on infants whose mothers were type O+ and the room and board savings for the 12 fewer infants who would either not require phototherapy or would not be readmitted. Another source of savings, or more properly a lack of increased cost, occurred by performing ETCOc at the time of the newborn’s hearing screen. Using this method resulted in no additional time spent by any hospital staff to obtain the results. Potentially the most important source of savings is decreasing the risk of sending infants home with significant hemolysis who were not identified. In this study, 12/29 (41.4%) of the infants requiring phototherapy were either DAT negative or did not have their DAT measured. A total of 84 of the 999 (8.4%) infants in the entire group who were either DAT negative or did not have their DAT measured had significant hemolysis (ETCOc ≥2.5 PPM). These infants have an increased risk of significant hyperbilirubinemia, and potentially kernicterus, that might not be picked up until significant neurological damage has occurred. Unfortunately, the current legal system in the United States does not function well to accurately determine true medical malpractice. One of the authors (DLS) has served as a defense expert in 2 malpractice cases where there was no evidence of malpractice [19, 20]. However, the plaintiffs presented the two children with significant neurological deficits during their trials. In one case [19], the jury awarded the plaintiff a judgment in excess of $100,000,000, and in the other case [20], the parties reached a multimillion-dollar settlement. Since the awards in kernicterus cases run between 10 and 50 million dollars [21], avoiding one case of kernicterus would pay for nasal cannulas to perform ETCOcs on the newborns in our institution for 125 years.
In summary, ETCOc is a simple, non-invasive test that is the current gold standard for determining hemolysis in a newborn [11]. By using ETCOc instead of DAT+ to determine hemolysis, fewer infants will require phototherapy during their birth hospitalization, and fewer infants will be readmitted to the hospital for phototherapy after their initial discharge. In addition to the health benefits to these infants and families, there would be monetary savings to the hospitals, and potentially the avoidance of cases of kernicterus and all of its disastrous consequences.
Data availability
Data can be obtained on appropriate request from the corresponding author.
References
Qattea I, Farghaly MAA, Elgendy M, Mohamed MA, Aly H. Neonatal hyperbilirubinemia and bilirubin neurotoxicity in hospitalized neonates: Analysis of the US database. Pediatr Res. 2022;91:1662–8.
Diamond LK, Blackfan KD, Baty JM. Erythroblastosis fetalis and its association with universal edema of the fetus, icterus gravis neonatorum and anemia of the newborn. J Pediatr. 1932;1:269–76. https://doi.org/10.1016/S0022-3476(32)80057-0
Odell GB, Poland RL, Ostrea EM. Neonatal Hyperbilirubinemia. In Klaus MH and Fanaroff AA Care of the High-Risk Newborn. WB Saunders: Philadelphia,1973;1973:197.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.
Herschel M, Karison T, Wen M, Caldarelli L, Baron B. Isoimmunization is unlikely to be the cause of hemolysis in ABO-incompatible but direct antiglobulin test -negative neonates. Pediatrics. 2002;110:127–30.
Schutzman DL, Gatien E, Ajayi S, Wong RJ. Carboxyhemogobin levels as a predictor of risk for significant hyperbilirubinemia in African-American DAT+ infants. J Perinatol. 2016;36:386–8.
Elsaie AL, Taleb M, Nicosia A, Zangaladze A, Pease ME, Newton K, et al. Comparison of end-tidal carbon monoxide measurements with direct antiglobulin tests in the management of neonatal hyperbilirubinemia. J Perinatol. 2020;40:1513–7.
Bhutani VK, Maisels MJ, Schutzman DL, Castillo Cuadrado ME, Aby JL, Bogen DL, et al. Identification of risk for neonatal hemolysis. Acta Paediatr. 2018;107:1350–6.
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103:6–14.
Kemper AR, Newman TB, Slaughter JL, Maisels MJ, Watchko JF. Clinical practice guideline revision: Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2022;150:e2022058859.
Christensen RD, Bahr TM, Wong RJ, Vreman HJ, Bhutani VK, Stevenson DK. A “gold standard” test for diagnosing and quantifying hemolysis in neonates and infants. J Perinatol. 2023;43:1541–7.
Bahr TM, Shakib JH, Stipelman CH, Kawamoto K, Lauer S, Christensen RD. Improvement initiative: End-tidal carbon monoxide measurement in newborns receiving phototherapy. J Pediatr. 2021;238:168–173.e2.
Kuzniewicz MW, Park J, Niki H, Walsh EM, McCulloch CE, Newman TB. Predicting the need for phototherapy after discharge. Pediatrics. 2021;147:e2020019778.
Bao Y, Zhu J, Ma L, Zhang H, Sun L, Xu C, et al. An end-tidal carbon monoxoide nomogram for term and late preterm Chinese newborns. J Pediatr. 2022;250:16–21.
Cahill C, Jegatheesean P, Song D, Cortes M, Adams A, Narasimhan SR, et al. Implementing higher phototherapy thresholds for jaundice in healthy infants 35 plus weeks. Hosp Pediatr. 2023;13:857–64.
Sarathy L, Chou JH, Romano-Clarke GR, Darci KA, Lerou PH. Bilirubin measurement and phototherapy use after the AAP 2022 newborn hyperbilirubinemia guidelines. Pediatrics. 2024;153:e2023063323.
Christensen RD, Lambert DK, Henry E, Yaish HM, Prchal JT. End-tidal carbon monoxide as an indicator of the hemolytic rate. Blood Cells Mol Diseases. 2015;54:292–6.
Kuzniewicz MW, Li SX, McCulloch CE, Newman TB. Predicting the need for phototherapy after discharge: Update for 2022 phototherapy guidelines. Pediatrics. 2022;150:19–21.
Hagans v Hospital of the University of Pennsylvania in the Court of Common Pleas in Philadelphia County.
Gordon v Reading Hospital in the Court of Common Pleas of Philadelphia County. Case ID#210501208.
Acknowledgements
The authors would like to thank the staff of the post-partum unit for collecting ETCOc levels on the infants in this study.
Author information
Authors and Affiliations
Contributions
SW participated in writing and editing the manuscript, collecting data, and reviewing and approving the completed manuscript. RB participated in collecting data and reviewing and approving the completed manuscript. KN participated in collecting data and reviewing and approving the completed manuscript. DLS conceived the project, participated in writing and editing the manuscript, collecting data, and reviewing and approving the completed manuscript.
Corresponding author
Ethics declarations
Competing interests
None of the authors has any conflicts of interest to disclose. Dr. Schutzman is an unpaid member of the medical advisory board of Capnia, Inc. The nasal cannulas used in this study were provided by Capnia at no charge. At no point did any member of Capnia have input into the formulation, performance, or data interpretation of this study.
Ethics
This study was approved by the Institutional Review Board of Einstein Medical Center (Approval # 2023-1055). The need for informed consent was waived by the IRB. This study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wells, S., Balasubramanian, R., Nguyen, K. et al. End-tidal carbon monoxide for routine monitoring of significant hemolysis in the management of newborn hyperbilirubinemia. J Perinatol 45, 957–960 (2025). https://doi.org/10.1038/s41372-025-02242-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02242-z
This article is cited by
-
The prediction of phototherapy by early postnatal ETCOc in Chinese newborns
BMC Pediatrics (2025)
-
Hemolysis and dat positivity
Journal of Perinatology (2025)