Abstract
Objective
To screen high-risk infants for CP in a level IV NICU and high-risk infant follow-up (HRIF) clinic.
Study Design
By using quality improvement methodology, we implemented the General Movement Assessment (GMA) and Hammersmith Infant Neurological Examination (HINE) to screen for CP and lower age at diagnosis. Main balancing measures included no-show rates.
Results
Within the first year, 89% of infants had a GMA in the NICU, 100% in HRIF and 87% had a HINE in HRIF. Median age at diagnosis decreased from 18.5 months adjusted [16.7,19.4] in 2021 to 7.5 months [5.9,14.4; p = 0.01] in 2022 and 8.9 months [6.6,12.2; p = 0.01] in 2023. No-show rates increased in 2022 compared to 2021 (24% vs 17%, p = 0.02).
Conclusions
By implementing and continuously improving a standard process in the NICU and HRIF, we demonstrated a successful increase in screening for CP leading to a lower age at diagnosis sustained for two years.
Similar content being viewed by others
Introduction
Cerebral palsy (CP) is the most common motor disability of childhood affecting 1 in 345 children in the United States [1,2,3,4]. Underlying mechanisms can be divided into intrauterine, peripartum and postnatal factors, but in more than half of cases the etiology is unknown while advances in genomic testing have uncovered genetic causes of CP in up to 25% of affected people [5,6,7,8,9,10,11,12,13,14].
Historically, CP was considered an unseen handicap, leading to delayed diagnoses, tied to caregiver dissatisfaction [15,16,17,18,19,20,21]. However, earlier diagnosis allows families to proactively engage with providers while promoting interventions that harness the brain’s neuroplasticity [21, 22]. Well-validated screening tools have demonstrated high sensitivity and specificity for CP including the General Movement Assessment (GMA) and the Hammersmith Infant Neurological Examination (HINE), both of which measure different but complementary constructs when combined with neuroimaging and gross motor tests [21, 23,24,25,26,27,28,29,30,31,32]. The GMA is a qualitative assessment first described by Dr. Heinz Prechtl based on visual gestalt of an infant’s spontaneous movements that reflect the integrity of the neural network. He observed two distinct general movement patterns in preterm and term infants [30]:
-
1.
Writhing movements: begin around 36 weeks postmenstrual age and persist until nine weeks adjusted age and are categorized as normal, poor repertoire, chaotic or cramped synchronized.
-
2.
Fidgety movements: begin around seven weeks adjusted and persist until five months adjusted and are categorized as normal, abnormal or absent.
Several studies have demonstrated the predictive value of the GMA as an early screening tool for CP, particularly the trajectory of cramped synchronized movements followed by absent fidgety movements, which are highly predictive of spastic CP [24, 29]. The HINE is a validated neurologic examination that consists of 26 items that evaluate cranial nerves, tone, posture, movements, reflexes and reactions, providing a global optimality score that can be conducted in infants aged two months to two years; serial exams over time can help differentiate transient versus permanent abnormal neurologic findings [23]. Similar to the GMA, multiple studies have demonstrated the HINE’s predictive value for CP and ability to provide diagnostic and potentially prognostic information in this population [33, 34].
Evidence-based clinical guidelines in 2017 advocated for early CP detection to provide timely support for families, improve access to services and facilitate earlier interventions [21]. These guidelines incorporate tools traditionally used such as imaging and gross motor assessments but not all institutions have adopted use of the GMA and/or HINE. Although institutions have reported on successful implementation of these tools, use of differing quality improvement (QI) methods applied to heterogenous populations in various settings make it challenging to replicate their findings [35,36,37,38,39]. In our level IV NICU and HRIF clinic serving a majority Medicaid-funded, urban population, we did not have a standardized way to screen for or diagnose CP. Therefore, we utilized a QI framework to implement early detection tools and follow age at diagnosis over time.
Methods
Context
This initiative was carried out from January 2022 to December 2023 in a level IV NICU and HRIF clinic. Our NICU serves a wide catchment area across New York extending to New Jersey and Connecticut and admits an average of 1100 infants annually. About 90% are inborn with an annual average of 165 infants born less than 32 weeks and about 12 infants with hypoxic-ischemic encephalopathy (HIE) who receive therapeutic hypothermia admitted each year. Our 17-bed infant cardiac NICU admits on average 110 infants annually. Both units are staffed by about 25 neonatologists, 15 neonatal-perinatal fellows, 50 advanced practice providers, 250 registered nurses, physical therapists (PT) and occupational therapists (OT) and pediatric residents.
The HRIF clinic follows infants born less than 29 weeks, very low birth weight, or if they have any neural insult or complex condition (e.g., congenital diaphragmatic hernia, hypoplastic left heart syndrome). About 98% of referrals are internal. During this initiative, the HRIF team was composed of neonatologists, a nurse practitioner, developmental-behavioral pediatrician, developmental psychologist, physical therapist and coordinator. Before 2021, either the coordinator contacted families of infants who qualified if a referral was placed in the NICU, or the parents contacted the clinic to make an appointment. However, many patients were missed because there was no formal referral process at NICU discharge. Infants were seen at six months (adjusted) and followed every six months until 30–36 months and underwent a Bayley Scales of Infant and Toddler Development Screening Test at the first visit followed by the Bayley-Third Edition in 2021 and Fourth Edition starting in 2022 or the Developmental Assessment of Young Children Second Edition if conducted over telehealth. The provider conducted a history and physical exam. No guidelines existed regarding when to consider a CP diagnosis.
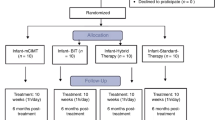
Interventions
After joining the Cerebral Palsy Foundation Early Detection and Intervention Network consisting of seven other NICUs and HRIF programs at the time across the United States in December 2021, we created a local team composed of HRIF providers, PT/OT representatives, and an early detection coordinator. During the pre-implementation phase, we performed a review of infants seen in 2021, including 227 visits, with five infants diagnosed with CP. Over one year, our primary aim was to standardize screening practices including the GMA and HINE from a baseline of 0% to a goal of 100% in infants who qualified for HRIF while our outcome was age at CP diagnosis. We focused on key drivers and interventions shown in Fig. 1 with steps delineated in Table 1.
Phase 1: Provider training, operational work-flow changes and education
All HRIF providers and inpatient PTs and OTs underwent HINE training by the Cerebral Palsy Foundation in March 2022 followed by the basic GMA course in August 2022. Starting in July 2022, we routinely administered the Alberta Infant Motor Scale (AIMS) as our standardized motor assessment given ease of administration in-person or via telehealth. We shifted to an earlier clinic visit at three to four months (adjusted) to capture a fidgety period GMA and saw patients every six months until 30–36 months. The number of visits remained the same except for an extra visit at six months (adjusted) reserved for infants designated high-risk for CP (HRCP), those with a low HINE score, or to follow-up other concerns. Infants were considered HRCP if they had a clinical risk factor for CP and at least two of the following: atypical GMA findings (e.g., absent fidgety movements), low HINE scores, gross motor impairment, neuroimaging associated with CP, and/or an established genetic biomarker associated with CP. A diagnosis of CP was considered in high-risk infants if all elements were present or if longitudinal assessments demonstrated continued impairment as evidenced by persistent gross motor delay and HINE scores below age-expected scores even in the setting of a normal GMA [21].
Phase 2: Integration of tools into standard clinical practice
Prior to starting the GMA, process flowcharts were created (Supplementary Figure 1). An early detection coordinator screened the census weekly and identified eligible infants. In the NICU, the therapist team obtained consent to film the video. Videos were recorded using an iPad, uploaded into a protected hospital server, interpreted by two therapists, with results documented in the medical record. The writhing period GMA was done at term-equivalent age or before discharge—whichever came first. Cramped synchronized (CS) results were reported directly to the NICU team, and a family meeting was coordinated to discuss recommendations to obtain a brain MRI and provide education on HRIF and early intervention. Of note, term equivalent brain MRIs were not routinely conducted on all preterm infants and were done on a case-to-case basis at the discretion of the attending neonatologist. Reasons to defer a GMA included high dose sedative/analgesic medications, significant respiratory support or hemodynamic instability, recent abdominal or thoracic procedures or parent refusal. In HRIF, consent was obtained, and a fidgety period GMA was recorded. Storage and documentation of results were identical to the inpatient workflow and interpretation took place in real-time. Starting in July 2021, a PT in HRIF administered the HINE during two half-day sessions per week. Following HINE training in March 2022, all providers administered the HINE to all infants in HRIF.
Diagnostic criteria for CP were based on review of evidence-based guidelines of infants with a newborn-attributable risk factor [21]. If an infant had absent fidgety movements, a HINE score beneath an age-expected cut-off score (e.g., <57 at 3 months or <63 at 6–12 months), gross motor impairment, and neuroimaging associated with CP, then a diagnosis was considered [21]. In infants with normal GMA findings but persistently low HINE scores, providers considered referral for neuro-imaging if not done. In infants with normal imaging but abnormal HINE and gross motor findings, providers considered referral to the CP center or making a diagnosis based on clinical judgement.
Phase 3: Sustainability
Next, we focused on establishing a sustainable process that began with standardizing documentation and communication. Flowsheets (Supplemental Fig. 2) were created in the medical record for the HINE, GMA and AIMS, allowing results to be automatically incorporated into notes by July 2023. To build inter-rater reliability, GMA review sessions were held bimonthly. In November 2023, the neonatology division approved clinical practice guidelines delineating a GMA workflow. In the fall of 2023, clinical criteria to consider a diagnosis of CP or a HRCP were re-visited and a checklist was created. Lastly, infants diagnosed with CP were referred to our institution’s CP center for establishment of care.
Measures
Our primary measure was number of qualifying infants screened for CP, which was tracked as the ratio of infants who underwent a GMA and/or HINE from 2022 to 2023 to all qualifying infants. This was chosen because infants with CP in 2021 were diagnosed by another specialist despite being followed by HRIF while a quarter of patients were seen via telehealth, limiting the ability to make a diagnosis. Our primary outcome was median age at CP diagnosis. Other measures collected included the number of infants diagnosed with CP or designated HRCP, patient demographic and clinical characteristics. Measures and age at diagnosis were evaluated quarterly. Balancing measures included no-show rates and number of infants referred because of clinical concern outside of HRIF criteria in order to determine if adding one more visit for a subgroup of infants in three months led to higher no-show rates or if adding another tool in the NICU over-identified infants referred to HRIF.
Analysis
To demonstrate change over time, we tracked the ratio of qualifying infants who had a GMA in the NICU and/or HRIF, and HINE in HRIF monthly using p charts. Fisher’s exact test or ANOVA testing were used to compare patient characteristics from 2021 to 2023. To compare the median adjusted age at CP diagnosis over time, we performed a Dunn’s pairwise nonparametric test using median age in 2021 as the baseline and created a run chart to track age at diagnosis. Analyses were conducted using QI Macros or R software (R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Ethical considerations
The project was not considered human subjects research by the Institutional Research Board at Columbia University Medical Center and therefore did not require review or approval from our local IRB. We adhered to all QI ethical guidelines in the planning and execution of this project. No interventions, therapies, or subjects were randomized. The study team accessed all charts and reported deidentified data to the Cerebral Palsy Foundation in the form of quarterly reports that were tracked alongside the other sites part of the CP Early Detection and Intervention Network. No personal health information was shared outside of the institution.
Results
GMA and HINE screening and age at diagnosis
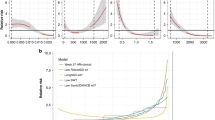
Providers routinely administered the HINE in HRIF in March 2022, and started seeing patients at three months in August 2022 with the introduction of the fidgety period GMA. The inpatient PT/OT team started conducting the GMA in the NICU in September 2022. Within five months, there was a significant change in the centerline for the ratio of qualifying infants who had a GMA in the NICU in the fall of 2022 maintained for the next ten months (Fig. 2A). In December 2023, there was one data point below the lower control limit, which was attributed to having limited personnel available during a holiday season. The most common reason cited for missing a GMA was inability to capture infants discharged earlier than 36 weeks. In HRIF, with initiation of a three-month visit, 100% of qualifying infants underwent a GMA by April 2023 (Fig. 2B). Three caregivers refused the GMA in the NICU and HRIF over two years. Five months after HINE training, there was a significant increase in the number of infants with a HINE starting in August 2022 that was sustained through December 2023 (Fig. 2C). The most common reason for not completing a HINE was inability to administer due to infant’s state.
The median adjusted age at CP diagnosis was significantly lower at 7.5 months [5.9,14.4; p = 0.02] in 2022 and 8.9 months [6.6,12.2; p = 0.01] in 2023 compared to 18.5 months in 2021 [16.7,19.4]. After hiring an early detection coordinator, introducing the HINE and joining a network, there was a trend towards a lower age at diagnosis by the first quarter of 2022 followed by a shift noted from the third quarter of 2022 to the second quarter of 2023 following the initiation of a three-month visit (Fig. 3).
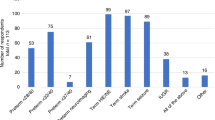
Secondary process metrics and balancing measures
The number of clinic visits more than doubled from 2021 to 2023 (Supplementary Table), and the number of new CP diagnoses increased (Table 2). Eight brain MRIs were done in the NICU in infants who had CS movements: two with high-grade intraventricular hemorrhage, two with low grade intraventricular hemorrhage, one with white matter injury, one with a neuronal migration disorder, one with ventriculomegaly, and one that had a normal term equivalent MRI. Two infants with CS movements and normal cranial ultrasounds (cUS) did not have an MRI for unclear reasons. Two infants who did not meet criteria for HRIF were referred due to abnormal movements observed. No-show rates significantly increased from 17% in 2021 to 24% in 2022 (p = 0.02) but subsequently decreased in 2023 to 22% (p = 0.09).
Characterization of infants diagnosed with CP
Five infants were diagnosed with CP in 2021, and 10 infants were diagnosed in 2022—all of whom were premature. In 2023, 4 out of the 11 infants (36%) diagnosed with CP had HIE and received therapeutic hypothermia (Table 2). Among infants diagnosed with CP from 2022 to 2023, most (21/26, 81%) had neuroimaging findings on either a cUS or MRI correlated with CP while four (15%) had a normal cUS but no MRI to review and one (4%) had a normal cUS and MRI at term equivalent age. More infants with CP had absence of fidgety movements but did not have CS movements during the writhing period. Further characteristics and demographics of infants diagnosed with CP are shown in Table 2.
Discussion
In a level IV NICU and HRIF clinic, we demonstrated successful implementation of an early CP detection initiative utilizing evidence-based screening tools in high-risk infants. The ratio of qualifying infants who underwent a GMA increased from 0% to 89% in the NICU and 100% at the first HRIF visit. In HRIF, 87% infants had a HINE done visit during the latter half of the initiative. Our efforts led to a sustained reduction in the age at CP diagnosis from 18.5 months to below nine months sustained for two years after hiring an early detection coordinator, joining a collaborative effort, and initiating an earlier HRIF visit [40]. The largest study to date involving five HRIF programs reported an average age at diagnosis of 9.5 months decreased from 19.5 months sustained for five years [36]. Similarly, a key component in our study was standardization of a three-month visit, allowing for earlier establishment of care and a fidgety period GMA, which is more sensitive and specific for CP compared to the writhing period GMA [21]. Of infants who had a GMA, 4.2% (10/240) had CS movements and 6.3% (11/176) had absent fidgety movements, which was less frequent compared to previous groups reporting 6.5% (63/965) and 10.2% (144/1414) respectively in recent publications [37]. In our cohort, clinically significant MRI findings were detected in 62.5% (5/8) of infants with CS movements higher than 52% of a recent cohort of 144 infants [41]. In our cohort, only five additional MRIs were done in response to GMA findings over two years—all but one had abnormalities not captured on cUS while one had a normal MRI and was ultimately designated HRCP [42].
Through outreach efforts and improvements to the referral process, the number of infants seen in HRIF increased by 2.7-fold with a CP prevalence ranging from 3-3.7% from 2021 to 2023, lower than those previously reported [38, 43]. We postulated this may be due to our referral criteria recently broadened in 2023 to include all very low birth weight infants and a higher follow-up rate at the three-month visit that was sustained at older ages.
Most new diagnoses were among term infants with HIE in 2023 compared to the previous years, but the sample size was variable. Most infants with HIE were diagnosed with CP earlier than six months, particularly after the GMA and HINE were administered. This difference in distribution in 2023 may be due to improved follow-up of infants with HIE. In 2021 33% (4/12) of infants with HIE were seen in HRIF, which improved to 60% (12/20) in 2022 and 80% (4/5) in 2023. The larger sample size in 2022 and improved follow-up may have skewed our distribution of diagnoses in 2023 away from preterm infants who continue to have an increasing prevalence of CP across the country [6, 44]. Larger scale longitudinal studies are needed to clarify the contributions of different risk factors to CP. Additionally, diagnostic variability continues to exist [45]. Four infants in our cohort were diagnosed with hypotonic CP at older ages—one with a chromosomal deletion, two with periventricular leukomalacia, and a growth restricted preterm infant with a normal brain MRI. Diagnosis was made in collaboration with a CP specialist and led to increase in therapies but highlighted limitations of neuroimaging, which can be normal in up to 15% of infants with CP [46, 47]. Additionally, a genetics evaluation was considered in light of recent work that has uncovered new genes implicated in the development of CP in both individuals with and without known risk factors [5, 48].
Privacy was a major concern considered when establishing a GMA workflow, which was a barrier that our institution encountered [49]. Video recordings were stored in a HIPAA-compliant, cloud-based storage. Initially, our institution’s Office of Legal Affairs required consent for the GMA but in January 2024, they acknowledged the GMA as a standard tool and determined that formal consent was no longer required. Further strategies have been explored, including use of a phone application that allows parents to film a GMA securely, while others are researching use of automated assessment of general movements [50, 51].
Previous studies have reported an overall positive parental perception of early diagnosis and use of a HRCP designation among caregivers [17, 18, 52]. Furthermore, a consensus statement advocated that a HRCP designation be considered if one element was missing or normal [52]. Starting in the fall of 2022 we adopted a modified use of a HRCP designation and found that 7/11 (64%) of those diagnosed in 2023 had been designated HRCP. We collaborated with the Cerebral Palsy Foundation and created a checklist to guide when to consider a HRCP designation and/or conversion to a diagnosis [16]. In a recent qualitative study published by our group, caregivers were not only accepting of early CP diagnoses but also were supportive of the use of a HRCP designation even if their infant did not ultimately develop CP [53].
No-show rates were followed to assess the impact of an earlier visit and potential added six-month visit. Although the no-show rate increased in 2022 compared to 2021 (Supplementary Table) the number of clinic visits more than doubled with a stable no-show rate in 2023. Because no standardized referral system existed prior to 2022 allowing for selection bias, the referral process was re-vamped to include meetings with the coordinator and families in the NICU, one-month telephone check-ins and virtual reminders to ensure equitable follow-up. In 2021, 45% of eligible patients came to their first appointment, increased to 72% in 2022 and 89% in 2023. Among infants who had an additional three-month follow-up, 29% (8/28) were lost to follow-up in 2022, decreased to 14% (10/67) in 2023 following the adoption of a HRCP checklist, which may partly explain the increase in no-show rates in 2022 when criteria were more lenient. Although patients with Medicaid were less likely to be seen compared to those privately insured, there was no difference among the years as well as no difference among English-speaking versus non-English speaking families to account for a further increase in no-show rates [54].
We demonstrated that using a QI framework could successfully lead to implementation of guidelines by using iterative processes to achieve sustainability [55]. Each infant benefitted from a diagnosis in terms of increased therapies—nine (35%) had no prior services, three (12%) were referred to local rehabilitation centers while one with hemiplegic CP was referred to a study evaluating role of constraint-induced movement therapy, which can improve affected hand function [56, 57].
Limitations
This QI initiative occurred at a single large academic referral center in a metropolitan area, which limits the generalizability of these findings. An early detection coordinator was critical in the success of this initiative, which may not be feasible elsewhere; however, achieving buy-in with existing key stakeholders played an important role in leveraging skills and utilization of available resources. Our focus was on capturing infants in the NICU who qualified for HRIF while other institutions have implemented universal GMA screening. Although implementation of early tools should lead to earlier diagnoses, ensuring fidelity and reliability of these tools on a repeated basis is an integral part of this process. Lastly, several members were GMA-trained, which could lead to different interpretations but more than a dozen providers received advanced training, allowing for improved clinical discretion.
Conclusions
In this QI initiative, we demonstrated successful implementation of evidence-based screening tools (e.g., GMA, HINE) conducted in high-risk infants in our NICU and HRIF clinic sustained over time with a subsequent lower age at CP diagnosis. Continued education, demonstration of successful implementation efforts and standardization of elements essential for a diagnosis are feasible with the support of a committed team.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Maenner MJ, Blumberg SJ, Kogan MD, Christensen D, Yeargin-Allsopp M, Schieve LA. Prevalence of cerebral palsy and intellectual disability among children identified in two U.S. National Surveys, 2011–2013. Ann Epidemiol. 2016;26:222–6.
Durkin MS, Benedict RE, Christensen D, Dubois LA, Fitzgerald RT, Kirby RS, et al. Prevalence of cerebral palsy among 8-year-old children in 2010 and preliminary evidence of trends in its relationship to low birthweight. Paediatr Perinat Epidemiol. 2016;30:496–510.
Bax MC. Terminology and classification of cerebral palsy. Dev Med Child Neurol. 1964;6:295–7.
Novak I, Hines M, Goldsmith S, Barclay R. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics 2012;130:e1285–312.
Gonzalez-Mantilla PJ, Hu Y, Myers SM, Finucane BM, Ledbetter DH, Martin CL, et al. Diagnostic yield of exome sequencing in cerebral palsy and implications for genetic testing guidelines: a systematic review and meta-analysis. JAMA Pediatr. 2023;177:472–8.
Graham HK, Rosenbaum P, Paneth N, et al. Cerebral palsy. Nat Rev Dis Prim. 2016;2:15082.
Benninger KL, Purnell J, Conroy S, Jackson K, Batterson N, Neel ML, et al. Intrauterine drug exposure as a risk factor for cerebral palsy. Dev Med Child Neurol. 2022;64:453–61.
Stavsky M, Mor O, Mastrolia SA, Greenbaum S, Than NG, Erez O. Cerebral palsy—Trends in epidemiology and recent development in prenatal mechanisms of disease, treatment, and prevention. Front Pediatr. 2017;5:21.
Rankin J, Cans C, Garne E, Colver A, Dolk H, Uldall P, et al. Congenital anomalies in children with cerebral palsy: a population‐based record linkage study. Dev Med Child Neurol. 2010;52:345–51.
Grunt S, Mazenauer L, Buerki SE, Boltshauser E, Capone Mori A, Datta AN, et al. Incidence and outcomes of symptomatic neonatal arterial ischemic stroke. Pediatrics 2015;135:e1220–8.
Himpens E, Van Den Broeck C, Oostra A, Calders P, Vanhaesebrouck P. Prevalence, type, distribution, and severity of cerebral palsy in relation to gestational age: a meta-analytic review. Dev Med Child Neurol. 2008;50:334–40.
Rouabhi A, Husein N, Dewey D, Letourneau N, Daboval T, Oskoui M, et al. Development of a bedside tool to predict the diagnosis of cerebral palsy in term-born neonates. JAMA Pediatr. 2023;177:177–86.
Jin SC, Lewis SA, Bakhtiari S, Zeng X, Sierant MC, Shetty S, et al. Mutations disrupting neuritogenesis genes confer risk for cerebral palsy. Nat Genet. 2020;52:1046–56.
Wang Y, Xu Y, Zhou C, Cheng Y, Qiao N, Shang Q, et al. Exome sequencing reveals genetic heterogeneity and clinically actionable findings in children with cerebral palsy. Nat Med. 2024;30:1395–405.
McIntyre S, Morgan C, Walker K, Novak I. Cerebral palsy-don’t delay. Dev Disabil Res Rev. 2011;17:114–29.
Kim F, Maitre N. Cerebral Palsy Foundation. A call for early detection of cerebral palsy. NeoReviews. 2024;25:e1–11.
Baird G, McConachie H, Scrutton D. Parents’ perceptions of disclosure of the diagnosis of cerebral palsy. Arch Dis Child. 2000;83:475–80.
Byrne R, Duncan A, Pickar T, Burkhardt S, Boyd RN, Neel ML, et al. Comparing parent and provider priorities in discussions of early detection and intervention for infants with and at risk of cerebral palsy. Child Care Health Dev. 2019;45:799–807.
Velde A, Morgan C, Novak I, Tantsis E, Badawi N. Early diagnosis and classification of cerebral palsy: An historical perspective and barriers to an early diagnosis. J Clin Med. 2019;8:1599.
Hubermann L, Boychuck Z, Shevell M, Majnemer A. Age at referral of children for initial diagnosis of cerebral palsy and rehabilitation: current practices. J Child Neurol. 2016;31:364–9.
Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017;171:897–907.
Morgan C, Darrah J, Gordon AM, Harbourne R, Spittle A, Johnson R, et al. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev Med Child Neurol. 2016;58:900–9.
Haataja L, Mercuri E, Regev R, Cowan F, Rutherford M, Dubowitz V, et al. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J Pediatr. 1999;135:153–61.
Bosanquet M, Copeland L, Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Dev Med Child Neurol. 2013;55:418–26.
Morgan C, Romeo DM, Chorna O, Novak I, Galea C, Del Secco S, et al. The pooled diagnostic accuracy of neuroimaging, general movements, and neurological examination for diagnosing cerebral palsy early in high-risk infants: A case control study. J Clin Med. 2019;8:1879.
Støen R, Boswell L, de Regnier RA, Fjørtoft T, Gaebler-Spira D, Ihlen E, et al. The predictive accuracy of the general movement assessment for cerebral palsy: A prospective, observational study of high-risk infants in a clinical follow-up setting. J Clin Med. 2019;8:1790.
Kwong AKL, Boyd RN, Chatfield MD, Ware RS, Colditz PB, George JM. Early motor repertoire of very preterm infants and relationships with 2-year neurodevelopment. J Clin Med. 2022;11:1833.
Romeo DMM, Cioni M, Palermo F, Cilauro S, Romeo MG. Neurological assessment in infants discharged from a neonatal intensive care unit. Eur J Paediatr Neurol. 2013;17:192–8.
Prechtl HF, Einspieler C, Cioni G, Bos AF, Ferrari F, Sontheimer D. An early marker for neurological deficits after perinatal brain lesions. Lancet. 1997;349:1361–3.
Einspieler C, Prechtl HF. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev. 2005;11:61–7.
Prechtl HF. Qualitative changes of spontaneous movements in fetus and preterm infant are a marker of neurological dysfunction. Early Hum Dev. 1990;23:151–8.
Maitre NL, Chorna O, Romeo DM, Guzzetta A. Implementation of the Hammersmith Infant Neurological Examination in a high-risk infant follow-up program. Pediatr Neurol. 2016;65:31–8.
Hay K, Nelin M, Carey H, Chorna O, Moore-Clingenpeel M, Naitre N, et al. Hammersmith Infant Neurological Examination asymmetry score distinguishes hemiplegic cerebral palsy from typical development. Pediatr Neurol. 2018;87:70–4.
Romeo DM, Ricci D, Brogna C, Mercuri E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Dev Med Child Neurol. 2016;58:240–5.
Byrne R, Noritz G, Maitre NL, NCH Early Developmental Group. Implementation of early diagnosis and intervention guidelines for cerebral palsy in a high-risk infant follow-up clinic. Pediatr Neurol. 2017;76:66–71.
Maitre NL, Damiano D, Byrne R. Implementation of early detection and intervention for cerebral palsy in high-risk infant follow-up programs. Clin Perinatol. 2023;50:269–79.
Maitre NL, Burton VJ, Duncan AF, Iyer S, Ostrander B, Winter S, et al. Network implementation of guideline for early detection decreases age at cerebral palsy diagnosis. Pediatrics 2020;145:e20192126.
Razak A, Johnston E, Sackett V, Clark M, Charlton M, Zhou L, et al. Early neurodevelopmental assessments for predicting long-term outcomes in infants at high risk of cerebral palsy. JAMA Netw Open. 2024;7:e2413550.
King AR, Al Imam MH, McIntyre S, Morgan C, Khandaker G, Badawi N, et al. Early diagnosis of cerebral palsy in low- and middle-income countries. Brain Sci. 2022;12:539.
Quality Improvement Essentials Toolkit. Boston: Institute for Healthcare Improvement; 2017. (Available at ihi.org).
Chirigos AJ, Ostrander B, Burton VJ, Mirecki M, Maitre NL. Cerebral Palsy Foundation Early Detection and Intervention Network. Prechtl’s general movements assessment at writhing age guides MRI use in clinical implementation network. Pediatr Res. 2024;95:1188–90.
Ho T, Dukhovny D, Zupancic JAF, Goldmann DA, Horbar JD, Pursley DM. Choosing Wisely in Newborn Medicine: Five Opportunities to Increase Value. Pediatrics 2015;136:e482–9.
King AR, Machipisa C, Finlayson F, Fahey MC, Novak I, Malhotra A. Early detection of cerebral palsy in high‐risk infants: translation of evidence into practice in an Australian hospital. J Paediatr Child Health. 2021;57:246–50.
DeMauro SB, McDonald SA, Heyne RJ, Vohr BR, Duncan AF, Newman JE, et al. Increasing prevalence of cerebral palsy among two-year-old children born at <27 weeks of gestation: a cohort study. J Pediatr. 2024;268:113944.
Aravamuthan BR, Fehlings D, Shetty S, Fahey M, Gilbert L, Tilton A, et al. Variability in cerebral palsy diagnosis. Pediatrics 2021;147:e2020010066.
Bax M, Tydeman C, Flodmark O. Clinical and MRI correlates of cerebral palsy: the European cerebral palsy study. JAMA 2006;296:1602–8.
Towsley K, Shevell MI, Dagenais L. Population-based study of neuroimaging findings in children with cerebral palsy. Eur J Paediatr Neurol. 2011;15:29–35.
Van Eyk CL, Fahey MC, Gecz J. Redefining cerebral palsies as a diverse group of neurodevelopmental disorders with genetic aetiology. Nat Rev Neurol. 2023;19:542–55.
Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. 2021;22:122.
Spittle A, Olsen J, Kwong A, Doyle LW, Marschik PB, Einspieler C, et al. The Baby Moves prospective cohort study protocol: using a smartphone application with the General Movements Assessment to predict neurodevelopmental outcomes at age 2 years for extremely preterm or extremely low birthweight infants. BMJ Open. 2016;6:e013446.
Gao Q, Yao S, Tian Y, Zhang C, Zhao T, Wu D, et al. Automating general movements assessment with quantitative deep learning to facilitate early screening of cerebral palsy. Nat Commun. 2023;14:8294.
Maitre NL, Byrne R, Duncan A, Dusing S, Gaebler-Spira D, Rosenbaum P, et al. “High-risk for cerebral palsy” designation: A clinical consensus statement. J Pediatr Rehabil Med. 2022;15:165–74.
Kim F, Ryder S, Marin A, Zygmunt A, Guttmann K. Caregiver perceptions of communication about early cerebral palsy or high-risk designation in infants. JAMA Netw Open. 2025;8:e2519421.
Lakshmanan A, Rogers EE, Lu T, Gray E, Vernon L, Briscoe H, et al. Disparities and early engagement associated with the 18- to 36-month high-risk infant follow-up visit among very low birthweight infants in California. J Pediatr. 2022;248:30–8.e3.
Bapat R, Pearlman S. The role of QI collaboratives in neonatology. J Perinatol. 2024;45:417–25.
Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, Hines A, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep. 2020;20:3.
Eliasson AC, Sjöstrand L, Ek L, Krumlinde-Sundholm L, Tedroff K. Efficacy of baby-CIMT: study protocol for a randomised controlled trial on infants below age 12 months, with clinical signs of unilateral CP. BMC Pediatr. 2014;14:141.
Acknowledgements
We would like to acknowledge the pediatric physical and occupational therapists at NewYork-Presbyterian Morgan Stanley Children’s Hospital for their continued dedication to providing excellent developmental care in the NICU. We wish to acknowledge Dr. Nathalie Maitre, Rachel Byrne, Rebecca Lam, the Cerebral Palsy Foundation and network implementation sites for their continued guidance throughout the implementation process. We also wish to acknowledge Lynn Kim, Christopher Chang and Robert Casanova for providing expertise in quality improvement methodology and to Vivian Yuan for her biostatistical support. Lastly, we thank the families of infants who we care for both in the NICU and HRIF clinic.
Funding
Drs. Faith Kim (principal investigator) and Sylvan Ryder (early detection coordinator) received support from the Cerebral Palsy Foundation Early Detection Initiative that was awarded to Dr. Anna Penn. This work (in part) was supported by Columbia University Department of Pediatrics Innovation Nucleation Fund awarded to Dr. Faith Kim.
Author information
Authors and Affiliations
Contributions
FK and SR conceptualized and designed the study, drafted the initial manuscript, collected data, and critically reviewed and revised the manuscript. MK collected data, drafted the initial manuscript and critically reviewed and revised the manuscript. SB carried out initial analyses and critically reviewed and revised the manuscript. SO, PR and JW helped to collect data and critically reviewed and revised the manuscript. AA, KB, JH, GP, AZ, LY, AP critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ryder, S., Kerner-Rossi, M., Brachio, S. et al. Standardizing early cerebral palsy detection in high-risk infants: reducing age at diagnosis through a quality improvement initiative. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02412-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02412-z