Abstract
Neonatal hypoglycemia is the most common metabolic disorder in newborns and can lead to neurological damage if untreated. While intravenous dextrose is the standard treatment, it is invasive. Oral 40% dextrose gel (0.5 ml/kg) offers a non-invasive alternative. A systematic review of five randomized controlled trials (RCTs), involving 2,742 neonates (1,326 received dextrose gel; 1,416 received placebo), assessed its effectiveness in reducing NICU admissions in neonates with blood glucose < 2.6 mmol/L. Although the overall meta-analysis showed a non-significant reduction in NICU admissions (risk ratio 0.68; 95% CI: 0.33–1.38; p = 0.28), a sensitivity analysis excluding one outlier study improved consistency (I² = 19%) and revealed a statistically significant reduction (risk ratio 0.52; 95% CI: 0.31–0.90; p = 0.02). These findings suggest that oral dextrose gel may reduce NICU admissions in neonates with hypoglycemia, but further large-scale studies are required to confirm its clinical effectiveness.
Similar content being viewed by others
Introduction
During gestation, glucose serves as a primary metabolic fuel of the fetus, and its concentration plays a crucial role in optimal brain development and function, disruption of which can lead to adverse effects in the fetal brain [1, 2]. Neonatal hypoglycemia, defined as a reduction in blood glucose concentration in neonates, is a common metabolic disturbance in glucose homeostasis affecting up to 15% of all newborns and occurs in up to 50% of those with risk factors such as prematurity, maternal diabetes, or abnormal birthweight (either high or low) [2]. A study in rural Kerala found that the incidence of hypoglycemia was highest in the first 24 h after birth, with exclusively breastfed babies showing lower rates (10.5%) compared to formula-fed infants (33.3%) [3]. A systematic review revealed that approximately 26.3% of infants are eligible for neonatal hypoglycemia screening, with this proportion remaining relatively stable over a 15-year period [4].
During pregnancy, the fetus derives glucose from the mother via transplacental transfer, which occurs through a concentration gradient and facilitated diffusion [5, 6]. However, during birth once the umbilical cord is clamped, the glucose supply from mother to the newborn is interrupted which leads to a drop in glucose concentration within 1–2 h of birth. This period is very critical for newborn before initiation of postnatal metabolic adaptation, ultimately contributing to development of neonatal hypoglycemia. Hypoglycemia in neonates can be a transient or persistent type, and is associated with several adverse effects such as tachycardia, temperature irregularities, respiratory distress and neuroglycopenic signs including seizure, coma, cyanotic episodes, and apnoea [7]. Clinically, undetected low interstitial glucose concentrations were linked to greater neurodevelopmental problems too between age of 6 and 11 years, visual-motor impairment and executive dysfunction at 4-5 years, and a two-fold increased risk for literacy skills [8, 9].
The definition of hypoglycemia in neonates remains complex and controversial due to the variability of normal blood glucose concentration, which can differ based on gestational age, birth weight, and the time elapsed since birth [10]. Notably, there is currently no universally accepted or standardized guideline for the diagnostic threshold of neonatal hypoglycemia, and the criteria used vary across different studies and clinical guidelines. Several authors have proposed operational thresholds based on gestational maturity. In preterm and low-birth-weight neonates, hypoglycemia has been defined as a whole blood glucose concentration of less than 20 mg/dL (1.1 mmol/L). For term neonates, hypoglycemia is often defined as a concentration of less than 30 mg/dL (1.5 mmol/L) during the first 72 h of life, and less than 40 mg/dL (2.2 mmol/L) thereafter [11]. Over the decades, the accepted threshold for hypoglycemia in neonates has evolved. In the 1960s, it is as low as 20 mg/dL considered acceptable. This threshold increased to approximately 40 mg/dL during the 1970s, and by 1988, many neonatologists had adopted 47 mg/dL (2.6 mmol/L) as the lower limit of acceptable blood glucose concentration [12]. Despite these evolving benchmarks, many experts still continue to cite the concentration of approximately 40 mg/dL (2.2 mmol/L) as the lower physiological limit during the first day of life [13].
For newborn, the first hour after birth is often referred to as the “golden hour,” a critical period for ensuring optimal health outcomes [14, 15]. In cases of neonatal hypoglycemia, it is essential to maintain blood glucose concentration within an acceptable range in this hour to minimize the risk of brain injury [16]. The initial management typically involves feeding the infant with breast milk or an appropriate infant formula. However, when blood glucose concentration fall critically low ranging between 18 and 25 mg/dL (1.0–1.4 mmol/L) intravenous dextrose administration is recommended. This usually entails a bolus of 200 mg/kg, followed by a continuous infusion at a rate of 4-8 mg/kg per minute, adjusted based on the infant’s response and glucose monitoring [17, 18]. However, in this situation, the infants should be admitted to the NICU, which involves time, expense, invasiveness and separation of the infant from the mother. This causes distress to the mother and interferes with breastfeeding initiation.
For the quick and affordable treatment of hypoglycemia in neonates, oral dextrose gel at 200 mg/kg (40% dextrose equivalent to 0.5 ml/kg) combined with breastfeeding is highly recommended as the first line of treatment [19, 20]. Oral dextrose gel acts by direct absorption of glucose through the mucous membranes, providing a rapid increase in blood glucose levels. Additionally, any portion of the gel that is swallowed is absorbed through the gastrointestinal tract, offering a sustained release of glucose into the bloodstream. This dual absorption mechanism, buccal and gastrointestinal ensures both immediate and prolonged stabilization of blood sugar levels in neonates [21]. Several studies have investigated the efficacy of oral dextrose gel in managing neonatal hypoglycemia and showed that dextrose gel significantly reduced the need for intravenous fluids in the neonates and supporting continued breastfeeding and minimizing mother-infant separation, and contributing to overall better outcomes for newborn [22]. Further, it also has the prophylactic potential to reduce the risk of hypoglycemia in at-risk infants too [23].
Though the existing studies suggest that oral dextrose gel can effectively reduce the incidence of neonatal hypoglycemia, its impact on broader clinical outcomes, such as NICU admissions, remains uncertain according to few authors [24]. Considering the available evidence, a systematic review is imperative to comprehensively assess the effectiveness of oral dextrose gel as a first-line treatment for neonatal hypoglycemia. Therefore, this review aims to address existing knowledge gaps for its use in clinical practice through a systematic assessment of the existing literature.
Materials and methods
Review question
The systematic review protocol was registered with PROSPERO (CRD42023467289) and were conducted in accordance with the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines to answer the following research question: “Is oral dextrose gel more effective than placebo in preventing hypoglycemia in neonates?”
Inclusion and exclusion criteria
The eligibility criteria based on the following PICOS characteristics were considered
-
Population (P): Subject with neonatal hypoglycemia
-
Intervention (I): Buccal dextrose gel used for treatment
-
Comparison (C): Placebo or breastfeeding
-
Outcomes (O): Proportion of neonates admitted to NICU or variations in the blood glucose concentration
-
Study design (S): Experimental trial (RCT)
Original studies meeting the “Subjects, Intervention, Comparison, Outcome” (PICO) criteria were considered eligible for inclusion. During the intervention at a dose of 0.5 ml/kg of 40% buccal dextrose gel to treat neonatal hypoglycemia reported in the study group and compared with the placebo or breastfeeding for improvement in their glycaemic status were considered. Further, studies used glucose oxidase method for assessing blood glucose in infants with hypoglycemia followed by admission to NICU were considered for meta-analysis. Ex-vivo cell studies and case reports or case series were excluded.
Search strategy
Two independent researchers (S.S and G.S) performed electronic searches through four databases: MEDLINE (PubMed), Web of Science, Scopus, and Embase to retrieve published relevant articles from 2010 to March 2023. Additional searches through google scholar was conducted to find any missing studies. Studies published in English were only included in this review. A summary of the search strategy for each database is given in Table 1.
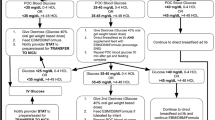
Screening of articles
Duplicates were removed after collating articles collected from various databases showing similarities in title, author, and year of publication. The title and abstract were independently screened by two authors (S.S and G.S), articles that did not meet the specified PICO criteria were excluded. Any disagreements in selection of articles were resolved by discussion and consultation with a third author (L.P). Full-text of eligible articles were retrieved and screened individually by two authors (S.S and G.S) and the disagreement was resolved via discussion. The study protocol is shown in Fig. 1.
Data extraction
For studies that fulfilled the eligibility criteria, data were extracted using standardized extraction form including: (a) author and year, (b) study location, (c) study type, (d) sample size, (e) study group, (f) control group, (g) primary outcome, (h) cut-off for considering hypoglycemia, (i) evaluation method, (j) results, (k) significance, and (l) inference. Background characteristics and outcome measures of the included studies are given in the Table 2 and Table 3 respectively. The primary outcome focused was the proportion of neonates admitted to the NICU for hypoglycemia, treated with oral dextrose gel or placebo.
Risk of bias assessment
The studies were assessed the Risk of Bias (ROB) using the revised Joanna Briggs Institute (JBI) critical appraisal checklist for randomized controlled trials [25] by two independent review authors (S.S and G.S), and the disagreement among them was resolved by the third reviewer (L.P).
Effect measures and statistical analysis
Data extracted from the included studies were entered into Microsoft Excel 2016. The number of subjects admitted to the NICU for hypoglycemia was considered for analysis. Comprehensive Meta-Analysis software version 3.0 (Biostat Inc., USA) was used for analysis of the outcomes [26]. Data from the RCTs were used in the meta-analysis to estimate the risk ratio and 95% confidence interval comparing the study group with a placebo. A random effect model was chosen due to expected heterogeneity between the RTCs. Statistical heterogeneity was assessed using I2 index, and a value greater than 50% was assumed as significant variations [27]. Potential publication bias was assessed using Egger’s test and visualized through a funnel plot. Statistical significance was set at p < 0.05. The GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach was adopted to analyze the certainty of evidence using the online software GRADEpro GDT (https://gradepro.org/) [28].
Results
Description of study characteristics
Five articles with similar outcomes finally were included in this systematic review (Table 2) [23, 29,30,31,32]. The number of included neonates in each trial ranged from 100 to 2129, with all studies following randomized clinical trial design, except one study by Coors et al. [29], which followed Quasi-Experimental design. The blood glucose concentration of <2.6 mmol/L ( < 47 mg/dl) served as the cut-off for defining hypoglycemia necessitating NICU admission. Studies reported that the primary risk factor for neonatal hypoglycemia was infant of diabetic mother, late preterm (35 or 36-weeks’ gestation), small (birth weight <2500 g) or large for gestational age (birth weight >4500 g). There was a statistically significant difference between the dextrose gel and placebo groups in the number of newborns admitted to the NICU due to hypoglycemia in all investigations except two studies (p > 0.05) [23, 29].
A study by Harris et al., 2017 [30] was not included in the meta-analysis due to lack of similarity in the outcome measures, where they examined blood glucose variations. Finally, a total of 2742 participants from the four included trials were included in the quantitative evidence syntheses.
Effectiveness of oral dextrose gel
Figure 2 illustrates the forest plot of four randomized controlled trials assessing the effectiveness of oral dextrose gel in reducing NICU admissions among neonates with hypoglycemia. The overall pooled risk ratio was 0.68 (95% CI: 0.33 to 1.38; p = 0.28), suggesting a lower likelihood of NICU admission in the dextrose gel group compared to the placebo or comparator group. However, the result did not reach statistical significance. Notably, the study by Harding et al. [23], contributed the greatest weight (34.4%) and reported a the effect size favoring the comparator, which may have attenuated the overall effect. Moreover, substantial heterogeneity was observed among the studies (I² = 76%), indicating variability that could impact the reliability of the pooled estimate. Despite the wide confidence interval, the direction of effect across most studies suggests potential utility of oral dextrose gel usage in reducing NICU admissions.
Sensitivity analysis
Figure 3 presents the results of a sensitivity analysis performed by excluding the study by Harding et al. [23], in order to reduce the heterogeneity observed in the initial analysis. After its removal, the revised meta-analysis included three studies and demonstrated a statistically significant reduction in the risk of NICU admission among neonates treated with oral dextrose gel, with a pooled risk ratio of 0.52 (95% CI: 0.31 to 0.90; p = 0.02). Additionally, heterogeneity was markedly reduced (I² = 19%), indicating a more consistent effect across the remaining studies in favoring dextrose gel in reducing NICU admission when compared to placebo gel.
Risk of bias
The following sections are taken for risk of bias analysis in the included studies: (a) Selection bias: sequence generation and allocation concealment, (b) Performance bias: blinding, (c) Detection bias: blinding of outcome assessors, (d) Attrition bias: incomplete outcome data, (e) Reporting bias, and (f) Other potential biases [25]. The risk of bias in each study was categorized as “high risk”, “low risk “ or “unclear” in each of these domains. Notably, a study by Harris et al. [31], consistently demonstrated low risk across all evaluated criteria. Similarly, two studies exhibited low risk of bias across all domains and unclear bias in the outcomes showing multiple outcome measures [23, 32]. The remaining two studies showed significant performance in bias assessment [29, 30]. Consequently, the overall risk of bias across was low to moderate in all included studies (Table 4). These findings confirm the reliability of the study results and support their suitability for analysis and interpretation.
Publication bias
Funnel plots generated to assess publication bias and heterogeneity between studies. Examination of the funnel plot indicated a mild asymmetry without any obvious sign of publication bias within the included studies. One of the four studies [23] was beyond the cluster of studies in the funnel plot, indicating its potential role as the main source of heterogeneity. This outlier has significantly higher relative weight, complicating the possibility of excluding it from the analysis. Despite this outlier, Egger’s regression test for funnel plot asymmetry yielded an intercept of -3.19 (95% CI: -6.06 to -0.33) with a t-value of -2.183 and a p-value of 0.161. As the p-value exceeds 0.05, there is no statistically significant evidence of publication bias. Thus, both visual and statistical assessments suggest minimal risk of reporting bias in the included studies. In the absence of publication bias, the study strengthens the reliability of the findings (Fig. 4).
Certainty of evidence
Grades of evidence indicate the strength and valuable of evidence based on how thoroughly the study was conducted. Considering the certainty assessment parameters like inconsistency, indirectness, imprecision, risk of bias and other factors [28] the summary of evidence with five randomized controlled trials infers the conclusion of high certainty towards the generated evidence (Table 5).
Discussion
The present review focuses on the management of neonatal hypoglycemia, a common disturbance in glucose homeostasis in newborns. Among the various treatment options, oral dextrose gel therapy has emerged as one of the most conservative and effective approaches for mitigating hypoglycemia in neonates. Alternative therapies, such as intravenous dextrose administration, often necessitate admission to a neonatal intensive care unit (NICU). This requirement can result in the physical separation of the newborn from the mother, potentially disrupting breastfeeding and bonding. The use of oral dextrose gel aligns with a more conservative treatment strategy, as highlighted in this review, preserving the opportunity for maternal-infant interaction while addressing this critical metabolic emergency [30]. Our review summarizes studies demonstrating the efficacy of oral dextrose gel versus placebo or other management for neonatal hypoglycemia. Of the five trials, one study [30] was excluded from the pool of quantitative evidence synthesis due to significant variability in the reporting outcomes. Nonetheless, the results of the present review revealed a notable finding: administering dextrose gel led to a significant increase in blood glucose concentration by 3.3 mg/dL compared to infants who did not receive breast milk or other form [30]. Of the four studies analyzed [23, 29, 31, 32], two demonstrated significant differences favoring dextrose gel over placebo in reducing neonatal intensive care unit (NICU) admissions for hypoglycemia [31, 32], while the remaining two did not [23, 29].
Among the studies yielding insignificant results, one study [29], with a relative weight of 25.62%, reported NICU admissions in 7 out of 72 neonates (9.7%) in the prophylactic group compared to 24 out of 164 neonates (14.6%) in the control group. Despite these observations, caution is essential when interpreting these findings due to inherent limitations in the study design. Firstly, the study employed a quasi-experimental methodology without randomized allocation of participants, which may have introduced selection bias. Secondly, the dextrose gel formulation used in this study, Insta-Glucose, contained 77% carbohydrate (including dextrose, dextrins, and maltose), differing from other dextrose gel formulations. This composition may have triggered a hyperinsulinemic response, potentially attenuating the expected therapeutic benefits. Additionally, the study utilized a glucometer based on the glucose dehydrogenase method, which is known for reduced precision and sensitivity at lower glucose concentrations compared to the plasma glucose oxidase method, the gold standard for glucose measurement. These methodological constraints necessitate cautious interpretation of the reported outcomes.
The second study [23], which also showed insignificant results, revealed that prophylactic administration of dextrose gel at a dose of 200 mg/kg failed to reduce NICU admissions among at-risk neonates. However, it did demonstrate a reduction in the incidence of hypoglycemic episodes. Several factors may account for this apparent discrepancy. Notably, 81% of the participants were infants born to mothers with diabetes, which could limit the external validity and generalizability of the findings. Furthermore, 16.5% of glucose measurements in this study were performed using a less reliable analyzer, potentially introducing variability and affecting the accuracy of the results.
A positive effect of using oral dextrose gel with a 32% reduction in NICU admission for neonatal hypoglycemia was observed in this systematic review. Further, these results were supported by the findings of Walravens et al. [33], where they showed a sustained reduction in number of interventions by incorporating buccal dextrose gel in late preterm and term infants. Similarly, Parappil et al. [21] examined the effectiveness of dextrose gel supplementation in treating asymptomatic neonatal hypoglycemia, and found a 13.1% improvement in neonatal discharges and significant reduction in NICU admission (3.5%) and intravenous dextrose therapy (5.2%).
Similar beneficial effects of oral dextrose gel were shown in various studies [24, 34,35,36,37,38,39]. Meneghin and their group showed asymptomatic hypoglycaemic neonates treated with 40% oral dextrose gel had very lower rate of NICU transfers (10%) compared to the controlled group (48.7%) [36]. According to Rawat et al. [37], 74% of asymptomatic hypoglycaemic infants had increased blood glucose concentration after receiving three doses of dextrose gel with feeds, compared to 58% after receiving feeds alone. Similar observations were found in a retrospective study by Gregory et al. [40] they highlighted the therapeutic potential of dextrose gel treatment for hypoglycaemic neonatal condition by decreasing the need of intravenous dextrose administration. In addition, this approach has several benefits, including cost-effectiveness and life-saving treatment strategy. Further, this approach helps in mitigating adverse neuro developmental outcomes in neonates at the community concentration [41].
Limitation
The study provides valuable new insights into the effectiveness of oral dextrose gel in controlling neonatal hypoglycemia. However, there are some limitations such as the relatively small number of included studies with different study designs and methodologies, which leads to heterogeneity among the studies and limit the generalizability of the findings. Despite these limitations, buccal dextrose gel application remains a promising option providing a cost-effective approach without any apparent adverse effects, suggesting its potentials for treating neonates at risk of hypoglycemia. Further investigations are necessary to confirm these results in different populations and also to optimize dosing as it is a first-line treatment option.
Clinical implication
Follow-up data from the clinical trials have shown that treatment with dextrose gel is not only effective in the short term but also safe in the long term. At two years of age, no significant differences were observed in neurosensory impairment, cognitive processing, or other developmental outcomes between infants treated with dextrose gel and those receiving placebo [35, 42]. Clinically, dextrose gel has been shown to significantly reduce the need for neonatal intensive care unit (NICU) admissions, with a number needed to treat (NNT) of just 8 to prevent one NICU admission. This has profound implications for promoting mother-infant bonding, supporting exclusive breastfeeding, and reducing healthcare costs. Moreover, fewer infants required formula feeding in the dextrose gel group at two weeks of age, underscoring its role in facilitating breastfeeding continuity. The treatment has demonstrated excellent tolerability with no associated adverse effects, reinforcing its safety profile. Given its ease of administration, cost-effectiveness, and moderate evidence of long term benefit without any reported adverse effect, oral dextrose gel should be considered a first-line, non-invasive intervention for managing neonatal hypoglycemia in both clinical and community settings.
Conclusion
Our comprehensive meta-analysis highlights the significant effectiveness of oral dextrose gel as an affordable and minimally invasive therapy for neonatal hypoglycemia. Further, our results demonstrated its effectiveness in reducing invasive procedures and hypoglycaemic episodes. In addition to its clinical efficacy, oral dextrose gel therapy promotes breastfeeding and strengthens the bond between mothers and infants. The use of oral dextrose gel has potential benefits in improving health outcomes in newborns, and provides a practical solution for clinicians and caregivers.
Data availability
Data are available upon reasonable request.
References
Hay WW Jr, Raju TN, Higgins RD, Kalhan SC, Devaskar SU. Knowledge Gaps and Research Needs for Understanding and Treating Neonatal Hypoglycemia: Workshop Report from Eunice Kennedy Shriver National Institute of Child Health and Human Development. J Pediatr. 2009;155:612–7.
Harris DL, Weston PJ, Harding JE. Incidence of Neonatal Hypoglycemia in Babies Identified as at Risk. J Pediatr. 2012;161:787–91.
Pillai SK, Fhausiya VK. A cross-sectional study on the frequency and risk factors for neonatal hypoglycemia in babies born in rural Kerala. J Fam Med Prim Care. 2022;11:6949–54.
O’Brien M, Gilchrist C, Sadler L, Hegarty JE, Alsweiler JM. Infants eligible for neonatal hypoglycemia screening: a systematic review. JAMA Pediatr. 2023;177:1187–96.
Schneider H, Reiber W, Sager R, Malek A. Asymmetrical transport of glucose across the in vitro perfused human placenta. Placenta. 2003;24:27–33.
Holme AM, Roland MC, Lorentzen B, Michelsen TM, Henriksen T. Placental glucose transfer: a human in vivo study. PLoS ONE. 2015;10:e0117084.
Boluyt N, van Kempen A, Offringa M. Neurodevelopment after neonatal hypoglycemia: a systematic review and design of an optimal future study. Pediatrics. 2006;117:2231–43.
Shah R, Harding J, Brown J, McKinlay C. Neonatal glycaemia and neurodevelopmental outcomes: a systematic review and meta-analysis. Neonatology. 2019;115:116–26.
McKinlay CJ, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, et al. Association of Neonatal Glycemia With Neurodevelopmental Outcomes at 4.5 Years. JAMA Pediatr. 2017;171:972–83.
Vain NE, Chiarelli F. Neonatal Hypoglycaemia: A Never-Ending Story? Neonatology. 2021;118:522–29.
Cornblath M, Ichord R. Hypoglycemia in the neonate. Semin Perinatol. 2000;24:136–49.
Sinclair JC. Approaches to the definition of neonatal hypoglycemia. Acta Paediatr Jpn. 1997;39:S17–20.
Neczypor JL, Holley SL. Providing evidence-based care during the golden hour. Nurs Women’s Health. 2017;21:462–72.
Sharma D. Golden 60 min of newborn’s life: Part 1: Preterm neonate. J Matern Fetal Neonatal Med. 2017;30:2716–27.
Harding JE, Harris D, Hegarty JE, Alsweiler JM, McKinlay CJD. An emerging evidence base for the management of neonatal hypoglycaemia. Early Hum Dev. 2017;104:51–6.
Levene I, Wilkinson D. Identification and management of neonatal hypoglycaemia in the full-term infant (British Association of Perinatal Medicine—Framework for Practice). Arch Dis Child Educ Pract Ed 2019;104:29–32.
Adamkin DH, Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127:575–9.
Rozance PJ, Wolfsdorf JI. Hypoglycemia in the newborn. Pediatr Clin North Am. 2019;66:333–42.
Weston PJ, Harris DL, Harding JE. Dextrose gel treatment does not impair subsequent feeding. Arch Dis Child Fetal Neonatal Ed. 2017;102:539–41.
Edwards T, Liu G, Battin M, Harris DL, Hegarty JE, Weston PJ, et al. Oral dextrose gel for the treatment of hypoglycaemia in newborn infants. Cochrane Database Syst Rev. 2022;3:CD011027.
Gupta K, Amboiram P, Balakrishnan U, Abiramalatha T, Devi U. Dextrose gel for neonates at risk with asymptomatic hypoglycemia: a randomized clinical trial. Pediatrics. 2022;149:e2021050733.
Harding JE, Hegarty JE, Crowther CA, Edlin RP, Gamble GD, Alsweiler JM. hPOD Study Group. Evaluation of oral dextrose gel for prevention of neonatal hypoglycemia (hPOD): A multicenter, double-blind randomized controlled trial. PLoS Med. 2021;18:e1003411.
Chandrasekharan P, Lakshminrusimha S. Single dose of prophylactic oral dextrose gel reduces neonatal hypoglycaemia. BMJ Evid Based Med. 2017;22:62.
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Systematic reviews of effectiveness. Joanna Briggs Inst reviewer’s Man. 2017;19:3 https://reviewersmanual.joannabriggs.org/ (accessed 20 May 2024).
Comprehensive Meta-Analysis Version 3.0Borenstein, M Hedges, L Higgins, J Rothstein, H Biostat, Englewood, NJ (2022).
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Methods Med. 2002;21:1539–58.
GRADE handbook, https://gdt.gradepro.org/app/handbook/handbook.html (accessed 20 May 2024).
Coors SM, Cousin JJ, Hagan JL, Kaiser JR. Prophylactic dextrose gel does not prevent neonatal hypoglycemia: a quasi-experimental pilot study. J Pediatr. 2018;198:156–61.
Harris DL, Gamble GD, Weston PJ, Harding JE. What Happens to Blood Glucose Concentrations After Oral Treatment for Neonatal Hypoglycemia? J Pediatr. 2017;190:136–41.
Harris DL, Weston PJ, Signal M, Chase JG, Harding JE. Dextrose gel for neonatal hypoglycaemia (the Sugar Babies Study): A randomised, double-blind, placebo-controlled trial. Lancet. 2013;382:2077–83.
Hegarty JE, Harding JE, Gamble GD, Crowther CA, Edlin R, Alsweiler JM. Prophylactic oral dextrose gel for newborn babies at risk of neonatal hypoglycaemia: a randomised controlled dose-finding trial (the Pre-hPOD Study). PLoS Med. 2016;13:e1002155.
Walravens C, Gupta A, Cohen RS, Kim JL, Frymoyer A. Fewer glucose checks and decreased supplementation using dextrose gel for asymptomatic neonatal hypoglycemia. J Perinatol 2023;43:532–37.
Parappil H, Gaffari M, Ahmed J, Skaria S, Rijims M, Chandra P, et al. Oral Dextrose gel use in asymptomatic hypoglycemic newborns decreases NICU admissions and parenteral dextrose therapy: A retrospective study. J Neonatal Perinat Med. 2023;16:111–17.
Griffith R, Hegarty JE, Alsweiler JM, Gamble GD, May R, McKinlay CJ, et al. Two-year outcomes after dextrose gel prophylaxis for neonatal hypoglycaemia. Arch Dis Child Fetal Neonatal Ed. 2021;106:278–85.
Meneghin F, Manzalini M, Acunzo M, Daniele I, Bastrenta P, Castoldi F, et al. Management of asymptomatic hypoglycemia with 40% oral dextrose gel in near term at-risk infants to reduce intensive care need and promote breastfeeding. Ital J Pediatr. 2021;47:1–8.
Rawat M, Chandrasekharan P, Turkovich S, Barclay N, Perry K, Schroeder E, et al. Oral Dextrose Gel Reduces the Need for Intravenous Dextrose Therapy in Neonatal Hypoglycemia. Biomed Hub. 2017;1:1–9.
Desai P, Verma S, Bhargava S, Rice M, Tracy J, Bradshaw C. Implementation and outcomes of a standard dose dextrose gel protocol for management of transient neonatal hypoglycemia. J Perinatol 2022;42:1097–02.
Stanzo K, Desai S, Chiruvolu A. Effects of Dextrose Gel in Newborns at Risk for Neonatal Hypoglycemia in a Baby-Friendly Hospital. J Obstet Gynecol Neonatal Nurs 2020;49:55–64.
Gregory K, Turner D, Benjamin CN, Monthe-Dreze C, Johnson L, Hurwitz S, et al. Incorporating dextrose gel and feeding in the treatment of neonatal hypoglycaemia. Arch Dis Child Fetal Neonatal Ed. 2020;105:45–49.
Glasgow MJ, Harding JE, Edlin R, Alsweiler J, Chase JG, Harris D, et al. Cost analysis of treating neonatal hypoglycemia with dextrose gel. J Pediatr. 2018;198:151–55.e1.
Harris DL, Alsweiler JM, Ansell JM, Gamble GD, Thompson B, Wouldes TA, et al. Outcome at 2 years after dextrose gel treatment for neonatal hypoglycemia: follow-up of a randomized trial. J Pediatr. 2016;170:54–59.e2.
Brown LD, Rozance PJ. A sweet addition for the treatment of neonatal hypoglycemia. J Pediatr. 2016;170:10–12.
Funding
The authors did not receive any specific grants from public, commercial, or not-for-profit funding agencies for this research.
Author information
Authors and Affiliations
Contributions
GS and SS: Conceptualization of the study, supervision, initial screening of studies, quality assessment of included studies, statistical analysis, manuscript drafting, and critical review of the manuscript, P K: Validation of results, supervision of screening of studies, quality assessment of included studies, and drafting of the discussion section, critical review and final approval of the manuscript, L P: Data collection, literature review, initial screening of studies, quality assessment of included studies, and drafting of the methodology section, A M: Supervision of data extraction, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sivakumar, G., Kuppusamy, P., P, L.P. et al. Effectiveness of oral dextrose gel for neonates at risk of hypoglycemia: A systematic review, meta-analysis, and GRADE assessment of randomized controlled trials. J Perinatol 45, 1335–1344 (2025). https://doi.org/10.1038/s41372-025-02387-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02387-x